Inflammatory fibroid polyp (lFP) is a rare, benign, and solitary neoplasm predominantly located in the gastric antrum and small bowel. Its clinical symptoms are heterogeneous and essentially depend on the location and size of the tumor. Definitive diagnosis is made through histopathology and this pathology has excellent long-term prognosis.
AimTo identify the cases of IFP seen at the Instituto Nacional de Ciencias Médicas y Nutrición Salvador Zubirán over a 10-year period.
MethodsA retrospective, cross-sectional, descriptive, and observational study was conducted that included patients with histopathologic diagnosis of IFP within the time frame of January 2001 and December 2011.
ResultsSix cases were found and 5/6 (83.3%) of them were women. The median age was 41 years (minimum-maximum range of 19-56 years). The most frequent symptoms were weight loss (n=3), fever (n=2), nausea (n=2), and vomiting (n=2). Three patients presented with iron deficiency anemia and 2 cases with intussusception. The IFPs were located at the following sites: esophagus (n=1), stomach (n=2), small bowel (n=2), and colon (n=1). Treatment was surgical in 5/6 (83.3%) of the patients.
ConclusionsIFPs are extremely rare in our population. They usually present with weight loss and iron deficiency anemia and are more frequently located in the stomach and small bowel. This is the largest reported IFP case series in a Mexican population.
El pólipo fibroideo inflamatorio (PFI) es una neoplasia rara, benigna y solitaria, predomina en el antro gástrico y el intestino delgado. Los síntomas clínicos son heterogéneos, dependen fundamentalmente de la localización y el tamaño del tumor. El diagnóstico definitivo se establece mediante histopatología y su pronóstico es excelente a largo plazo.
ObjetivoIdentificar los casos de PFI en el Instituto Nacional de Ciencias Médicas y Nutrición Salvador Zubirán en un período de 10 años.
MétodosEstudio observacional, descriptivo, transversal y retrospectivo, se incluyó a los pacientes con diagnóstico histopatológico de PFI desde enero del 2001 hasta diciembre del 2011.
ResultadosSe encontraron 6 casos, 5/6 (83.3%) fueron mujeres. La mediana de edad fue de 41 años (rango mínimo-máximo de 19 a 56 años). Los síntomas más frecuentes fueron pérdida de peso (n=3), fiebre (n=2), náuseas (n=2) y vómito (n=2). Tres pacientes cursaron con anemia ferropénica. Dos casos se presentaron con intususcepción. La localización de los PFI fue la siguiente: esófago (n=1), estómago (n=2), intestino delgado (n=2) y colon (n=1). El tratamiento fue quirúrgico en 5/6 (83.3%) pacientes.
ConclusionesLos PFI son extremadamente raros en nuestra población, suelen presentarse con pérdida de peso y anemia ferropénica, se localizan con mayor frecuencia en el estómago y el intestino delgado. Esta es la serie de casos más grande de PFI que se ha reportado en población mexicana.
Inflammatory fibroid polyp (IFP) is a rare, benign, and solitary neoplasm initially described by Vanek in 1949 as a submucosal gastric granuloma with eosinophilia.1 Helwig and Ranier proposed the term IFP in 1953.2 Its incidence is extremely low (0.1%) and usually presents in the sixth and seventh decades of life. It is slightly more frequent in the male sex.2,3 IFPs predominate in the gastric antrum and small bowel.2,4,5 Its etiology is unknown, but some authors suggest that it is an allergic reaction due to the presence of eosinophils. However, other factors have been implicated, such as neural hyperplasia, irritants, trauma, genetic alterations, and bacterial, physical, or chemical stimulants.2 Activating mutations in the platelet-derived growth factor receptor alpha (PDGFRA) gene have been associated with the development of IFPs and of gastrointestinal stromal tumor (GIST), showing a similar physiopathogenesis between these 2 neoplasms and lending support to the theory of a neoplastic IFP origin.6,7 Mutations have been documented in 21.7 to 69.6% of the cases.8 The clinical symptoms are heterogeneous and essentially depend on the location and size of the tumor.9,10
The definitive diagnosis is made through histopathology.11–13 Currently, the majority of cases can be treated with polypectomy, with the rest requiring surgical treatment, and the long-term prognosis is excellent.14
The aim of this study was to identify the cases of IFP seen at the Instituto Nacional de Ciencias Médicas y Nutrición Salvador Zubirán (INCMNSZ) over a period of 10 years.
