The solid test meal (STM) is a challenge test that is done during esophageal manometry and appears to increase the diagnostic yield of the study. The aim of our analysis was to establish the normal values for STM and evaluate its clinical utility in a group of Latin American patients with esophageal disorders versus healthy controls.
Material and methodsA cross-sectional study was conducted on a group of healthy controls and consecutive patients that underwent high-resolution esophageal manometry, in which STM was done at the final part of the study and consisted of asking the subjects to eat 200 g of precooked rice. The results were compared during the conventional protocol and the STM.
ResultsTwenty-five controls and 93 patients were evaluated. The majority of the controls (92%) completed the test in under 8 min. The STM changed the manometric diagnosis in 38% of the cases. The STM diagnosed 21% more major motor disorders than the conventional protocol; it doubled the cases of esophageal spasm and quadrupled the cases of jackhammer esophagus, whereas it demonstrated normal esophageal peristalsis in 43% of the cases with a previous diagnosis of ineffective esophageal motility.
ConclusionsOur study confirms the fact that complementary STM during esophageal manometry adds information and enables a more physiologic assessment of esophageal motor function to be made, compared with liquid swallows, in patients with esophageal motor disorders.
La prueba con comida sólida (PCS) es una prueba de provocación que se realiza durante una manometría esofágica y al parecer incrementa el rendimiento diagnóstico de ésta. El objetivo de este estudio fue establecer los valores de normalidad de la PCS y evaluar su utilidad clínica en un grupo de pacientes hispanos con trastornos esofágicos y controles sanos.
Material y métodosSe realizó un estudio transversal en un grupo de controles sanos y pacientes consecutivos que fueron sometidos a una manometría esofágica de alta resolución, donde al final se realizó la PCS que consistió en pedirles que comieran 200 gramos de arroz precocido. Se compararon los resultados obtenidos durante el protocolo convencional y la PCS.
ResultadosSe evaluaron 25 controles y 93 pacientes. La mayoría de los controles (92%) completaron la prueba en un tiempo menor de 8 minutos. La PCS cambió el diagnóstico manométrico en el 38% de los casos. La PCS diagnosticó 21% más trastornos motores mayores que el protocolo convencional, en especial se duplicaron los casos de espasmo esofágico y se cuadruplicaron los casos de esófago en martillo neumático. Por otro lado, la PCS demostró una peristalsis esofágica normal en 43% de los casos con diagnóstico previo de motilidad esofágica inefectiva.
ConclusionesNuestro estudio confirma que la realización de una PCS complementaria durante el protocolo de manometría esofágica añade información y permite una evaluación más fisiológica de la función motora esofágica en comparación con las degluciones líquidas en pacientes con trastornos motores del esófago.
With the advent of high-resolution esophageal manometry (HREM), the way of classifying esophageal motor disorders changed substantially. In 2009, a group of experts formulated the Chicago classification (CC) for esophageal motor disorders, for the purpose of creating diagnostic algorithms to provide homogeneous approaches and therapies worldwide.1 That classification has evolved over time, and even though version 3 (CCv3.0) has been the most widely used, the latest version came out in 2021 (CCv4.0).2,3
The standard protocol, according to the CCv3.0,2 is based on the evaluation of 10 liquid swallows (LSs), with a programmed sequence, and should be carried out with the subject in the supine position. The new CCv4.0 protocol recommends performing an additional sequence of multiple rapid swallows (MRSs) (for evaluating the peristaltic reserve), carrying out at least 5 swallows in a seated position, and then carrying out a rapid drink challenge (RDC) with 200 ml of water.3–5 The new protocol notwithstanding, if there is no conclusive evidence of a major motility disorder, or if the findings do not explain patient symptoms, support measures that include solid swallows,6 a drug challenge (amyl nitrite or cholecystokinin),7,8 or a solid test meal (STM) can be considered.9,10
The STM is the challenge test that perhaps best reflects esophageal physiology during eating, thus providing better diagnostic accuracy. In 2017, in two different studies, The Mark Fox group in Switzerland established normal values for the STM by evaluating healthy controls and patients with motility disorders in the United Kingdom.9,10 With the addition of that modification to the Chicago protocol, known as the Chicago classification adapted for solids (CCS), STM was shown to increase the number of patients that are diagnosed with a major esophageal motility disorder, especially in patients evaluated for dysphagia. More recently, in a French cohort of patients with dysphagia, STM increased the number of major motor disorders diagnosed, by 13.4%.11
Even though there is evidence on the clinical utility of the STM in the evaluation of motor disorders of the esophagus, the information comes from two European cohorts (the United Kingdom and France). Therefore, the primary aim of the present study was to establish normal STM values and evaluate its clinical utility in a group of Latin American patients with esophageal disorders versus healthy controls.
