Today, antireflux surgery has an established position in the management of gastroesophageal reflux disease. Some case series have shown good short-term results, but there is still little information regarding long-term results. Studies have recently focused on evaluating residual symptomatology and its impact on quality of life.
ObjectivesTo determine the postoperative quality of life and degree of satisfaction in patients that underwent laparoscopic Nissen fundoplication.
Patients and methodsA total of 100 patients (59 women and 41 men) were studied after having undergone laparoscopic Nissen fundoplication. The variables analyzed were level of satisfaction, gastrointestinal quality of life index (GIQLI), residual symptoms, and the Visick scale.
ResultsNo variation was found in relation to sex; 49 men and 51 women participated in the study. The mean age was 49 years. The degree of satisfaction encountered was: satisfactory in 81 patients, moderate in 3, and bad in 2 patients. More than 90% of the patients would undergo the surgery again or recommend it. The Carlsson score showed improvement at the end of the study (p<0.05). In relation to the GIQLI, a median of 100.61 points±21.624 was obtained. Abdominal bloating, regurgitation, and early satiety were the most frequent residual symptoms. The effect on lifestyle measured by the Visick scale was excellent.
ConclusionsThe level of satisfaction and quality of life obtained were comparable with reported standards; and the residual symptoms after antireflux surgery were easily controlled.
La cirugía antirreflujo tiene actualmente un lugar establecido en el manejo de la enfermedad por reflujo gastroesofágico. Algunas series han revelado buenos resultados a corto plazo, pero los resultados a largo plazo permanecen aún poco conocidos. Recientemente, los estudios se han centrado en evaluar la sintomatología residual y su impacto en la calidad de vida.
ObjetivoDeterminar la calidad de vida en el postoperatorio y la satisfacción en pacientes intervenidos de funduplicatura de Nissen laparoscópica.
Pacientes y métodosSe estudió a 100 pacientes (59 mujeres y 41 hombres) postoperados de funduplicatura de Nissen laparoscópica. Las variables fueron grado de satisfacción, calidad de vida (GIQLI), síntomas residuales y escala Visick.
ResultadosNo se encontró variación en el sexo, siendo 49 hombres y 51 mujeres; el promedio de edad fue de 49 años. La valoración del grado de satisfacción fue: satisfactoria en 81 pacientes, moderada en 3 y mala en 2 pacientes. Más del 90% se sometería de nuevo o recomendaría la cirugía. En cuanto a la clasificación de Carlsson, se mostró mejoría al final del estudio (p<0.05). De acuerdo con el cuestionario GIQLI, se obtuvo una mediana de 100.61 puntos±21.624. Distensión abdominal, regurgitación y saciedad temprana fueron los síntomas residuales más frecuentes. La repercusión en el estilo de vida mediante escala de Visick fue excelente.
ConclusionesEl grado de satisfacción y la calidad de vida obtenidos son comparables con estándares reportados y los síntomas residuales son fácilmente controlables posterior a la cirugía antirreflujo.
Gastroesophageal reflux disease (GERD) was recognized as an important clinical problem in 1935 by Winklestein and it was identified as the cause of esophagitis by Allison in 1946.1,2 Surgery has an established position today in the management of GERD.3 The popularizing of anti-reflux surgery over the last few years, associated with the introduction of the laparoscopic technique and its advantages --a less traumatic and invasive approach and a rapid return to normal daily activities-- has led to the increased performance of laparoscopic fundoplication. This procedure has thus become established as the criterion standard in the surgical management of GERD.4,5
Studies have recently focused on evaluating the postoperative results, especially when there is residual symptomatology after surgery and its short-term impact on patient quality of life. The indicators of this latter status and the level of patient satisfaction are currently an important way of estimating the result of anti-reflux surgery, because gastroesophageal symptoms in the post-fundoplication patient have long been regarded as the equivalent of surgical failure.6,7
With this in mind, the aim of our study was to carry out a long-term evaluation of the results of Nissen fundoplication through the application of the following 4 questionnaires: the Gastrointestinal Quality of Life Index (GIQLI), the Dysphagia score, the Visual analog scale for dysphagia, and the Visick scale.
