Jackhammer esophagus is a recently identified motility disorder. Experience with the novel pathologic condition has been reported in different studies but there is little information on the subject in Latin America. Our case series conducted in Bogota, Colombia, describes the prevalence of jackhammer esophagus and its demographic, clinical, and manometric characteristics.
Materials and methodsA retrospective, observational, cross-sectional study included consecutive patients diagnosed with jackhammer esophagus that were referred for high-resolution esophageal manometry. Their clinical and manometric records were reviewed, and the pertinent information for the present study was collected.
ResultsWithin the study period, 6445 patients were evaluated through esophageal manometry, 27 of whom were diagnosed with jackhammer esophagus (prevalence of 0.42%). The majority of those patients were women (n = 17, 63%) in the sixth decade of life. The most common symptom was regurgitation (n = 17, 63%), followed by dysphagia (n = 15, 56%). The mean distal contractile integral was 9384 (5,095−18,546) mmHg·s·cm. Dysphagia was more common in patients > 60 years of age (79%, p < 0.01) and regurgitation was more frequent in patients < 60 years of age (92%, p < 0.03).
ConclusionsThe present study is the first to characterize the prevalence of jackhammer esophagus and its demographic, clinical, and manometric characteristics in Latin American patients. The prevalence of jackhammer esophagus in our study population was considerably lower than that reported in international case series. Our findings suggest that there are important geographic differences in the prevalence and clinical presentation of jackhammer esophagus, compared with data from other international centers.
“Jackhammer Esophagus” (o esófago en “martillo hidráulico” en español), es un trastorno motor esofágico identificado recientemente. Diversos estudios han descrito su experiencia con este novel padecimiento. Sin embargo, no existe información al respecto en Latinoamérica. Nuestro trabajo describe la prevalencia, características demográficas, clínicas y manométricas en una serie de casos con “Jackhammer Esophagus” en Bogotá, Colombia.
Materiales y MétodosEste es un trabajo observacional retrospectivo de corte transversal. Pacientes consecutivos referidos para manometría esofágica de alta resolución diagnosticados con “Jackhammer Esophagus” fueron considerados para el estudio. Los expedientes clínicos y manométricos de estos enfermos fueron revisados y la información pertinente extraída.
ResultadosDurante el periodo de estudio, 6445 pacientes fueron evaluados con manometría esofágica, 27 fueron diagnosticados con “Jackhammer Esophagus” (prevalencia 0.42%). La mayor parte, fueron mujeres (n = 17,63%) mujeres en la sexta década. El síntoma más común fue la regurgitación (n = 17 63%), seguido por disfagia (n = 15 56%). El promedio de contracción distal integral observado fue 9,384 (5,095-18,546) mm Hg-s-cm. Disfagia fue más común (79% p < .01) en pacientes de > 60 años y regurgitación más frecuente (92%, p < .03) en < 60 años.
ConclusionesEste es el primer estudio en caracterizar la prevalencia, hallazgos demográficos, clínicos y manométricos en pacientes con “Jackhammer Esophagus” en Latino América. En nuestra población, la prevalencia de este trastorno es notablemente más baja que en series internacionales. Nuestros hallazgos sugieren la existencia de importantes diferencias geográficas en la prevalencia y presentación clínica de “Jackhammer Esophagus” en comparación con datos de otros centros internacionales.