Material and methodsPopulation studiedA cross-sectional study was conducted on subjects invited to voluntarily participate in the investigation. All the subjects had been referred to either the Department of Digestive Physiology and Gastrointestinal Motility of the Instituto de Investigaciones Medico Biológicas of the Universidad Veracruzana (Veracruz, Mexico) or the Neurogastroenterology Unit of the Department of Gastroenterology of the Hospital Italiano de Buenos Aires (Buenos Aires, Argentina), within the time frame of April to June 2018, to undergo HREM due to esophageal symptoms, such as heartburn, regurgitation, noncardiac chest pain, and dysphagia. Patients with previous esophageal surgery, psychiatric comorbidity, severe chronic disease (cancer, chronic kidney disease, diabetes mellitus with complications) or any other condition impeding the performance of HREM, were excluded.
At the same time, healthy controls (HCs) were prospectively recruited. They were invited to voluntarily participate through summons on social media networks and posters. All study participants signed written statements of informed consent. In addition, all the participants filled out questionnaires that evaluated gastrointestinal symptoms (GERD-Q and PAGI-SYM)12,13 and the Hospital Anxiety and Depression Scale (HADS) questionnaire.14 The subjects whose questionnaire results showed no gastrointestinal symptoms were considered the HCs.
Study protocolAt least one week prior to the manometry study, the patients suspended medications that could alter esophageal function, such as prokinetics, calcium channel blockers, anticholinergics, opioids, or nitrates. After an 8 h fast, HREM was carried out on all patients and HCs, in a 45º angle reclining position, in accordance with the CCv3.0 protocol.2 A solid state catheter with 36 pressure sensors (Manoscan, Medtronic, Los Angeles, CA, USA) was used. During the procedure, the catheter was placed via the nasal route, with the distal sensor placed 2 or 3 centimeters below the diaphragm. The CCv3.02 protocol was carried out to evaluate esophagogastric motility. It consisted of a baseline resting period of at least 30 seconds, followed by a series of 10 swallows of 5 ml of water at room temperature applied with a syringe, as well as the MRS test, through 5 rapid swallows of 2 ml of water, administered in 10 s. The subjects then underwent the STM protocol, which consisted of their ingesting 200 g of soft, warm precooked rice. It was ingested with the subjects in the vertical position, using a fork, at his/her natural rhythm, for a period of 8 min, just as suggested in the studies by Mark Fox.9,10