Patients and methodsIn our study we evaluated quality of life and residual symptomatology in a case series of 100 patients operated on within the time frame of February 2005 and December 2010. The specific aspects to be analyzed were:
- 1
Are the results of the laparoscopic Nissen fundoplication satisfactory for the patient?
- 2
The quality of life of the patient that underwent the laparoscopic Nissen fundoplication and its relation to the level of satisfaction.
- 3
Is symptom persistence frequent after anti-reflux surgery?
- 4
Is medication indispensable after the surgery?
Methods. One hundred patients were programmed to undergo laparoscopic floppy Nissen fundoplication. All the patients were operated on by the same surgical team; the surgical technique was standardized before the study and the internationally accepted standards were followed. Patient selection for surgical management was based on the guidelines established by the Mexican Consensus for the Study of GERD.8
The level of satisfaction, quality of life of the postoperative patients, and surgical morbidity were evaluated through standardized and validated questionnaires elaborated for that purpose. The Carlsson questionnaire was applied to all the patients in order to measure reflux intensity;9 quality of life was studied postoperatively through the GIQLI10 (an adequate, valid, and useful instrument for evaluating quality of life in patients presenting with reflux disease) because it includes specific questions about digestive symptoms and generic questions about physical, emotional, and social capacity. The questionnaire contains 36 items with an answer scale from 0 (the worst result) to 4 (the best result). Global scores above 86 were regarded as a satisfactory effect, even in the presence of residual symptoms. Dysphagia was evaluated with the Dysphagia score, the Analog scale for dysphagia,11 and the Visick grading system.12 The questionnaire dealing with the level of satisfaction and quality of life was applied to each patient that had a minimum 5-year postoperative period; it was applied verbally and the questions were asked by a researcher uninvolved in the surgical management. The level of satisfaction was evaluated nominally with the following questions: Would you accept being operated on again? Would you recommend the procedure to a friend or family member? The GIQLI was chosen because it is a validated questionnaire in Spanish. It consists of 36 questions divided into 5 sections, with a specific part for digestive diseases. Scoring and the visual analog for dysphagia were measured through validated scoring scales, whereas the Visick scale was measured ordinally.
Statistical analysis. An intention-to-treat analysis was done and descriptive statistics of means, standard deviation, medians, and percentages were employed. The proportion comparison was carried out with the chi-square test and the mean and median comparison with the Student's t test or the Mann-Whitney U test (for equal or different variances, respectively). The questionnaire was analyzed using the Student's t test and the group analysis was done with a variance analysis for both the overall results and those of each of its sections. A 95% confidence interval (CI) was used and statistical significance was set at a p<0.05. The study was approved by the Research Committee of the Hospital General de Zona No. 1 del IMSS in Colima.
ResultsFrom February 2005 to December 2010, 100 patients (59 women and 41 men) that were operated on due to GERD were studied. Fourteen patients were excluded from the final analysis for the following reasons: 10 had a different address at the time of the interview and 4 refused to answer the questionnaire. The mean follow-up of the remaining patients was 5±0.5 years. The overall follow-up rate at 5 years for the 100 patients was 82%. The mean length of time the patients remained hospitalized after surgery was 18±8.7h. There were no conversions and no deaths.
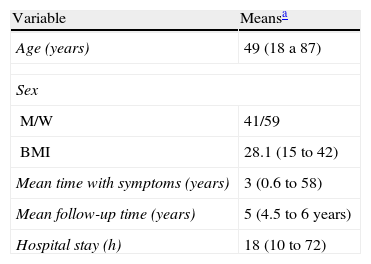
Distribution by sex was 49 men and 51 women. The age range was 18 to 87 years and the mean body mass index was 28.33±4.49. The characteristics of the patient population upon hospital admission are shown in Table 1.
Demographic characteristics of 100 patients that underwent laparoscopic Nissen fundoplication.
| Variable | Meansa |
| Age (years) | 49 (18 a 87) |
| Sex | |
| M/W | 41/59 |
| BMI | 28.1 (15 to 42) |
| Mean time with symptoms (years) | 3 (0.6 to 58) |
| Mean follow-up time (years) | 5 (4.5 to 6 years) |
| Hospital stay (h) | 18 (10 to 72) |
BMI: Body mass index; M/W: men/women.
