More than 20% of healthcare-associated infections correspond to those at surgical sites, and there is a higher incidence of infections in colorectal surgery due to the associated bacterial load. Surgical wound protectors are designed to prevent contamination and mechanical trauma. Our aim was to demonstrate the usefulness of a circumferential wound retractor/protector for the prevention of surgical site infections (SSIs) in emergency colorectal surgery.
MethodsForty-one patients that underwent emergency open surgery at a tertiary care hospital were randomized into 2 groups: 20 cases without the retractor (group A) and 21 cases with the retractor (group B). Subjects were assigned to a group in a 1:1 randomization allocation ratio. The chi-square and Fisher's exact tests were employed for the quantitative variables, and the statistical analysis was performed using the IBM Statistical Package for the Social Sciences software for Mac, version 16.0 (IBM SPSS Inc., Chicago, IL, USA).
ResultsThe SSI rate was 17%. Six group A patients developed SSI versus one group B patient. The use of a circumferential wound retractor/protector was statistically significant for the prevention of surgical wound infections, with a p = 0.031 and an OR of 8.5. In addition, preoperative blood glucose levels below 200 mg/dl provided a 3.2-times higher protective effect, compared with glucose levels above 200 mg/dl.
ConclusionsIn the present prospective randomized pilot study, the use of the circumferential wound retractor/protector significantly decreased the likelihood of surgical wound infection in emergency colorectal surgery.
Más del 20% de las infecciones asociadas al cuidado de la salud aparecen en sitios quirúrgicos y la prevalencia es mayor en los procedimientos colorrectales debido a la carga bacteriana asociada. El empleo de separadores de herida está enfocado en evitar la contaminación y el trauma mecánico. Nuestro objetivo fue demostrar la utilidad de un separador/protector circunferencial para evitar las infecciones de sitio quirúrgico (ISQ) en pacientes sometidos a cirugía colorrectal de urgencia.
MétodosSe incluyó a cuarenta y un pacientes atendidos en un hospital de tercer nivel. Los pacientes fueron atendidos con cirugía de urgencia y fueron divididos aleatoriamente en dos grupos: 20 casos sin utilizar el separador (grupo A) y 21 casos utilizándolo (grupo B). La aleatorización se realizó 1:1 de manera consecutiva y el análisis estadístico se hizo mediante prueba exacta de Fisher y chi cuadrada, con el software IBM Statistical Package for the Social Sciences, versión 16.0 para Mac (IBM SPSS Inc., Chicago, IL, USA).
ResultadosLa tasa de ISQ fue de 17%. Seis afectados pertenecían al Grupo A y sólo 1 al Grupo B. El uso del separador/protector circunferencial mostró una diferencia estadísticamente significativa para la prevención de ISQ con una p = 0.031 (OR de 8.5). Además, una glicemia perioperatoria por debajo de 200 mg/dl tiene un efecto protector de 3.2 veces en comparación con niveles por arriba de 200 mg/dl.
ConclusionesEl uso del separador/protector circunferencial demostró una reducción en la incidencia de infección de sitio quirúrgico (ISQ) en los casos de cirugía colorrectal de urgencia en el presente estudio.
Nosocomial infections are a serious public health concern, especially in secondary and tertiary care centers, at which elective and emergency surgical procedures are frequently performed. Said infections not only raise morbidity and mortality rates, but also medical care costs.
Over time, and together with the commitment of health professionals to reduce the incidence of surgical site infections (SSIs), the use of a wound edge protector to minimize surgical field contamination has been re-evaluated. The circumferential wound protector and retractor is a physical barrier that consists of 2 rigid rings joined by a polyurethane cylinder. It is placed by putting one ring inside the cavity and rolling the other ring down toward the edges of the wound, achieving adequate working area exposure. The device’s design provides 360º atraumatic retraction that makes the use of other instruments unnecessary, as well as preventing the tissue from coming into contact with the contents of the abdominal cavity.1
The aim of the present pilot study was to reaffirm the usefulness of this type of retractor to prevent SSI within 30 days after emergency colorectal surgery.
Materials and methodsA prospective, randomized, double-blind study was conducted at a tertiary care referral center in Mexico City, within the time frame of March 2014 and March 2015. All the retractors were donated by the Applied Medical company. Sample size was limited to the number of devices available, with a total of 41 patients enrolled.