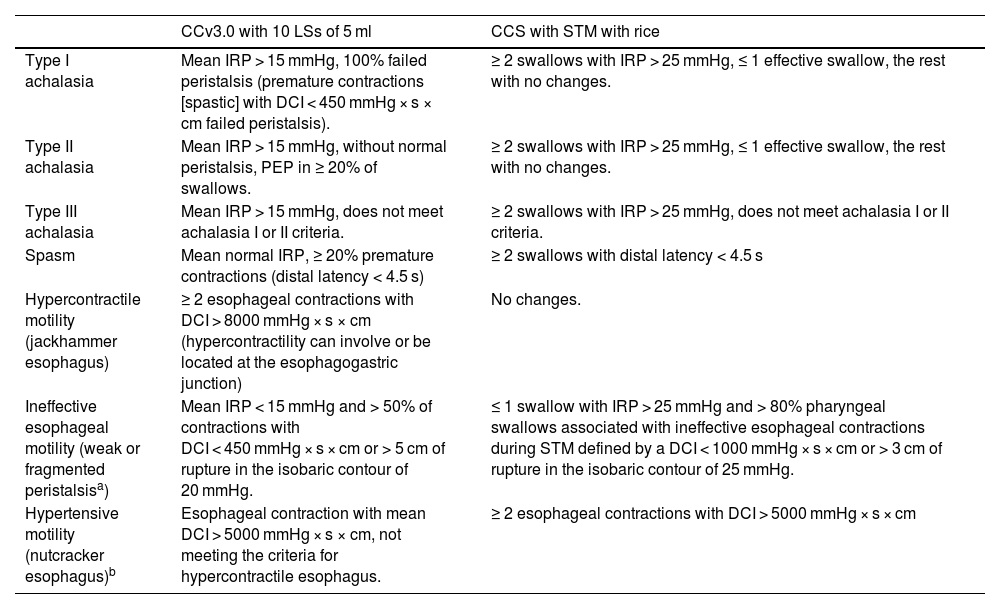
The parameters evaluated during the conventional protocol were upper esophageal sphincter (UES) characteristics; esophagogastric junction (EGJ) morphology (type I-III EGJ); manometric diagnosis of the esophageal motility pattern, according to the CCv3.0; and the adaptation proposed for solid food (CCS) (Table 1). In addition, during the STM, the number of swallows, quantity of rice intake, intake time, grams of rice per minute, grams of rice per swallow, number of effective swallows, and number of effective contractions per minute were registered.
Esophageal motor disorder classification according to the conventional Chicago version 3.0 classification and the solid test meal classification.
| CCv3.0 with 10 LSs of 5 ml | CCS with STM with rice | |
|---|---|---|
| Type I achalasia | Mean IRP > 15 mmHg, 100% failed peristalsis (premature contractions [spastic] with DCI < 450 mmHg × s × cm failed peristalsis). | ≥ 2 swallows with IRP > 25 mmHg, ≤ 1 effective swallow, the rest with no changes. |
| Type II achalasia | Mean IRP > 15 mmHg, without normal peristalsis, PEP in ≥ 20% of swallows. | ≥ 2 swallows with IRP > 25 mmHg, ≤ 1 effective swallow, the rest with no changes. |
| Type III achalasia | Mean IRP > 15 mmHg, does not meet achalasia I or II criteria. | ≥ 2 swallows with IRP > 25 mmHg, does not meet achalasia I or II criteria. |
| Spasm | Mean normal IRP, ≥ 20% premature contractions (distal latency < 4.5 s) | ≥ 2 swallows with distal latency < 4.5 s |
| Hypercontractile motility (jackhammer esophagus) | ≥ 2 esophageal contractions with DCI > 8000 mmHg × s × cm (hypercontractility can involve or be located at the esophagogastric junction) | No changes. |
| Ineffective esophageal motility (weak or fragmented peristalsisa) | Mean IRP < 15 mmHg and > 50% of contractions with DCI < 450 mmHg × s × cm or > 5 cm of rupture in the isobaric contour of 20 mmHg. | ≤ 1 swallow with IRP > 25 mmHg and > 80% pharyngeal swallows associated with ineffective esophageal contractions during STM defined by a DCI < 1000 mmHg × s × cm or > 3 cm of rupture in the isobaric contour of 25 mmHg. |
| Hypertensive motility (nutcracker esophagus)b | Esophageal contraction with mean DCI > 5000 mmHg × s × cm, not meeting the criteria for hypercontractile esophagus. | ≥ 2 esophageal contractions with DCI > 5000 mmHg × s × cm |
CCS: Chicago classification adapted for solids; CCv3.0; Chicago classification version 3.0; DCI: distal contractile integral; IRP: integrated relaxation pressure; LSs: liquid swallows; PEP: panesophageal pressurization; STM: solid test meal.