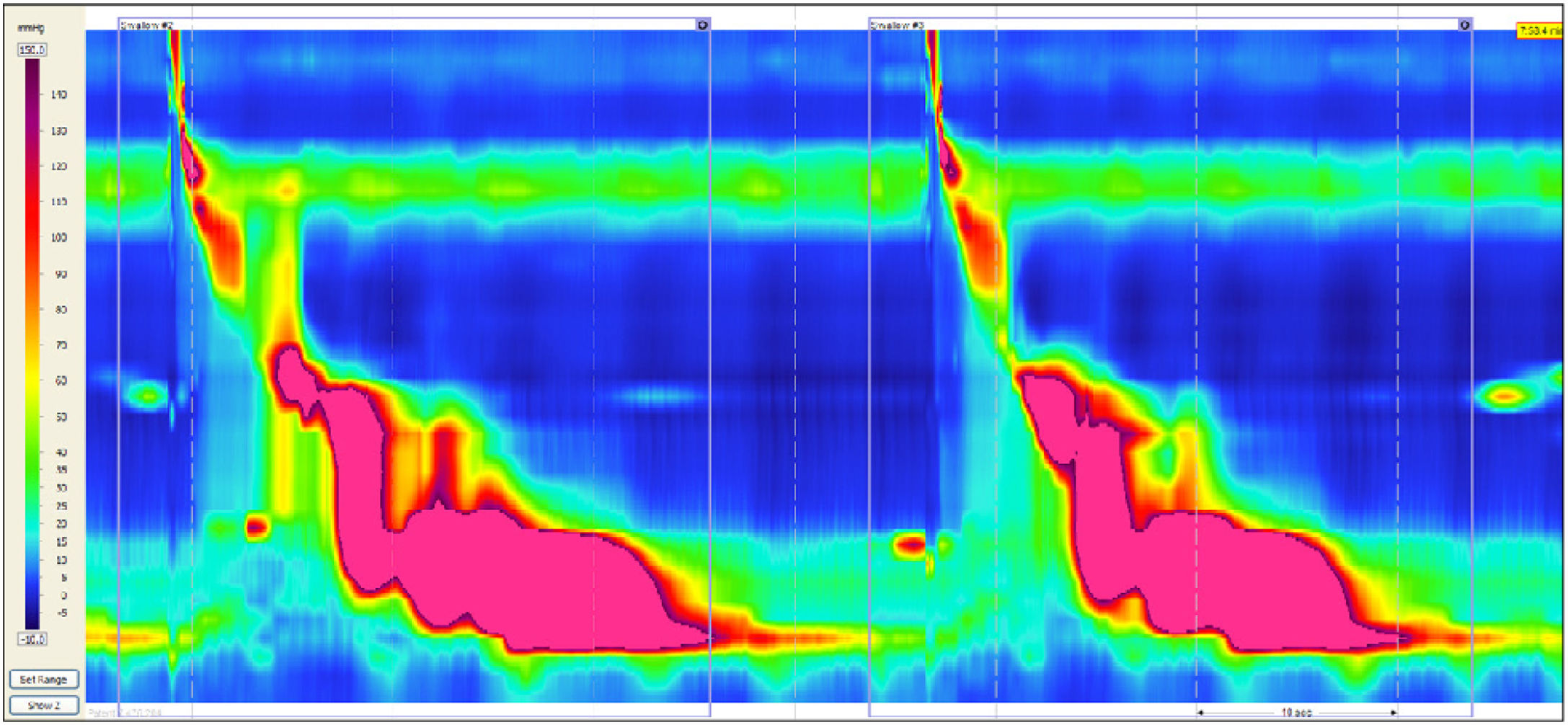
The advent of high-resolution esophageal manometry (HREM) has made the identification of new motility disorders possible. In January 2012, Román et al. first described a phenotype of extreme esophageal contraction with a distal contractile integral (DCI) > 8,000 mmHg-s-cm. The highest DCI value in 72 healthy controls was 7,732 mmHg-s-cm. Therefore, those researchers designated DCI values ≥ 8,000 mmHg-s-cm as abnormal, describing it with the term “jackhammer esophagus” (JHE).1 Since its discovery and up to the present, experience with that pathology has been reported in studies from different parts of the world,2 including Canada,3 Europe,4–7 Saudi Arabia,8 Asia,9 and the United States.1,10,11 However, data on the subject are scare in Latin America. Specifically, no case series from Latin American medical centers have been published. The aim of our study was to describe our experience with this motility disorder (specifically, its prevalence and demographic, clinical, and manometric characteristics) in a patient population in Bogota, Colombia, and compare our cases with those in the international literature.
Materials and methodsGeographic locationOur study was conducted at the Hospital Universitario San Ignacio in Bogota, Colombia. Bogota is a city with a population of 10,773,332 inhabitants in the metropolitan area,12 and is the sixth largest city in Latin America. The Hospital Universitario San Ignacio is a private tertiary care hospital that is a gastroenterology referral center, treating a large population from the metropolitan area, as well as from other municipalities and cities in the South of the country (Fig. 1).
PopulationThe study included consecutive patients that met the diagnostic criterion for JHE that were referred to our esophageal manometry unit, within the time frame of January 2011 and December 2017. Their clinical records were reviewed to determine the indications for the procedure and to collect the demographic data. Only those patients whose studies were completed with HREM were included in the analysis.