MethodsA retrospective, cross-sectional, descriptive, and observational study was conducted at the INCMNSZ and included patients with a histopathologic diagnosis of IFP within the time frame of January 2001 and December 2011. The demographic variables, clinical manifestations, laboratory and imaging studies, and clinical progression of the patients were obtained from the clinical case records.
The descriptive statistics included frequencies for the categorical variables and medians and minimum-maximum range for the continuous variables. The SPSS version 20.0 statistical program was utilized (Chicago, Illinois, USA).
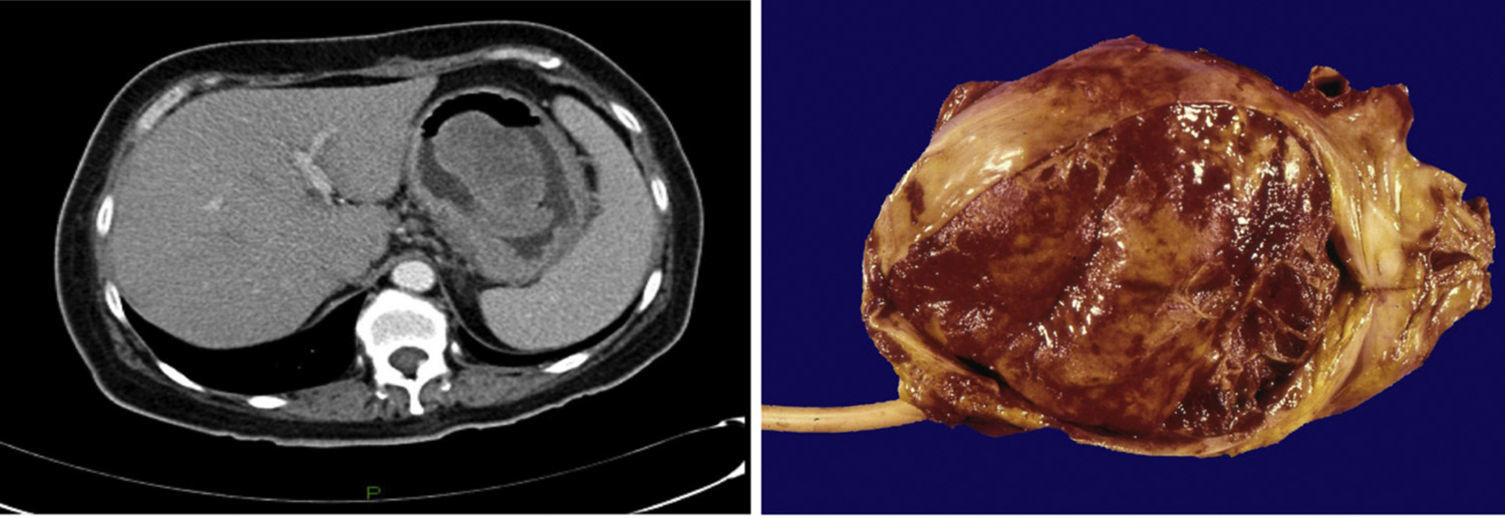
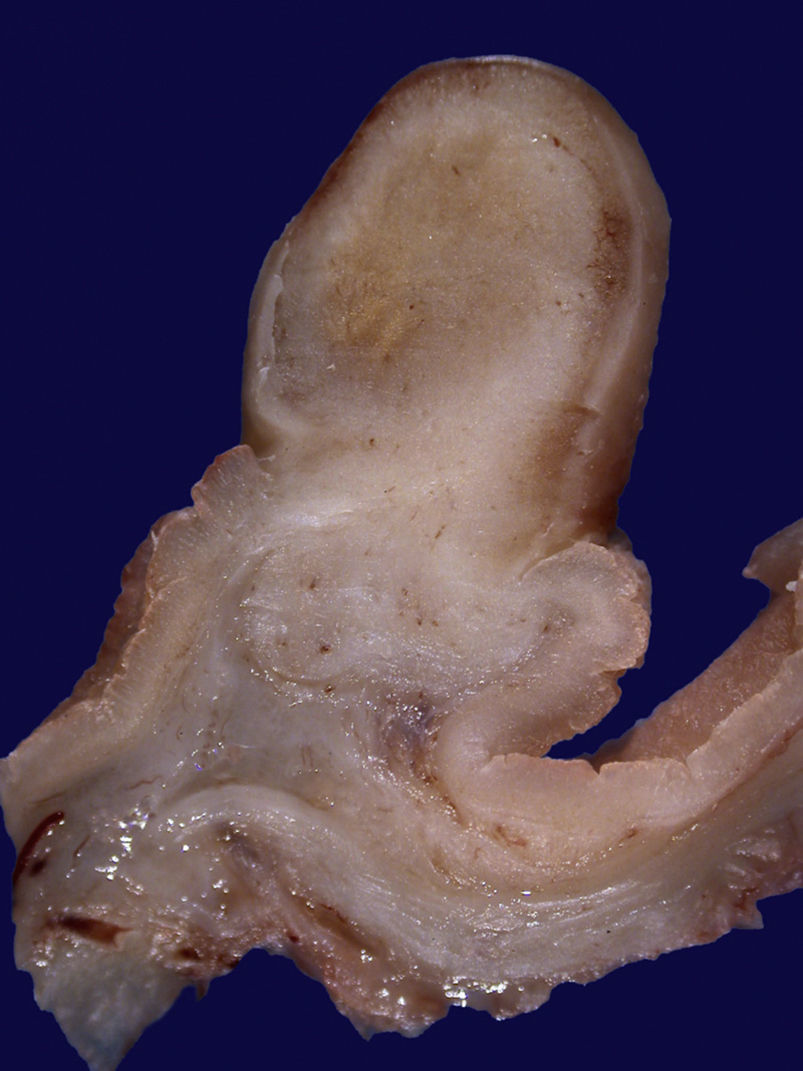
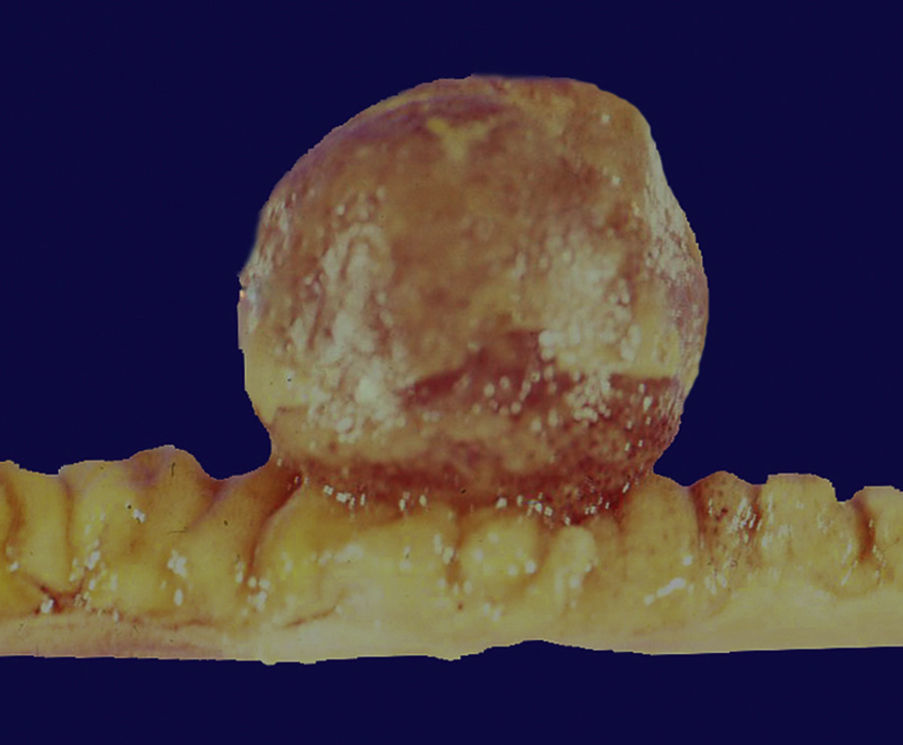
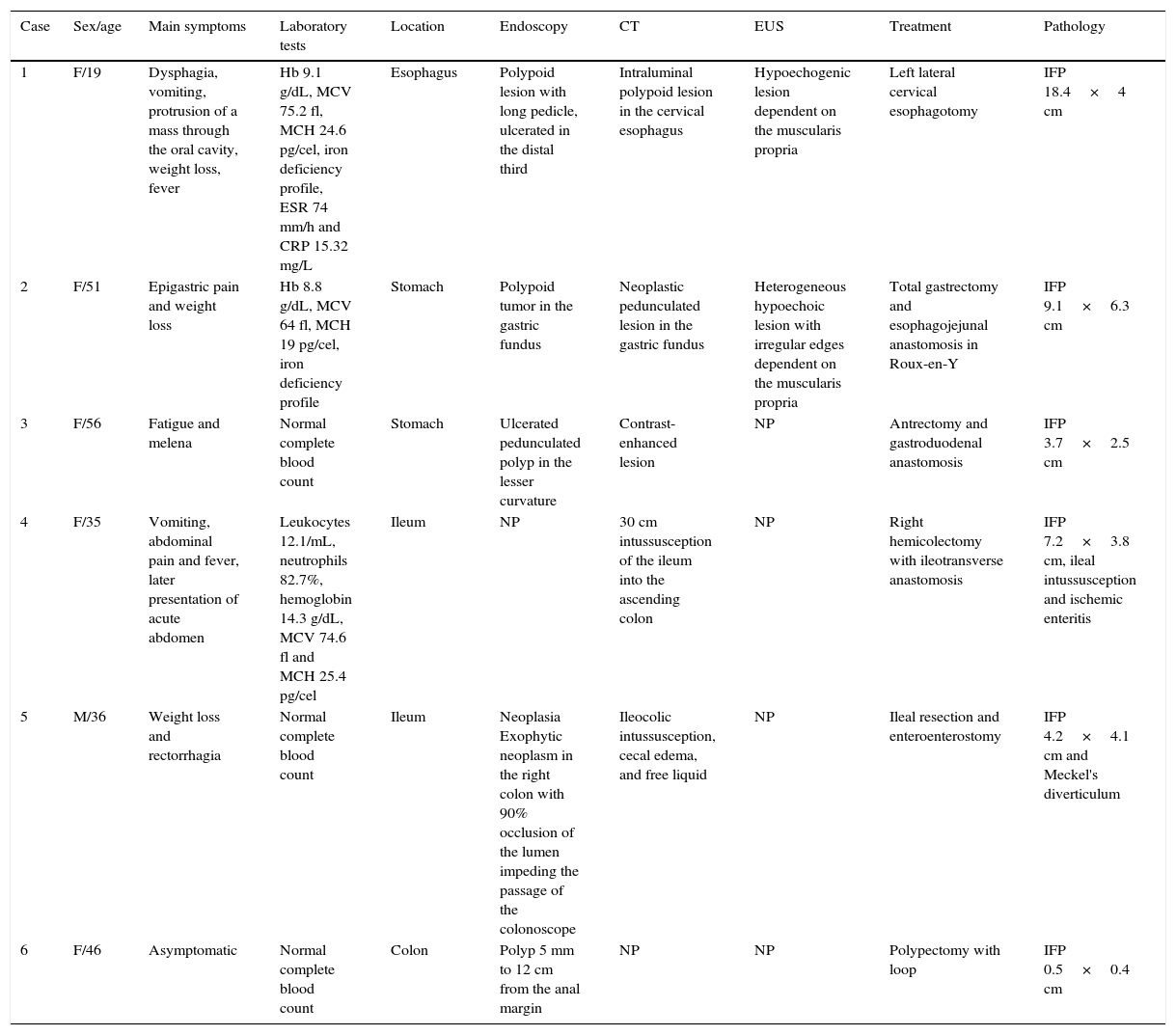
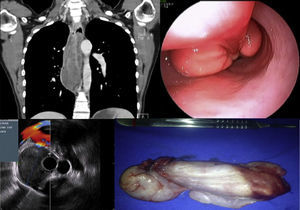
ResultsSix cases of IFP were found and 5/6 (83.3%) of them were in women. The median age was 41 years (minimum-maximum range of 19 to 56 years). The most frequent symptoms were weight loss (n = 3), fever (n = 2), nausea (n = 2), and vomiting (n = 2). Three patients presented with iron deficiency anemia and 2 with intussusception. The mean symptom duration was 7 months (range of 0 to 12 months). The IFPs had the following locations: esophagus (n = 1), stomach (n = 2), small bowel (n = 2), and colon (n = 1). The approach was carried out through panendoscopy (n = 3), colonoscopy (n = 2), computed tomography (n = 5), and endoscopic ultrasound (n = 2). Treatment was surgical in 5/6 (83.3%) of the patients, and only one case required loop polypectomy. At the follow-up (median 51 months) all patients were alive and asymptomatic (table 1) (figs. 1–6).