The patients were divided into 2 groups: 20 that underwent surgery without the protector/retractor (group A) and 21 that underwent surgery with the use of the device (group B). The patients were progressively assigned into each group through a 1:1 randomization allocation ratio.
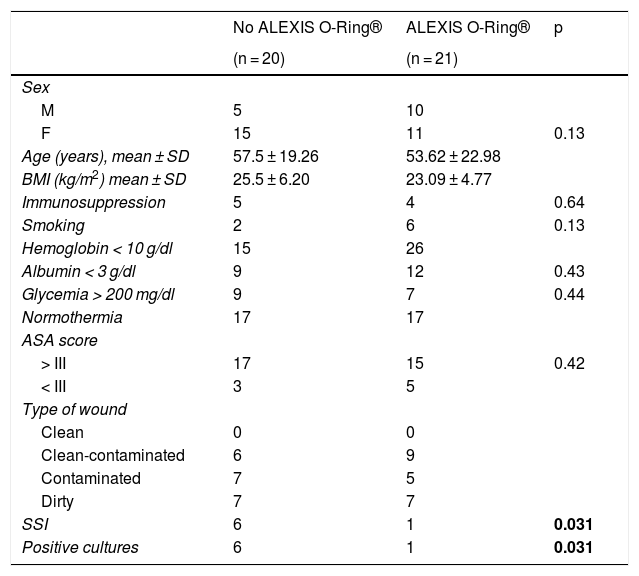
The variables studied were: age, sex, body mass index, immunosuppression, drug addiction (smoking), ASA classification, hemoglobin level, platelet count, albumin, blood glucose, and body temperature. The demographic characteristics were similar for both groups (Table 1).
Population characteristics.
| No ALEXIS O-Ring® | ALEXIS O-Ring® | p | |
|---|---|---|---|
| (n = 20) | (n = 21) | ||
| Sex | |||
| M | 5 | 10 | |
| F | 15 | 11 | 0.13 |
| Age (years), mean ± SD | 57.5 ± 19.26 | 53.62 ± 22.98 | |
| BMI (kg/m2) mean ± SD | 25.5 ± 6.20 | 23.09 ± 4.77 | |
| Immunosuppression | 5 | 4 | 0.64 |
| Smoking | 2 | 6 | 0.13 |
| Hemoglobin < 10 g/dl | 15 | 26 | |
| Albumin < 3 g/dl | 9 | 12 | 0.43 |
| Glycemia > 200 mg/dl | 9 | 7 | 0.44 |
| Normothermia | 17 | 17 | |
| ASA score | |||
| > III | 17 | 15 | 0.42 |
| < III | 3 | 5 | |
| Type of wound | |||
| Clean | 0 | 0 | |
| Clean-contaminated | 6 | 9 | |
| Contaminated | 7 | 5 | |
| Dirty | 7 | 7 | |
| SSI | 6 | 1 | 0.031 |
| Positive cultures | 6 | 1 | 0.031 |
Statistically significant data are in bold face (p ≤ 0.05).
SSI was defined as the presentation of clinical manifestations (erythema, edema, pain and/or purulent material) in the patient and a positive culture for microorganisms. Follow-up was carried out during the entire hospitalization period and 30 days after discharge.
Statistical analysisAll statistical tests were 2-tailed and considered significant with a p value < 0.05. The chi-square test and the Fisher’s exact test were employed for the quantitative variables. The statistical data were collected using the IBM Statistical Package for the Social Sciences, version 16.0, software for Mac (IBM SPSS Inc., Chicago, IL, USA).
ResultsA total of 63.4% of the study patients were women. The mean age and body mass index of the group A patients were 57.5 ± 19.26 years and 25.5 ± 6.20 kg/m2, respectively, and they were 53.62 ± 22.98 years and 23.09 ± 4.77 kg/m2 for the group B patients. Nine patients were considered immunosuppressed due to chronic steroid use or chemotherapy and none of them developed wound infection. Blood glucose levels were under 200 mg in 60.9% of the patients, and body temperature was normal in 82.9% (Table 1).