Study designThe present study was retrospective, observational, and cross-sectional. Each patient’s information was entered into a computer program that was specifically designed for the purpose of the analysis. All the manometry tracings were reviewed by an expert researcher (AH) experienced in high-resolution manometry interpretation. The studies were analyzed, utilizing the most recent Chicago classification (version 3.0).13
Esophageal manometryThe patients underwent esophageal manometry study after having fasted for at least 6 h. Medications that potentially affect esophageal motility, such as anticholinergics, calcium channel blockers, nitrates, opioids, muscle relaxants, and prokinetics, were suspended 5-7 days before the procedure, when possible.
A solid-state catheter, measuring 4.2 mm at its outer diameter, with 36 circumferential sensors spaced at 1 cm intervals (Given Imaging, Los Angeles, CA), was employed. The transducers were calibrated at 300 mmHg, using externally applied pressure, and responded to pressure > 6,000 mmHg/s, with measurement accuracy of ± 2 mmHg.
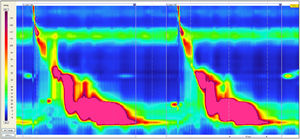
The patients were studied in a semi-supine position for the procedure. The manometry catheter was introduced transnasally and positioned to register pressure from the hypopharynx to the stomach, with approximately 3 intragastric sensors. Once the recording catheter was introduced, and before the study began, the patient was given a 5-10 min adaptation period. Our procedure protocol was adopted from that of Pandolfino et al.14 The study included at least one 30-second baseline recording and ten 5 ml liquid swallows every 30 seconds. The data were analyzed utilizing ManoView ™ software (Given Imaging, Los Angeles, CA, USA). The HREM tracings were also visually evaluated using the isobaric contour, aided by the software. The DCI was analyzed using the ManoView ™ automatic function and was measured between the proximal (P) pressure trough and the esophagogastric junction or the distal (D) pressure trough. Only pressures above 20 mmHg contributed to the calculation of the DCI expressed in mmHg-s-cm.15
Jackhammer esophagus diagnosisThe diagnosis of JHE was based on version 3.0 of the Chicago classification proposed by Kharilas et al.: ≥ 20% of the liquid swallows with a DCI ≥ 8,000 mmHg-s-cm and normal latency.16
Indications: the dominant symptom for which patients were referred for manometric study was obtained from the clinical records and listed as follows: dysphagia, chest pain, regurgitation, and/or heartburn.
Statistical analysisThe information was entered in a database in Excel, with the demographic, clinical, and manometric variables of interest. The categorical variables were expressed through proportions and the quantitative variables, according to distribution, were expressed through measures of central tendency, as mean and standard deviation, if they met the criterion of normality, and as median and interquartile range if they did not meet the criterion. Normality was determined through the Shapiro-Wilk test.
Ethical considerationsThe present study was reviewed and approved by the ethics committee of the Hospital Universitario San Ignacio in Bogota, Colombia. The names of the participants were kept confidential. Given the study’s retrospective design, individual informed consent was not required.
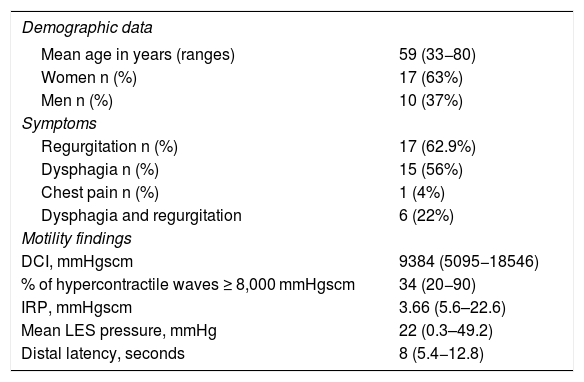
ResultsDuring the study period, a total of 6,445 patients were referred for HREM study, 27 (0.42%) of whom met the diagnostic criterion of JHE. Table 1 summarizes the demographic data, study indications, and high-resolution manometry findings. The majority of patients were women (n = 17, 63%) and the mean age of the patients was 59 years (range 33-80). The most common symptom was regurgitation (n = 17, 63%), followed by dysphagia (n = 15, 56%). Only one patient (4%) presented with chest pain, and none presented with heartburn. The percentages do not add up to 100% because 6 patients (22%) presented with both regurgitation and dysphagia.