In general, the level of satisfaction of the patients that underwent the surgery was classified as totally satisfied in 75 patients and good in 3 patients (78% with good to excellent results). As to whether they would undergo surgical treatment again or recommend it to a friend considering such treatment, the answer was affirmative in 90% and 96% of the cases, respectively.
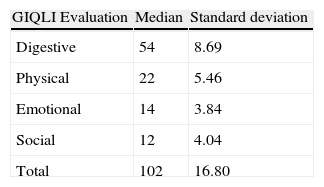
Quality of lifeThe results of the quality of life evaluation in 85 patients interviewed with the GIQLI were previously validated in 35 subjects.
The overall quality of life analysis showed an acceptable level after surgery (a score of 102±16.8). This level was more obvious in the group corresponding to the digestive, physical, emotional, and social activities. Table 2 shows both the total and separate GIQLI scores per function area.
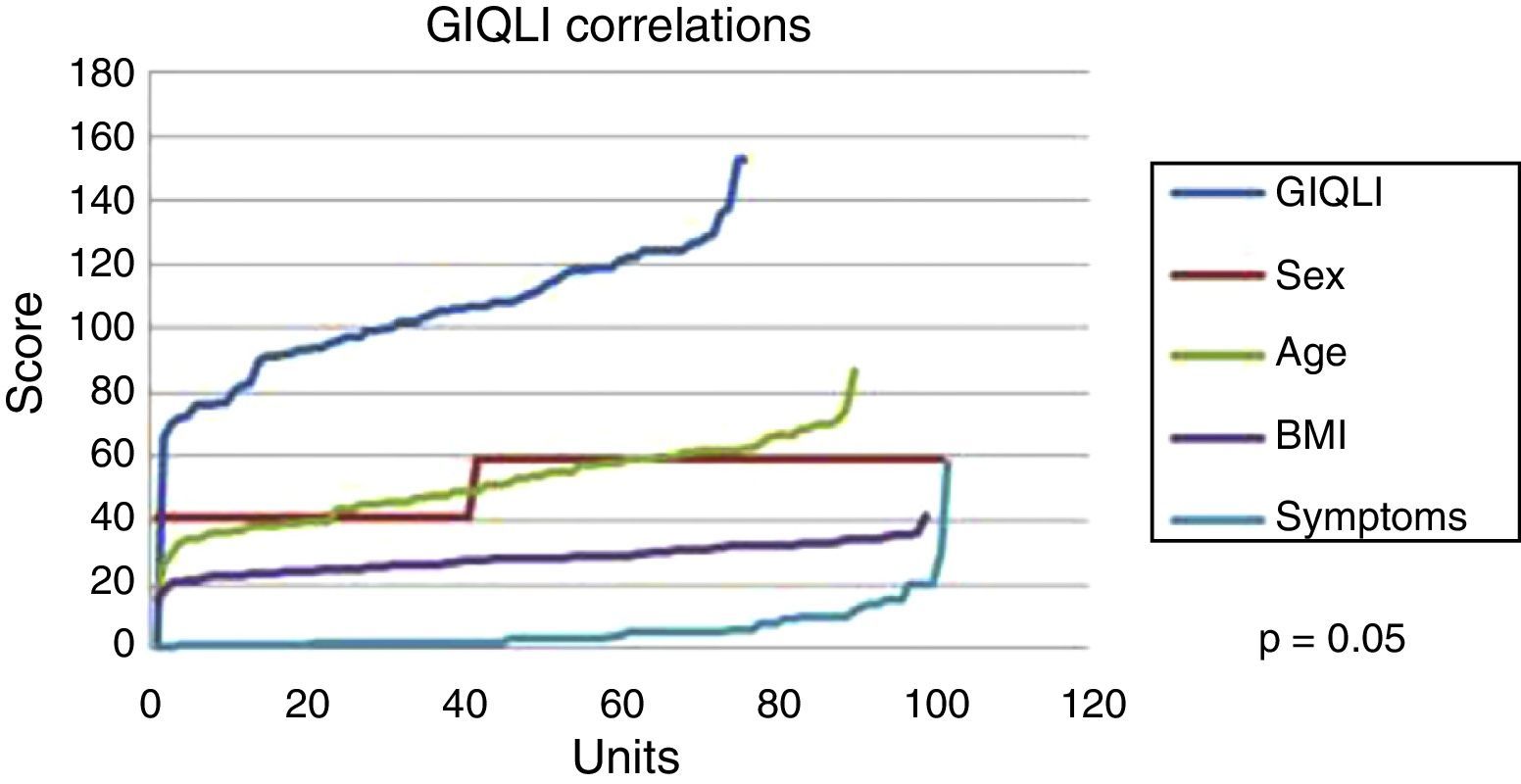
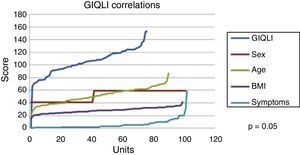
Figure 1 shows the correlation of the GIQLI score with sex, age, BMI, and symptoms; the scores remained the same throughout the follow-up and there were no statistically significant differences among the slopes of the curves (p=0.50).