The data were collected by the team of authors on a Microsoft Excel calculation sheet (XP professional edition; Microsoft Corp, Redmond, WA, USA). The manometric diagnoses were expressed as frequencies and percentages. The comparison between two quantitative variables was carried out using the Student’s t test, and the multiple variable comparison was made with the ANOVA test with the Bonferroni correction. The kappa concordance test was applied to evaluate agreement upon comparing the diagnoses according to the CCv3.0 with those of the STM. The statistical analysis was performed using the SPSS version 22 (IBM, Chicago, Illinois) program.
Ethical considerationsAll the procedures were carried out according to the provisions of the General Health Law in Health Research regulations, and the study subjects provided their informed consent. The study protocol met the ethical guidelines of the 1975 Declaration of Helsinki (the 2013 revision) and was approved and reviewed by the Ethics Committee of the IIMB-UV (registration number 2018-007/3).
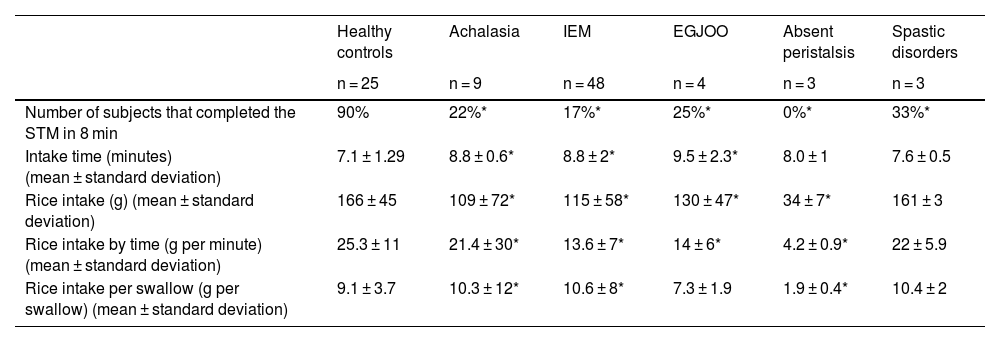
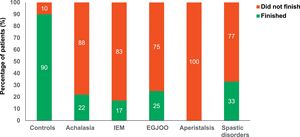
ResultsTwenty-five HCs (60% men, mean age 25 ± 5 years) and 93 patients (61% women, mean age 52.4 ± 5) were consecutively included in the study. Twenty-three (92%) of the HCs completed the STM and Table 2 shows the values of the parameters evaluated.
Mean values of the parameters obtained during the solid test meal.
| Healthy controls | Achalasia | IEM | EGJOO | Absent peristalsis | Spastic disorders | |
|---|---|---|---|---|---|---|
| n = 25 | n = 9 | n = 48 | n = 4 | n = 3 | n = 3 | |
| Number of subjects that completed the STM in 8 min | 90% | 22%* | 17%* | 25%* | 0%* | 33%* |
| Intake time (minutes) (mean ± standard deviation) | 7.1 ± 1.29 | 8.8 ± 0.6* | 8.8 ± 2* | 9.5 ± 2.3* | 8.0 ± 1 | 7.6 ± 0.5 |
| Rice intake (g) (mean ± standard deviation) | 166 ± 45 | 109 ± 72* | 115 ± 58* | 130 ± 47* | 34 ± 7* | 161 ± 3 |
| Rice intake by time (g per minute) (mean ± standard deviation) | 25.3 ± 11 | 21.4 ± 30* | 13.6 ± 7* | 14 ± 6* | 4.2 ± 0.9* | 22 ± 5.9 |
| Rice intake per swallow (g per swallow) (mean ± standard deviation) | 9.1 ± 3.7 | 10.3 ± 12* | 10.6 ± 8* | 7.3 ± 1.9 | 1.9 ± 0.4* | 10.4 ± 2 |
EGJOO: esophagogastric junction outflow obstruction; IEM: ineffective esophageal motility.