Demographic, clinical, and manometric characteristics of patients with jackhammer esophagus (JHE) (n = 27).
| Demographic data | |
|---|---|
| Mean age in years (ranges) | 59 (33−80) |
| Women n (%) | 17 (63%) |
| Men n (%) | 10 (37%) |
| Symptoms | |
| Regurgitation n (%) | 17 (62.9%) |
| Dysphagia n (%) | 15 (56%) |
| Chest pain n (%) | 1 (4%) |
| Dysphagia and regurgitation | 6 (22%) |
| Motility findings | |
| DCI, mmHgscm | 9384 (5095−18546) |
| % of hypercontractile waves ≥ 8,000 mmHgscm | 34 (20−90) |
| IRP, mmHgscm | 3.66 (5.6–22.6) |
| Mean LES pressure, mmHg | 22 (0.3–49.2) |
| Distal latency, seconds | 8 (5.4−12.8) |
DCI: distal contractile integral; IRP: integrated relaxation pressure; LES: lower esophageal sphincter.
*In some cases, the patients had more than one symptom.
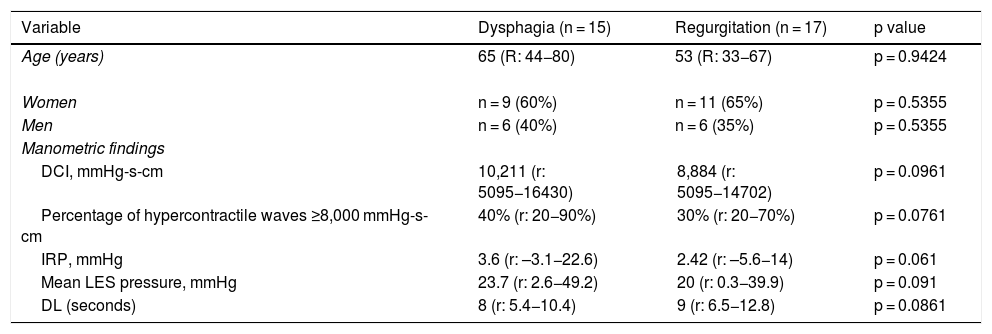
Table 2 compares the findings in our population grouped by symptom presentation: regurgitation or dysphagia. Even though the data showed no statistically significant differences, partially due to the small sample size, certain trends could be appreciated. For example, the patients with dysphagia tended to be older (a mean of 65 years, range: 44-80), compared with the patients with regurgitation (a mean of 53 years, range: 33-67), (p = 0.9424). The exception was the one patient with chest pain, who was 73 years old (not shown in the table). The findings in that male patient were a mean DCI of 18,546 mmHg-sg, 20% of hypercontractile waves ≥ 8000 mmHg-sg, IRP of 12 mmHg-sg, mean LES of 13.3 mmHg-sg, and distal latency of 7 s. In relation to sex, women had a higher prevalence of regurgitation (65% vs. 35%) and dysphagia (60% vs. 40%), albeit with no statistical significance (p = 0.5355). Likewise, mean DCI values were higher in the patients with dysphagia, than in the patients with regurgitation (10,211 vs. 8,884 mmHg-sg) (p = 0.0961). The exception was the patient with chest pain (18,546 mmHg-sg). Similarly, the percentage of hyperperistaltic contractions was slightly higher in the patients with dysphagia (40%, range: 20-90), than in the patients with regurgitation (30%, range 20-70) (p = 0.0761).
Comparison of the symptoms and manometric findings in JHE, based on the main indication for manometric study.
| Variable | Dysphagia (n = 15) | Regurgitation (n = 17) | p value | |
|---|---|---|---|---|
| Age (years) | 65 (R: 44−80) | 53 (R: 33−67) | p = 0.9424 | |
| Women | n = 9 (60%) | n = 11 (65%) | p = 0.5355 | |
| Men | n = 6 (40%) | n = 6 (35%) | p = 0.5355 | |
| Manometric findings | ||||
| DCI, mmHg-s-cm | 10,211 (r: 5095−16430) | 8,884 (r: 5095−14702) | p = 0.0961 | |
| Percentage of hypercontractile waves ≥8,000 mmHg-s-cm | 40% (r: 20−90%) | 30% (r: 20−70%) | p = 0.0761 | |
| IRP, mmHg | 3.6 (r: –3.1−22.6) | 2.42 (r: –5.6−14) | p = 0.061 | |
| Mean LES pressure, mmHg | 23.7 (r: 2.6−49.2) | 20 (r: 0.3−39.9) | p = 0.091 | |
| DL (seconds) | 8 (r: 5.4−10.4) | 9 (r: 6.5−12.8) | p = 0.0861 | |
DCI: distal contractile integral; DL: distal latency; IRP: integrated relaxation pressure; LES: lower esophageal sphincter; r: range.