Symptom evaluationThe mean scores of the Carlsson questionnaire for the preoperative and the postoperative groups were 7.8±3.4 and 3.5±3.1, respectively: these differences were statistically significant (p<0.05).
We found the following residual symptoms that presented in the postoperative period: abdominal bloating in 24 patients (27.5%), regurgitation in 16 patients (18.3%), and early satiety in 16 patients (18.3%). Other less frequent residual symptoms were: odynophagia in 7 patients (8%), burping in 4 patients (4.5%), temporary dysphagia in 2 patients (2.29%), nausea and vomiting in 2 patients (2.29%), and cough in one patient (1.1%). There was an absence of residual symptoms in 15 patients (17.24%).
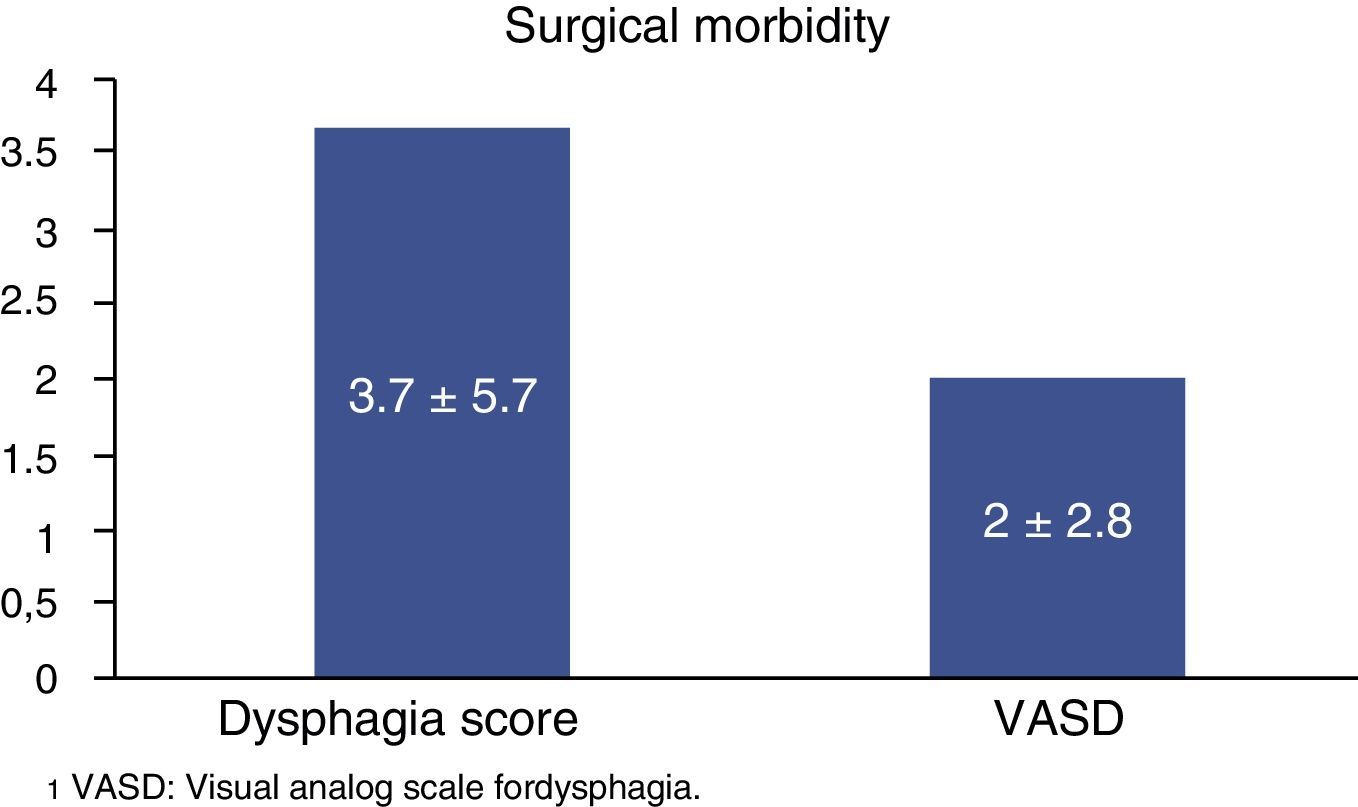
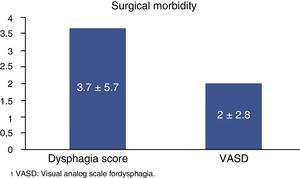
Figure 2 summarizes the dysphagia score in a range of 0 to 24 points, and the Visual analog scale in a range of 0 to 10 points in patients that underwent laparoscopic Nissen fundoplication; this was carried out at the fifth year of follow-up.
Forty-seven percent of the patients resorted to medication for symptoms, whereas 53% did not. The results were considered very good or good in 89.3% of the patients that took their accustomed amount of medication or less, whereas the response was regarded as poor in only 10.3% of the patients that had to take a larger quantity of medication.
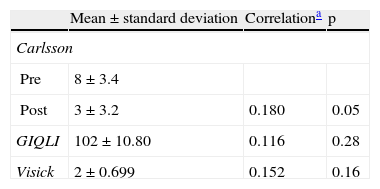