According to the CCv3.0 protocol, 22 HCs had normal esophageal motility (88%) and 3 (12%) had ineffective esophageal motility (IEM). None of the HCs reported esophageal symptoms during the performance of the test, and the mean time for its completion was 7.1 ± 1.29 min, with a mean rice intake of 166 ± 45 g during that period.
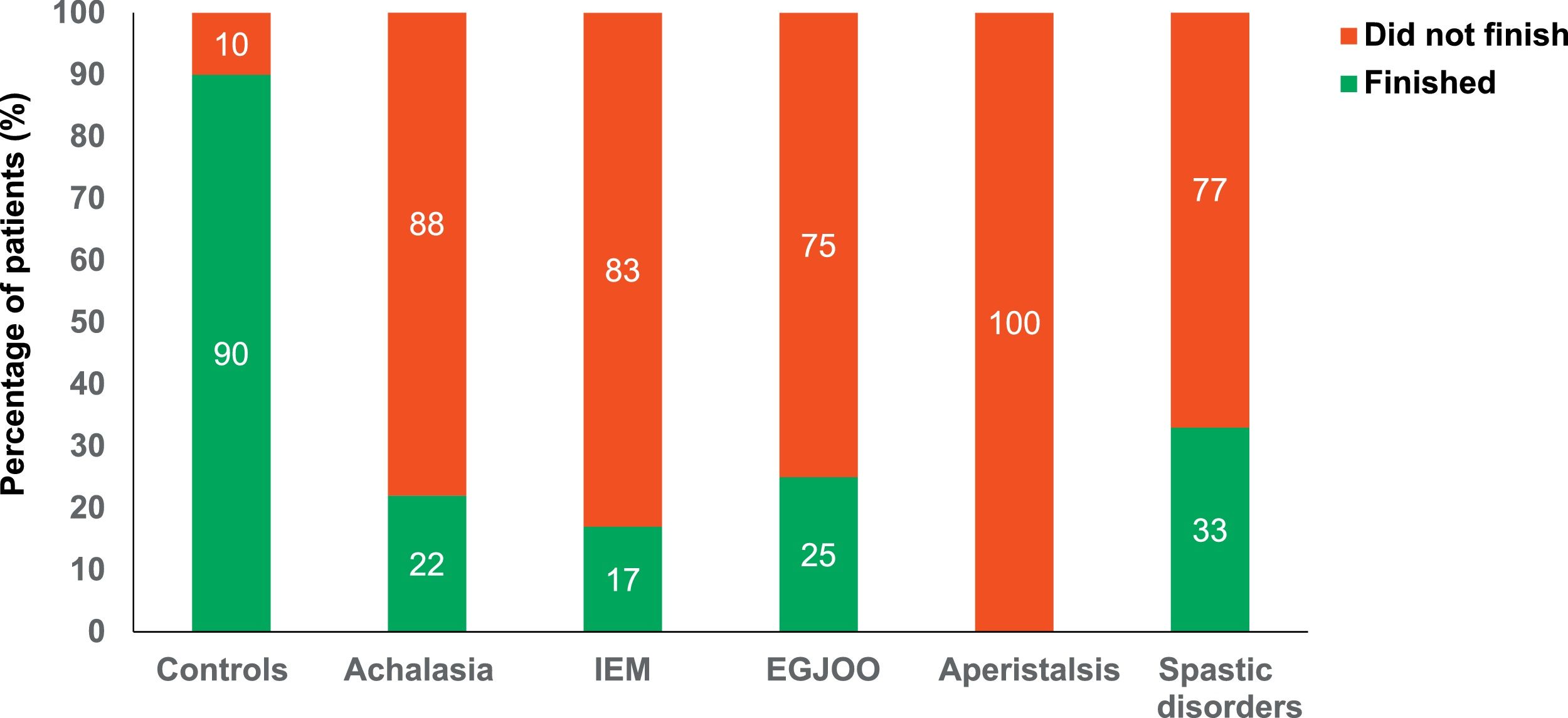
The study patients were seen and evaluated for the following symptoms: typical reflux symptoms (heartburn/regurgitation), 71 (76%); dysphagia, 16 (17%); and chest pain, 6 (7%). The diagnoses according to the CCv3.0 were normal esophageal motility in 32% (n = 29), IEM in 48% (n = 45), achalasia in 10% (n = 9), esophagogastric junction outflow obstruction (EGJOO) in 4% (n = 4), absent peristalsis in 2.5% (n = 3), distal esophageal spasm in 2% (n = 2), and jackhammer esophagus in 1% (n = 1). When the STM was carried out, the number of patients that could finish the test within 8 min was significantly lower, compared with the controls (Fig. 1) (range from 0% in IEM up to 33% in spastic disorders). The patients with EGJOO took the longest time to finish the test, and mean rice intake and rice intake per swallow were significantly lower in the patients with absent peristalsis < IEM < EGJOO < achalasia < spastic disorders < HC (p < 0.05) (Table 2).