*In some cases, the patients had more than one symptom, which is why there are more than 27 patients.
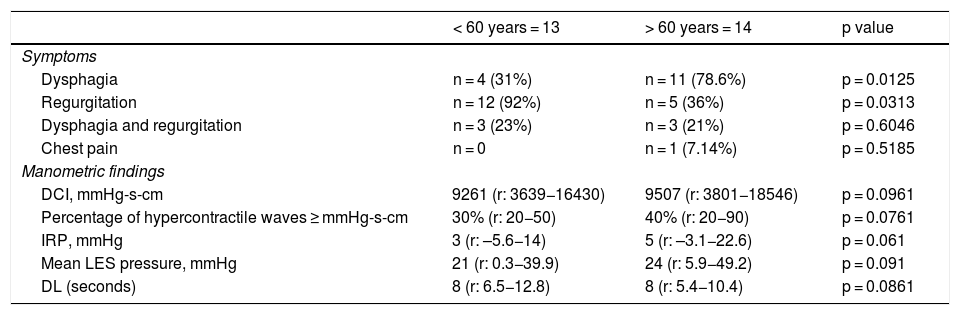
When grouping our patients by age > 60 years or age < 60 years, dysphagia was the most common symptom in those > 60 years of age n = 11(79%) vs. those < 60 years of age n = 4(31%) (p = 0.0125). In contrast, regurgitation occurred more frequently in patients < 60 years of age (n = 12, 92%) vs. those > 60 years of age n = 5(36%) (p = 0.0313). There were no statistically significant manometric differences based on age > 60 years or < 60 years (Table 3).
Distribution of symptoms and motility findings based on age: < 60 years or > 60 years.
| < 60 years = 13 | > 60 years = 14 | p value | ||
|---|---|---|---|---|
| Symptoms | ||||
| Dysphagia | n = 4 (31%) | n = 11 (78.6%) | p = 0.0125 | |
| Regurgitation | n = 12 (92%) | n = 5 (36%) | p = 0.0313 | |
| Dysphagia and regurgitation | n = 3 (23%) | n = 3 (21%) | p = 0.6046 | |
| Chest pain | n = 0 | n = 1 (7.14%) | p = 0.5185 | |
| Manometric findings | ||||
| DCI, mmHg-s-cm | 9261 (r: 3639−16430) | 9507 (r: 3801−18546) | p = 0.0961 | |
| Percentage of hypercontractile waves ≥ mmHg-s-cm | 30% (r: 20−50) | 40% (r: 20−90) | p = 0.0761 | |
| IRP, mmHg | 3 (r: –5.6−14) | 5 (r: –3.1−22.6) | p = 0.061 | |
| Mean LES pressure, mmHg | 21 (r: 0.3−39.9) | 24 (r: 5.9−49.2) | p = 0.091 | |
| DL (seconds) | 8 (r: 6.5−12.8) | 8 (r: 5.4−10.4) | p = 0.0861 | |
Values do not add up to 100% because several patients had more than one symptom.
DCI: distal contractile integral; DL: distal latency; IRP: integrated relaxation pressure; LES: lower esophageal sphincter; r: range.
HREM has become the standard method for evaluating unexplained esophageal symptoms.17,18 JHE is an esophageal motility disorder identified in the past decade, thanks to the introduction of HREM.14 Since its first description in 2012,1 to the present, JHE has been described in studies from North America,3,19–22 Europe,4 and Asia,23 but information on the disorder is very limited in Latin America, with only one clinical case.24 Our study is the first to provide information on JHE in a case series on a Latin American population. The aim of our study was to characterize the demographic, clinical, and manometric presentation of this novel motility disorder in our patient population in Bogota, Colombia.
At our tertiary care referral center, the prevalence of JHE was n = 27/6,425 (0.42%) or 4.2 per 1,000 patients undergoing manometry. In comparison, the prevalence of JHE described in different international case series ranges from 1.5 to 4%.1,3,20,25 The considerably lower prevalence of JHE at our center suggests the possibility of epidemiologic differences related to geography. Future studies are needed to confirm our observations.
The majority of patients in our population were women (n = 17, 63%) and mean patient age was 59 years (33-80), coinciding with findings in the literature reported by different researchers.1,19,25,26 A recent Spanish study described a case series of patients with JHE (n = 7), 100% of whom were women.27 Why the disorder occurs more frequently in women in the fifth or sixth decade of life has not been critically evaluated, but given the consistency of those findings across countries and continents, merits additional study.