The SSI rate was 17%. According to the surgical wound classification, 39.4% were clean-contaminated wounds, 28.9% were contaminated, and 31.5% were dirty. Finally, 6 group A patients developed SSI versus only one group B patient. All patients received at least one dose of prophylactic antibiotics, but the combination of ceftriaxone (1 g) plus metronidazole (500 mg) was the most prevalent regimen, received by 39% of the population (Table 1).
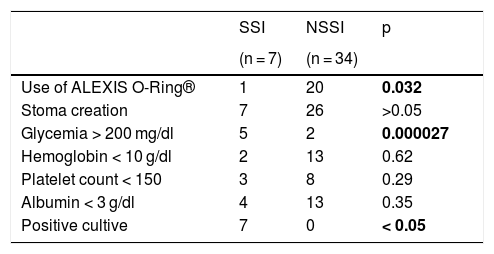
The variables of circumferential wound retractor/protector use and blood glucose yielded statistically significant results. The retractor reduced the risk of SSI with a p value of 0.031 and an OR of 8.5, with a 95% CI of 0.9 to 79.2. Similarly, if the surgical procedure was performed in a patient whose blood glucose level was below 200 mg/dl, the risk of infection decreased 3.2 times (p = 0.000027) (Table 2).
Study variables.
| SSI | NSSI | p | |
|---|---|---|---|
| (n = 7) | (n = 34) | ||
| Use of ALEXIS O-Ring® | 1 | 20 | 0.032 |
| Stoma creation | 7 | 26 | >0.05 |
| Glycemia > 200 mg/dl | 5 | 2 | 0.000027 |
| Hemoglobin < 10 g/dl | 2 | 13 | 0.62 |
| Platelet count < 150 | 3 | 8 | 0.29 |
| Albumin < 3 g/dl | 4 | 13 | 0.35 |
| Positive cultive | 7 | 0 | < 0.05 |
Statistically significant data are in bold face (p ≤ 0.05).
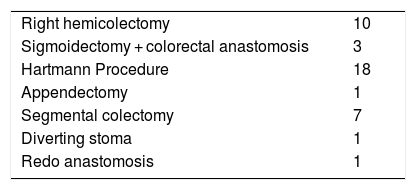
The most widely performed surgical procedure was Hartmann’s procedure secondary to diverticular disease (Hinchey III and IV) (31.7%), followed by right colectomy for miscellaneous reasons (21.9%), and 80.4% of the patients required stoma creation (Table 3).
DiscussionSeveral publications have estimated that 20% of healthcare-associated infections are surgery-related.2 There are multiple risk factors inherent to patients that lead to SSIs, including comorbidities, cigarette smoking, and body mass index, but other risk factors correlate more with the type of surgery and are modifiable.
The US National Nosocomial Infections Surveillance System of the Centers for Disease Control and Prevention introduced the concept of SSI in 1992.3 SSIs could be either incisional or organ/space infections. The former were further subdivided into superficial or deep. Superficial SSIs involve the skin and/or subcutaneous tissue, whereas deep SSIs involve the fascia and muscle layers. Organ/space SSIs correspond to those inside the abdominal cavity. Diagnostic criteria include the outflow of purulent material, a positive culture taken under sterile conditions, and clinical features.4 By definition, all SSIs must occur within 30 days after the procedure.
In colorectal surgery, the incidence of SSI ranges from 5 to 25%.5 Patients with inflammatory bowel disease and those undergoing emergency surgery fall into an important category because those two factors appear to be independent for the development of wound infection.
Currently, standard measures to prevent SSIs include the use of prophylactic antibiotics, trichotomy performance right before the incision, skin preparation with an antiseptic solution, and blood glucose and temperature control during and after surgery. There is controversy as to whether mechanical bowel preparation has a protective effect for SSI or not. Since its introduction in 1970,6 said preparation has been used when so decided by the surgeon, in the majority of cases.
The preoperative combination of oral and intravenous antibiotics, with aerobic and anaerobic coverage, reduces the risk of SSI by 75%,7 regardless of whether the procedure is elective or urgent. However, in an emergency setting, antibiotic administration can be difficult or delayed.
The development of SSIs is multifactorial. However, the emergency surgery setting plays an important and independent role. There is no doubt that prophylactic antibiotics are necessary for SSI prevention, but there is no consensus on the adequate drug regimen to be administered in either elective or emergency surgery, and antibiotic administration is usually delayed in the latter.