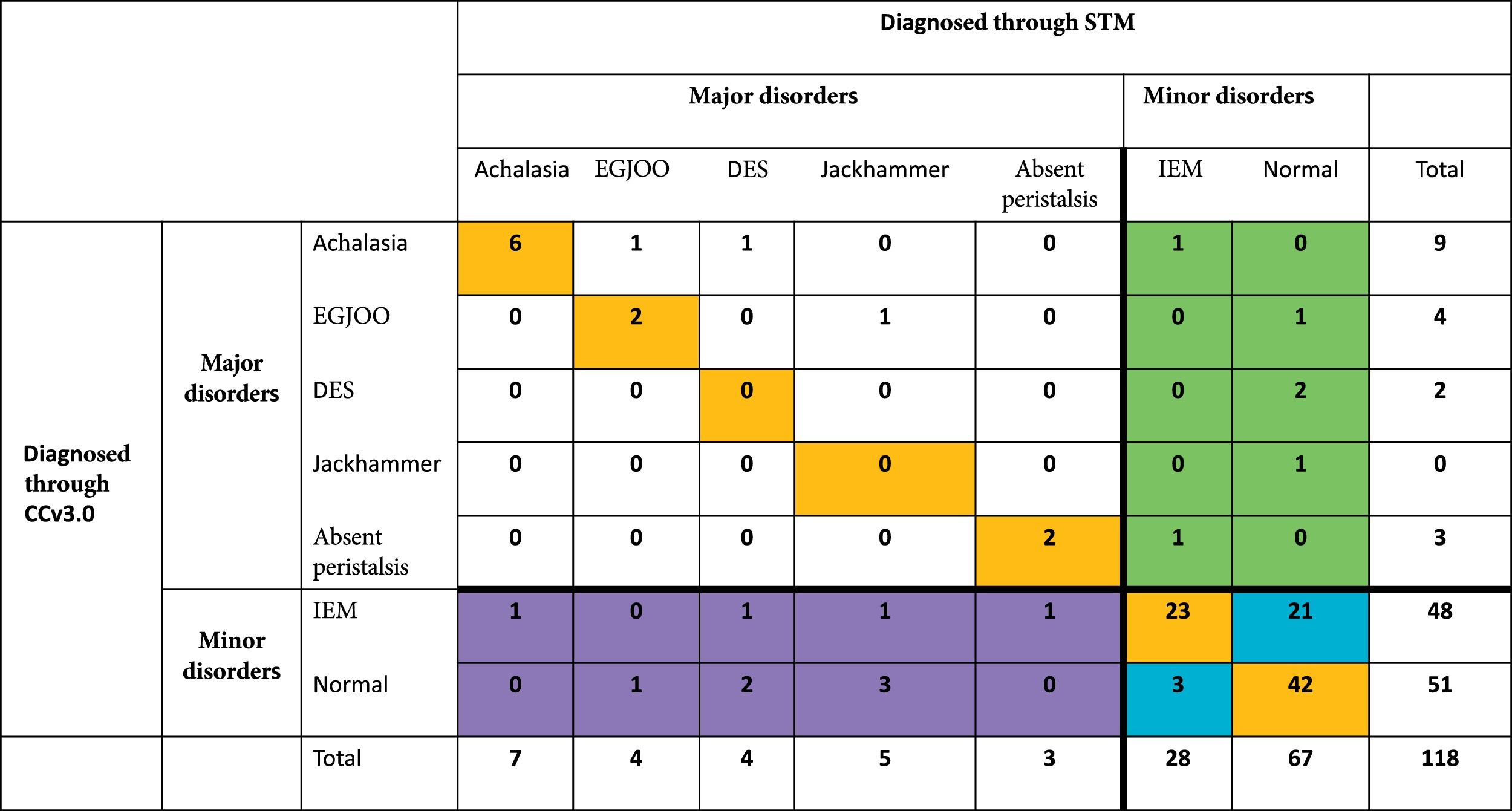
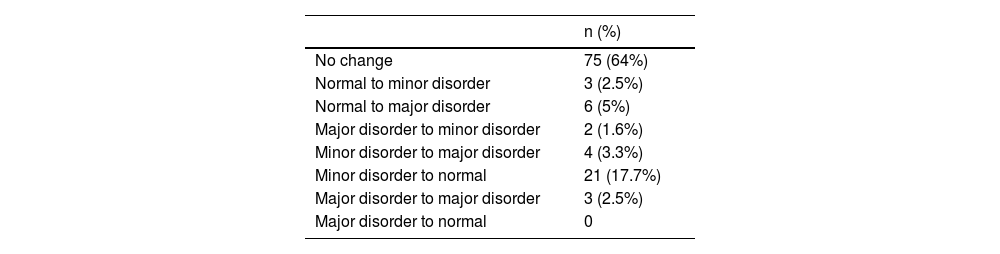
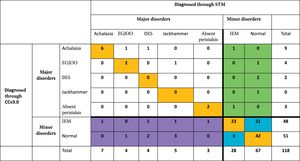
The general agreement between the diagnosis based on the conventional CCv3.0 protocol and the diagnosis with the STM was adequate (κ = 0.635, p = ≤0.0001) (Fig. 2). Thus, the STM changed the manometric diagnosis in 38% (n = 45) of the cases. More major motor disorders were diagnosed with the STM than with the CCv3.0 (23/118 [19.1%] vs. 19/118, [16.1%], p = 0.45). Considering that the number of major disorders increased from 19 to 23, their percentage of increase was 21% (4/19). Importantly, 6 patients whose HREM had been normal (3 with chest pain, 2 with dysphagia, and one with heartburn) (Fig. 2) changed to a major disorder with the STM. In addition, more cases of jackhammer esophagus were diagnosed with the STM, compared with the conventional CCv3.0 protocol (n = 5 vs. n = 1; 3 patients with chest pain, one with dysphagia, and one with heartburn), as well as more cases of distal esophageal spasm (DES) (n = 4 vs. n = 2; 3 patients with chest pain and one with heartburn). Of the 43% of the IEM cases (21/48) diagnosed through the CCv3.0, the STM revealed normal esophageal peristalsis (11 asymptomatic subjects, 8 patients with heartburn/regurgitation, and 2 with dysphagia). The main symptom in all the patients diagnosed with achalasia through the CCv4.0 was dysphagia. Table 3 shows the number and percentages of patients whose category of motor disorder type changed after the STM.
Diagnostic agreement between the conventional protocol (Chicago classification version 3.0) and the solid test meal.
CCv3.0: Chicago classification version 3.0; DES: distal esophageal spasm; EGJOO: esophagogastric junction outflow obstruction; IEM: ineffective esophageal motility; STM: solid test meal.