In general, the effect on lifestyle after the surgery–measured through the Visick grading system–was considered to be: excellent (Visick 1) in 19 (21.8%) patients and good (Visick 2) in 50 (57.4%) patients; 14 patients had moderate uncontrolled symptoms, but they did not interfere with their socioeconomic life (Visick 3); and 2 patients presented with moderate symptoms that interfered with their socioeconomic life (Visick 4). The correlation results of the preoperative and postoperative Carlsson questionnaire, the GIQLI, and the Visick grading system are shown in Table 3.
Correlations according to the preoperative and postoperative Carlsson questionnaire GIQLI questionnaire, and Visick scoring system.
| Mean±standard deviation | Correlationa | p | |
| Carlsson | |||
| Pre | 8±3.4 | ||
| Post | 3±3.2 | 0.180 | 0.05 |
| GIQLI | 102±10.80 | 0.116 | 0.28 |
| Visick | 2±0.699 | 0.152 | 0.16 |
Units: GIQLI (score), Sex (M/W), Age (years), BMI (score), Symptoms (nn).
GERD is responsible for 75% of the manifestations that present in the esophagus, causing symptoms or complications at this level and in the respiratory tract, as well as affecting the nutritional status. Various associated factors have been reported, such as the antireflux barrier, aggressive factors (acids, pepsin, bile, pancreatic enzymes, etc.), and defensive factors (esophageal acid clearance). Since the introduction of laparoscopy for treating gastroesophageal reflux, its use has rapidly extended and it is now accepted as the treatment of choice for that condition.13
Today the result of an antireflux procedure not only takes the degree of technical success into account, but also recognizes the relevance of the patient's perspective. The determination of the overall results that control the balance between the technical result and the patient's perspective are, without a doubt, what will define the concept of surgical failure.
