In the evaluation of the patient with esophageal symptoms (dysphagia, heartburn, and noncardiac chest pain), different diagnostic methods, such as endoscopy and esophagogram, are available to us, but the diagnostic yield continues to be limited.1,2 High-resolution esophageal manometry (HREM) was expected to provide additional utility. Despite all these advances, results continue to be modest. For example, in the absence of achalasia, the motility disorders detected through HREM generally do not correlate with the symptoms, or results are normal. A possible explanation is that during HREM, 10 liquid swallows (the customary protocol) are not physiologically sufficient for evaluating esophageal peristalsis.
As a consequence of the insufficient diagnostic yield provided by the 10 liquid swallows during HREM, different researchers have turned to additional techniques, including the use of viscous swallows,3 applesauce,4 and solid foods,5–7 but the results have been variable. Thus, the use of food during HREM continues to be studied.
Over the past decade, researchers, mainly at European centers, have attempted to simplify the food utilized during HREM, as well as to determine its impact on diagnostic yield. In 2014, Sweis et al. used a cheese and onion paste as the solid food, reporting an increase in diagnostic value in patients with gastroesophageal reflux. That study had the limitation of including only 10 controls and 18 patients with reflux.8
In 2015, Wang et al. studied a larger population of 57 controls and 12 patients with persistent symptoms after antireflux surgery. Utilizing a cheese and onion paste, the researchers showed that the solid test meal (STM) increased the diagnostic sensitivity of HREM in symptomatic patients after fundoplication.9
In 2017, two European studies were key in advancing knowledge regarding the solid food challenge during HREM. In the first work, the researchers established normal values of pharyngeal and esophageal contractions in healthy volunteers (n = 72), employing solid food.10 The study results were reproducible and a standard protocol was developed.10,11 In a second publication, those authors specified the diagnostic value of a cheese and onion paste as the solid food (in England), compared with precooked rice (in Switzerland). The results with the two types of food (cheese or rice) were almost identical.12
Based on the abovementioned observations and specifically employing precooked rice, Ang et al. compared the diagnostic utility between the standard test (ST) of 10 liquid swallows versus the STM with rice.11 Distributing the patients into a “study group” of 750 subjects (in England) and a “validation group” of 221 subjects (in Switzerland), those authors showed that, with the STM, more patients were diagnosed with a major motility disorder in the study group (43 vs. 22%, p < 0.0001), as well as in the validation group (33 vs. 22%, p = 0.014). This diagnostic yield was more notable in the patients with dysphagia (67% with the STM vs. 35% with the ST; p < 0.0001). The same advantage was also seen in the patients with reflux (19 vs. 10%). In addition, the utility of the STM was superior to the ST, with respect to symptom reproduction (61% STM vs. 1% ST; p < 0.0001).12
García-Zermeño et al. carried out the first study on STM use in a Latin American population,13 in which they included 25 healthy controls and 93 patients with different esophageal symptoms. They used precooked rice for the STM. The patient was in the vertical position and instructed to eat the rice at a “normal” or “customary” rhythm for a period of 8 min. The findings indicated that the STM modified the manometric diagnosis in 38% of the cases, including 21% more than the conventional protocol. Furthermore, in patients with ineffective motility, there was a reversion to normal peristalsis in 43%. On the other hand, the use of the STM doubled the number of cases of distal spasm of the esophagus and quadrupled the number of cases of jackhammer esophagus.
Interestingly, the majority of the controls (92%) could complete the STM in fewer than 8 min (mean time 7.1 ± 1.29 min), with a mean intake of rice of 166 ± 45 g. In contrast, the patients with motility disorders were not able to complete rice intake in the projected time of 8 min or were able to do so in only 17%–33% of the cases. Difficulty in completing the test was most notable in the patients with absent peristalsis, followed by ineffective motility, esophagogastric junction outflow obstruction, achalasia, and spastic disorders.
Another valuable aspect of the STM is the reproduction of esophageal symptoms. In the report by Ang et al., they pointed out that symptom reproduction during the STM was 61%, compared with only 1% with the conventional protocol.12 However, this was not reported in the Latin American study.