Percentage of change in diagnoses after the solid test meal.
| n (%) | |
|---|---|
| No change | 75 (64%) |
| Normal to minor disorder | 3 (2.5%) |
| Normal to major disorder | 6 (5%) |
| Major disorder to minor disorder | 2 (1.6%) |
| Minor disorder to major disorder | 4 (3.3%) |
| Minor disorder to normal | 21 (17.7%) |
| Major disorder to major disorder | 3 (2.5%) |
| Major disorder to normal | 0 |
Our study confirms the fact that the performance of complementary STM during the HREM protocol adds information and enables a more physiologic evaluation of esophageal motor function to be carried out, compared with LSs, in patients with esophageal motor disorders.
In addition, it provides the first determination of normal STM values in a Latin American population derived from the evaluation of a group of healthy volunteers. At present, there are only two studies for establishing STM parameters (n = 10 and n = 75) and they are conducted by the same group of authors.9,15 The need to conduct a study on normal values in a Latin American population arose from the fact that recent studies have shown that the results of tests for evaluating esophageal function (manometry, pH impedance, etc.) performed on asymptomatic subjects vary, depending on the system used, ethnic characteristics (region of the world), and behavioral characteristics, such as dietary patterns.16,17 According to our results in HCs, the percentage of healthy subjects that were able to completely finish the STM was above 90%, the same as reported by Hollenstein et al.,9 with similar parameter values. In our group of control subjects, just as in European populations, rice intake time was significantly shorter than in the patients with esophageal motor disorders, whereas rice intake quantity was higher. As reported in other studies utilizing the CCv3.0 in healthy subjects, up to 12% of those asymptomatic subjects were classified as having IEM, but interestingly, they were all reclassified as normal through the STM. Those findings are useful because the parameters described show that the STM can distinguish healthy subjects from those with esophageal motor diseases.
As in previous studies conducted on patients, our study showed that the STM changed the manometric diagnoses up to 38%, similar to the 32% reported by Araujo et al.11 The increase in the diagnostic yield of that maneuver signifies that it enabled up to 21% more major esophageal disorders to be diagnosed and up to 43% of IEM patients to be regarded as normal, according to the CCv3.0. In particular, the number of detected cases of DES doubled and the number of cases of jackhammer esophagus quadrupled, two disorders with sudden onset symptoms. The majority of those patients were evaluated for chest pain of presumed esophageal origin. The greater prevalence of esophageal motor disorders during the STM could have been due to the fact that during the LSs, the distension of the esophageal wall was not sufficient for triggering symptoms, but the rice swallows were, given that they are a challenge for the esophagus.
Regarding the patients previously diagnosed with IEM and described as normal after the STM, our results also are similar to those reported in previous studies (up to 37% in the study by Araujo et al.11). That finding confirms the prior observations that IEM diagnosis, even before the appearance of the CCv4.0, could be questioned or considered irrelevant in asymptomatic subjects, or in subjects with symptoms different from dysphagia. As with the challenge tests suggested by the CCv4.0, the STM could be helpful in daily practice for identifying patients with clinically relevant IEM.
Even though our results are interesting and consistent with those of other studies, it is important to comment on our study’s limitations, such as the small sample size (especially of the HCs) and reference bias. Having more data from a healthy population would increase the accuracy of the normal value ranges. In addition, the protocol proposed by the CCv4.0 could not be applied, given that it was published after our study was conducted, as well as the fact that, at present, it is difficult to clinically distinguish which primary position the STM should challenge. Without a doubt, studies comparing the STM and the updated CCv4.0 protocol are needed.
ConclusionIn our study population, the performance of the STM during the habitual HREM protocol, especially in patients with esophageal motor disorders, provided clinically relevant information that reclassified diagnoses made through the conventional protocol in up to one-third of the subjects, demonstrating that STM provides a more physiologic evaluation of esophageal function.
Financial disclosureNo financial support was received in relation to this study.
Conflict of interestDr. José María Remes-Troche is a member of the advisory board of Takeda, Alfasigma, Biocodex, and Asofarma. He has received speaker honoraria from Takeda, Chinoin, Ferrer, and Alfasigma. Dr. Mercedes Amieva-Balmori has received honoraria from Chinoin, Ferrer, and Takeda. The rest of the authors declare they have no conflict of interest.