Our results, at least at 5 years after the surgical procedure, show that 78% of the patients that underwent laparoscopic Nissen fundoplication were highly satisfied with their status and would repeat their decision to have the procedure or would recommend it to a friend considering such treatment. Similar conclusions in case series were reported by Dallemagne,14 Kelly,15 and Bloomston,16 adding to our result relevance. Likewise, Diaz-de Liaño17 previously reported a mean level of satisfaction of 8.1 in relation to a maximum of 10, with a satisfied patient percentage between 85 and 95%. Our patients presented with a level of satisfaction of 8.44 and 78% of the results were good to excellent.
Up to now, the aims of antireflux surgery have been to attenuate reflux symptoms with a minimum of risk and without adding long-term secondary effects. The health status of the population and subsequent disability have become the cornerstones of study on the part of clinical research investigators. The health perspective manifested by the patient in his or her biopsychosocial environment through specific or generic surveys is currently very relevant. Like Poves,18 we felt that the GIQLI, which was prepared in Germany, was validated in France for digestive pathologies, and then a validated version in Spanish was developed for reflux,10 can provide general, specific, and biopsychosocial information on the quality of life of the patient.
Our study included 84 patients that had been operated on and that had a mean follow-up period of 5 years. This made it possible to unquestionably demonstrate good quality of life after surgery (100.61), contrasting the values in normal subjects, as shown in the findings of Araujo Teixeira et al.19 and Dallemagne et al.14
At 6 months after surgery, the evaluated patients have had results similar to those reported in normal subjects, and an improved quality of life in relation to the physical and emotional statuses that had been confirmed by Araujo Teixeira.19 These results were maintained for the remainder of the period of observation, with the exception of the digestive activities. Similar results have been reported by numerous authors14,20 and they are attributed to specific residual symptoms, such as abdominal bloating, regurgitation, and early satiety.
Although the success of antireflux surgery is evaluated by symptom control, the presence and intensity of potential secondary effects, manifested by residual symptomatology, is often interpreted as failure. Nevertheless, the concepts of improvement are of vital significance in today's health environment, and could be the most important parameters for evaluating the effectiveness of surgical treatment. In our study, as in others,6,21 these manifestations were evaluated at 6 months after surgery, and despite the initial discomfort, no effect on quality of life data was found. No patients were documented with having severe dysphagia or its persistence 6 months after surgery. At present there is no explanation for the higher percentage of postoperative abdominal bloating.
Some patients continue to take medication despite the disappearance of all their reflux symptoms as a result of the surgery. The gradual increase over time in the use of antireflux medication could be partially due to a low, but continuous, risk for reflux recurrence. However, the reflux recurrence rate is probably lower than what the consumption of medication suggests, given that only 24% of the patients that continue taking antireflux medication after fundoplication actually present with reflux when they submit to a 24-hour pH-metry test.15,16 In our case series, 47% of the patients continued taking antireflux medication. This is considerably less than the 62% reported by Spechler.22
Other reports using the modified Visick classification had results similar to those of our study,20,23 in which grades I and II normally are regarded as a satisfactory result and correlate very well with acidity symptoms.
The evaluation of quality of life has always played a central, albeit at times subtle, role in the therapeutic aims of medicine. The majority of surgical procedures concentrate on the correction of physiologic or anatomic disorders that lead to a disease process. However, results of these procedures have little impact from the patients’ viewpoint and the recovery of quality of life becomes the mainstay of their satisfaction. This is why we decided to use both generic and specific evaluation instruments.
We therefore conclude that in general, and in agreement with prior publications,17,19,20,24 the evaluations showed important improvement in quality of life, according to the instruments employed.
Financial disclosureNo financial support was received in relation to this article.
Conflict of interestThe authors declare that there is no conflict of interest.
Please cite this article as: Prieto-Díaz-Chávez E, Medina-Chávez JL, Brizuela-Araujo CA, et al. Calidad de vida y grado de satisfacción de pacientes postoperados de funduplicatura de Nissen laparoscópica. Revista de Gastroenterología de México. 2014;79:73–78.