A valuable clinical application of this information is reflected in a recent study on patients with systemic sclerosis. Butikofer et al. evaluated the hypothesis that the STM (with rice) could detect abnormal motility at early stages in patients with systemic sclerosis, as well as predict disease progression.14 In a prospective longitudinal study, 32 patients with established systemic sclerosis, 24 patients with early disease, and 12 patients with “very early” disease (based on the European League Against Rheumatism and the American College of Rheumatology criteria) were compared with 72 healthy volunteers. The patients with systemic sclerosis swallowed less frequently and ate the rice more slowly than the healthy controls. The patients with confirmed systemic sclerosis and early disease, but not the patients with very early disease, had a lower percentage of effective peristalsis, compared with the controls. The number of effective peristaltic contractions per minute (p < 0.0001) and the speed of rice consumption were lower in the patients with systemic sclerosis (p < 0.0001), including the patients with very early disease that had not shown signs of ineffective motility during the HREM. The mortality rate for systemic sclerosis increases when the disease involves cutaneous and visceral injury. Therefore, the authors of that study suggest that patients with systemic sclerosis should be studied through HREM with a STM, given that the resulting findings can contribute to predicting the patients that require early therapeutic intervention.14
Murray et al. recently evaluated a group of patients with nonobstructive dysphagia (n = 93), showing that the STM (with precooked rice) diagnosed patients that had esophageal outflow obstruction undetected through the standard protocol of 10 liquid swallows. In those patients, the STM identified 19 (76%) patients that benefitted from dilation (with a balloon or “Endoflip”). That study was the first to establish, in patients with nonobstructive dysphagia, that the STM enabled the identification of patients with esophagogastric junction outflow obstruction that benefit from therapeutic dilation.15
Other researchers have continued to evaluate different solid foods, to increase the diagnostic yield. For example, Ribolsi et al. utilized a food based on toasted bread with ham that was eaten within a 20-minute period in the seated position. In that study, 23 patients with nonerosive reflux and 15 controls were evaluated. The STM was compared with the use of standard liquid swallows. Those authors found that the swallows with the solid food more commonly revealed motility disorders, compared with the standard liquid swallows.16
Araujo et al. studied 104 patients with dysphagia, comparing the STM and ST. The STM consisted of ingesting 5 swallows of “bread, or a food brought from home that precipitated symptoms”. The STM changed the diagnosis in 31.7% of the patients (including a change from normal or minor motility changes to a major motility disorder in 13.4%). In addition, 29% of the patients reproduced their symptoms during the test.17
In a retrospective study, Sanagapalli et al. showed the benefit of the STM (in this case, they used a combination of rice or 5–10 pieces of bread with butter, measuring one cubic centimeter each). The researchers reported greater diagnostic utility in the challenge test than in the standard swallows for identifying esophagogastric junction outflow obstruction, particularly in patients with clinically relevant obstruction.18
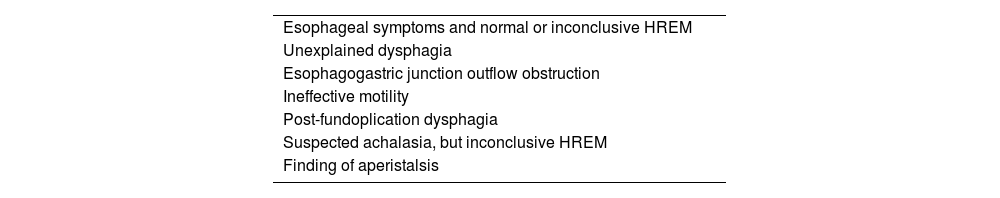
Putting this information in perspective, the use of challenge tests, such as those with rice, helps determine the significance of an inconclusive HREM (Table 1). Some of its indications are: (1) to evaluate patients with esophageal symptoms and normal motility, especially in those with unexplained dysphagia; (2) to determine the clinical significance of esophagogastric junction outflow obstruction (i.e., if the obstruction is functional); (3) to establish the clinical relevance in patients with ineffective motility (to determine the peristaltic reserve or motility normalization); (4) to identify the patients with post-fundoplication dysphagia that could respond to dilation; (5) to assess patients with suspected achalasia (typical clinical and radiologic findings but inconclusive HREM); and (6) to assess patients with aperistalsis, to determine whether it is early achalasia or whether there is peristaltic reserve (Table 1).
In summary, current HREM has evolved from a study of only 10 liquid swallows into a test that indispensably utilizes challenge tests. These tests include the “rapid drink challenge”, the “multiple rapid swallow”, a study with pharmacologic agents (not discussed in this editorial), and the STM.11 The rice-based STM is practical, adds only 8 additional minutes to the HREM, can be performed at any motility laboratory, has a minimal additional cost, the food (200 g of precooked rice) is easily accessible, and requires no special care. This test enables the diagnosis of a major motility disorder to be made in a larger number of patients (e.g., in 43%, compared with only 22% with the use of the conventional liquid swallow protocol, p < 0.0001). In patients with dysphagia, the benefit is even higher (67% with the STM vs. 35% with the ST, p < 0.0001).12 In patients with dysphagia, the STM contributes to determining the significance of certain motility disorders, such as ineffective motility or esophagogastric junction outflow obstruction (e.g., the normalization of those disorders during the STM).17 Likewise, the reproduction of esophageal symptoms increases with the STM.
Nevertheless, some questions still need to be resolved, with respect to the use of challenge tests with food, given that the type of solid food varies in the different studies.17 These observations require more prospective studies. Regarding the STM with precooked rice, it appears to be practical, effective, reasonable, and reproducible. Future prospective studies must focus on examining the value of the STM, to determine its therapeutic utility. In the meantime, we should congratulate García-Zermeño et al. for having established normal values in a Latin American population (albeit in a limited number of 25 healthy controls), to confirm once more that the STM identifies more motility disorders, compared with the conventional protocol, and to clarify the clinical significance in patients with ineffective motility.
Financial disclosureNo financial support was received in relation to this editorial.
Conflict of interestThe authors declare that there is no conflict of interest.