Inflammatory fibroid polyps.
| Case | Sex/age | Main symptoms | Laboratory tests | Location | Endoscopy | CT | EUS | Treatment | Pathology |
|---|---|---|---|---|---|---|---|---|---|
| 1 | F/19 | Dysphagia, vomiting, protrusion of a mass through the oral cavity, weight loss, fever | Hb 9.1 g/dL, MCV 75.2 fl, MCH 24.6 pg/cel, iron deficiency profile, ESR 74 mm/h and CRP 15.32 mg/L | Esophagus | Polypoid lesion with long pedicle, ulcerated in the distal third | Intraluminal polypoid lesion in the cervical esophagus | Hypoechogenic lesion dependent on the muscularis propria | Left lateral cervical esophagotomy | IFP 18.4×4 cm |
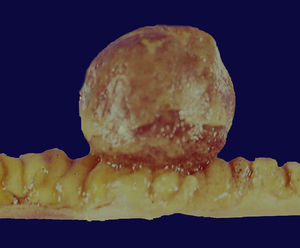
| 2 | F/51 | Epigastric pain and weight loss | Hb 8.8 g/dL, MCV 64 fl, MCH 19 pg/cel, iron deficiency profile | Stomach | Polypoid tumor in the gastric fundus | Neoplastic pedunculated lesion in the gastric fundus | Heterogeneous hypoechoic lesion with irregular edges dependent on the muscularis propria | Total gastrectomy and esophagojejunal anastomosis in Roux-en-Y | IFP 9.1×6.3 cm |
| 3 | F/56 | Fatigue and melena | Normal complete blood count | Stomach | Ulcerated pedunculated polyp in the lesser curvature | Contrast-enhanced lesion | NP | Antrectomy and gastroduodenal anastomosis | IFP 3.7×2.5 cm |
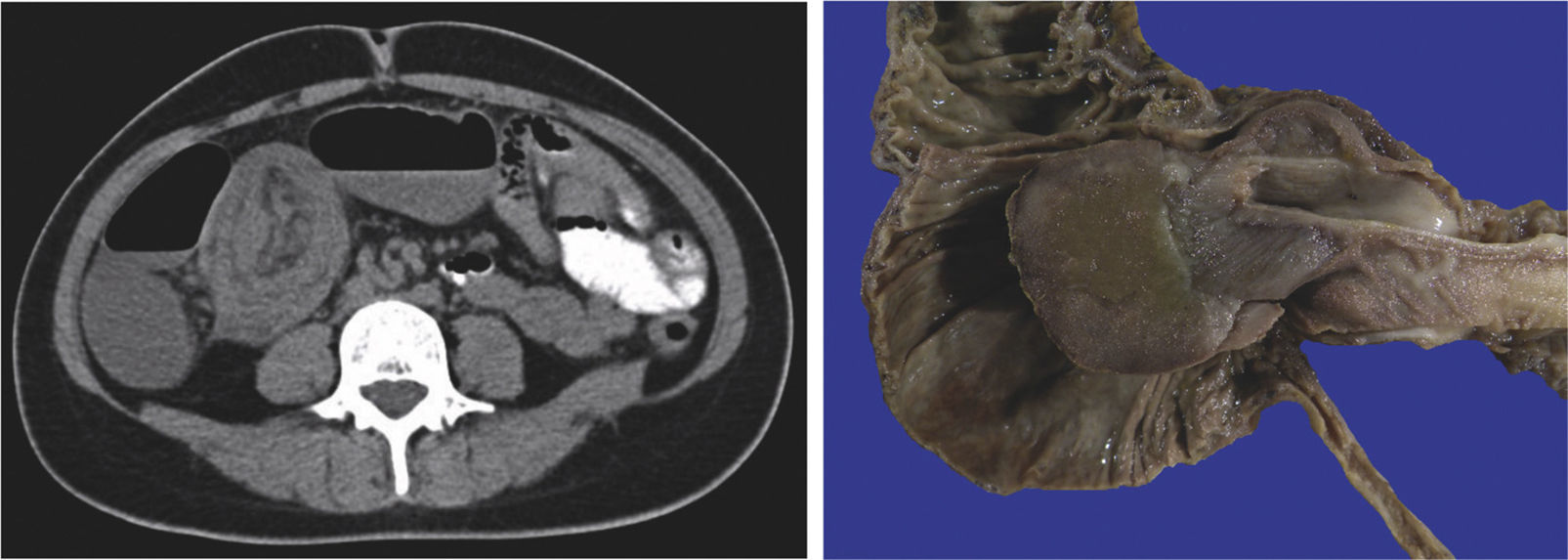
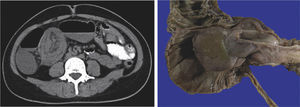
| 4 | F/35 | Vomiting, abdominal pain and fever, later presentation of acute abdomen | Leukocytes 12.1/mL, neutrophils 82.7%, hemoglobin 14.3 g/dL, MCV 74.6 fl and MCH 25.4 pg/cel | Ileum | NP | 30 cm intussusception of the ileum into the ascending colon | NP | Right hemicolectomy with ileotransverse anastomosis | IFP 7.2×3.8 cm, ileal intussusception and ischemic enteritis |