Several studies have attempted to demonstrate the effectiveness of wound retractors as a preventive measure for the appearance of infections in elective surgeries. According to findings by Itatsu et al., the implementation of such a barrier is an independent protective factor when employed for elective open gastrointestinal surgeries. The infection rate in their cohort of 1,022 patients was only 9% (p = 0.038, OR 0.73, 95% CI 0.55-0.98).8 On the other hand, in the prospective, observational study by Williams et al., 2 groups undergoing elective gastrointestinal surgery - one group with Vi-Drape® wound protector placement and one group without it - were compared. The incidence of SSI in the entire series was low (12%), resulting in no significant difference for the prevention of SSI with the use of the device.9 The tendency in the literature is to support the use of a wound retractor, but a consensus has yet to be reached.
One of the studies supporting the use of the circumferential wound retractor/protector in colorectal emergency surgery was conducted by Horiuchi et al. Their analysis included all the protective qualities of the retractor observed in 157 cases. There was a decrease in superficial incisional SSIs in patients whose abdominal cavity samples yielded positive cultures.7
Numerous studies currently support the use of a single dose of ertapenem as prophylaxis.10 However, it has not become routine practice due to concerns about antimicrobial resistance and the availability and cost of the drug.6 Additional strategies for preventing wound infection include body temperature control, less bleeding, lower blood pressure during surgery, and reduced trauma to adjacent structures.11
Wound protectors are meant to prevent the dissection and mechanical trauma of the abdominal wall. The current design of the circumferential wound retractor is an improvement over the original device developed in early 2000. Made from hypoallergenic material, it is simple to use and reproducible.12 Unlike other designs, the circumferential wound retractor cannot be displaced or dislodged, thanks to its fixation mechanism.
Over time, surgeons have felt more confident in using the circumferential wound retractor/protector, finding that it also has an effect on humidity and temperature preservation.13
The ROSSINI study is an important antecedent for this specific type of wound retractor. It was a randomized multicenter trial that showed no decrease in the infection rate, despite the use of a wound protector. The study only included patients that underwent either elective or urgent laparotomy.9
The introduction of rapid recovery programs for gastrointestinal surgery, both open and laparoscopic, has reduced the length of hospital stay. Therefore, uninfected wounds guarantee early hospital discharges.
A systematic review and meta-analysis by Mijalhevic et al., published in 2015, included 16 randomized controlled trials and a total of 3,600 patients, all of whom had circular wound protector placement. Those authors concluded that retractors were effective in reducing SSIs in open abdominal surgery, compared with standard care.14 In 2 sets of subgroup analyses of 11 randomized controlled trials, the use of wound retractors and previously described standard protection measures were compared. In the meta-analysis of those 11 trials, the benefit of wound retractors was demonstrated.15
Few organizations have issued recommendations regarding the use of wound edge protection devices. The National Institute for Health and Care Excellence (NICE) of the United Kingdom states that wound edge protection devices may reduce SSI rates after open abdominal surgery, but no recommendation is given due to the lack of further high quality evidence.16 In contrast, the guidelines of the Society for Healthcare Epidemiology of America/Infectious Diseases Society of America recommend the use of impervious plastic wound edge protectors for gastrointestinal and biliary tract surgery.12
Ethical considerationsInformed consent was obtained from all participants and the study was submitted to the hospital’s Ethics Committee, registered as: SCI-805-13/13-1. The authors declare that the present article contains no personal information that would allow the identification of any of the participants.
Conflict of interestThe retractors used in the present study were donated by the Applied Medical company at no cost to the patient. The company did not participate in the conception or development of this trial; thus, we declare there is no conflict of interest.
Financial disclosureNo specific grants were received from public sector agencies, the business sector, or non-profit organizations in relation to this study.
Please cite this article as: Salgado-Nesme N, Morales-Cruz M, Navarro-Navarro A, Patiño-Gómez TA, Vergara-Fernández O. Utilidad del separador circunferencial para herida en cirugía colorrectal de urgencia como medida preventiva para infección del sitio quirúrgico. El Alexis O-Ring® y la cirugía de urgencia. Revista de Gastroenterología de México. 2020;85:399–403.