The most common symptoms in our population were regurgitation n= 18(67%) and dysphagia n = 15(56%). Our case series differs from the majority of studies from other centers, in which dysphagia is the predominant symptom, with a prevalence that varies from 47-86%.1–26 However, regurgitation has also been described in other series at between 24% and 35%.4–19 Interestingly, the analysis of our population based on age > 60 years or < 60 years showed that dysphagia was the predominant symptom in patients > 60 years of age (79%, p < 0.0125), whereas regurgitation was predominant in the patients < 60 years of age (92%, p < 0.0313). That age-based symptomatic predilection has not been previously reported.
The cause of JHE has yet to be established. One proposed theory is an excess of cholinergic activity, causing “temporal asynchrony” between the contractions of the circular and longitudinal muscle layers of the muscularis propria.28 Other researchers have postulated the possible association with gastroesophageal reflux disease (GERD).29 In two European studies, one in Austria (n = 37)25 and the other in France (n = 43),26 a 43% prevalence of GERD was reported in both. The high prevalence of regurgitation in our case series suggests the possibility that gastroesophageal reflux plays a pathogenic role in the disorder. The systematic use of esophageal pH-monitoring in those patients would be of great interest in future studies. Recent publications have found an association between JHE and eosinophilic esophagitis.24,30 In addition, Japanese researchers have suggested that there is an eosinophilic infiltration at the level of the deep muscle layer that causes eosinophilic myositis, but without affecting the esophageal mucosa.31–33 Those studies indicate that further research is necessary to evaluate the role of the eosinophil in the genesis of JHE. Recent studies utilizing multiple swallows or repetitive swallows have suggested there is a heterogeneous abnormality of the inhibitory control of the neuronal network in patients with JHE.34 In summary, the cause of JHE remains unknown and is under study. In our case series, we detected no patient with eosinophilic infiltration into the mucosa and we did not systematically study the presence of GERD.
Several individual case studies or limited case series (n = 8) have described the progression of JHE to achalasia.35,36 Huang et al. found that the most important factor in determining progression to achalasia was incomplete or dysfunctional relaxation of the esophagogastric junction.36 Those observations are supported by a recent case, in which functional obstruction of the esophagogastric junction due to a gastric band was associated with JHE, which was resolved by removing the pressure created by the gastric band.37 Only one patient in our case series had IRP pressures above 15 mmHg, suggesting functional obstruction of the esophagogastric junction. We did not study the longitudinal long-term progression of our patients (> 12 months).
The main strength of the present work was the analysis of the variables that enabled the correlation between clinical indication, demographic aspects, and high-resolution manometry. Our study limitations included its retrospective design and the modest number of patients (n = 27). However, our sample size is similar to that of other retrospective case series and analyses published in the literature,1,3,20,25 and can be explained by the relatively low prevalence of JHE. An additional limitation was the fact that we did not objectively evaluate the presence of GERD, or associations with other diseases, such as eosinophilic esophagitis, nor did we determine the subtypes or patterns of JHE (one peak or multiple peaks), albeit the practical clinical importance of that observation is still unknown.
ConclusionsIn conclusion, the present case series is the first to describe JHE in Latin America. We found a low prevalence (0.42%) of JHE at our hospital center in Colombia. The patients in our case series population were predominantly female, in the fifth/sixth decade of life, and the most common symptoms were regurgitation and dysphagia. In the age-based analysis, dysphagia was the most prevalent symptom in the patients > 60 years of age. We found no statistically significant manometric differences between our patients, but mean DCI values were higher in the patients with dysphagia than in those with regurgitation (10,211 vs. 8,884 mmHg-sg, respectively). Similarly, the percentage of hyperperistaltic contractions tended to be higher in the patients with dysphagia (40%, range: 20-90), than in those with regurgitation (30%, range: 20-70). Compared with other international case series, our findings suggest there are geography-related epidemiologic differences regarding JHE and confirm its predominance in women in the fifth or sixth decade of life. In addition, they highlight important symptomatic differences in clinical presentation based on age.
Financial disclosureNo financial support was received in relation to this study.
Conflict of interestThe authors declare that there is no conflict of interest.
Please cite this article as: Hani A, Zuluaga C, Costa V, Leguizamo AM, Puentes G, Ardila AF, et al. «Jackhammer esophagus» (esófago en martillo hidráulico): prevalencia, características demográficas, clínicas y manométricas. Revista de Gastroenterología de México. 2020;85:421–427.