| 5 | M/36 | Weight loss and rectorrhagia | Normal complete blood count | Ileum | Neoplasia Exophytic neoplasm in the right colon with 90% occlusion of the lumen impeding the passage of the colonoscope | Ileocolic intussusception, cecal edema, and free liquid | NP | Ileal resection and enteroenterostomy | IFP 4.2×4.1 cm and Meckel's diverticulum |
| 6 | F/46 | Asymptomatic | Normal complete blood count | Colon | Polyp 5 mm to 12 cm from the anal margin | NP | NP | Polypectomy with loop | IFP 0.5×0.4 cm |
CT: Computed tomography; EUS: Endoscopic ultrasound; IFP: Inflammatory fibroid polyp; NP: Not performed
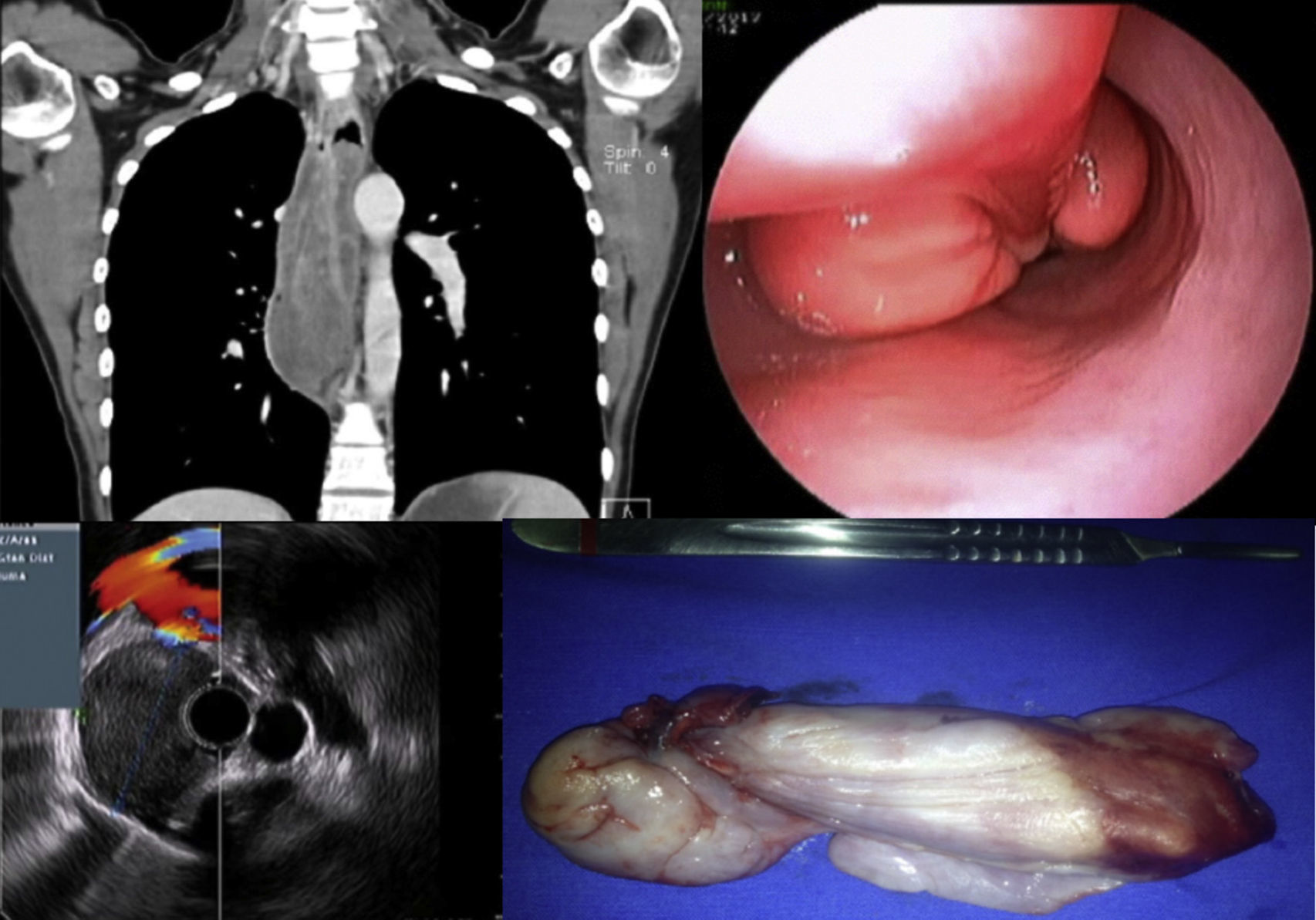
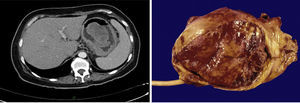
Case 1. The chest CT reported an intraluminal polypoid lesion dependent on the cervical esophagus. Panendoscopy revealed a polypoid lesion with a long pedicle. Endoscopic ultrasound showed a hypoechogenic lesion dependent on the muscularis propria layer. The surgical specimen reported IFP.
IFP is an extremely rare neoplasm. At the tertiary care INCMNSZ hospital only 6 cases were found over a 10-year period (2001-2011). Our results differ from those reported in the international literature in relation to the age of presentation and sex of the patients. The median age was 41 years and 83.3% of the patients were women.
IFPs are more frequent in the gastric antrum (66-75%), small bowel (18-20%), specifically in the ileum, colon (4-7%), gallbladder (1%), esophagus (1%), duodenum (1%), and appendix (<1%).1,4,5 In our study, the most frequent locations were the stomach (33.3%) and ileum (33.3%), followed by the esophagus (16.6%) and colon (16.6%).
The majority of IFPs are reported to be asymptomatic and their diagnoses are made through incidental endoscopic findings.1 However, in our case series, 5/6 (83.3%) of the patients presented with symptoms. Clinical symptoms tend to be heterogeneous and essentially depend on tumor location and size. The most frequent symptoms are abdominal pain (54%), bleeding (33%), and anemia (17%).9,10 Gastric polyps can produce pyloric obstruction or anemia, whereas those located in the small bowel present with obstruction or intussusception.1 Dysphagia is the most common symptom of IFP in the esophagus, followed by gastrointestinal bleeding due to erosions and ulcers on the surface of the polyp. There are reports of cases of regurgitation of the mass and food, as well as asphyxia.15 Fever is attributed to the effect of cytokines released from the inflammatory cells of the IFP.16 In our study, the most frequent symptoms were weight loss (n = 3), fever (n = 2), nausea (n = 2), and vomiting (n = 2). Three patients presented with iron deficiency anemia and there were 2 cases of intussusception. In 3/6 (50%) of our cases, endoscopy revealed submucosal, polypoid, intraluminal, and pedunculated lesions, which frequently have an ulcerated surface. These tumors usually measure 2 to 5cm at the time of diagnosis.4 Our results reported a median of 5.7cm in diameter. Computed tomography is considered the most sensitive radiologic method for diagnosing the polyp or its complications.13 Nevertheless, endoscopic ultrasound is an excellent method for the detailed anatomic description of the tumor. The most common ultrasound pattern is that of a hypoechogenic, homogeneous, non-encapsulated lesion with poorly defined margins located in the second and/or third echo layer of the gastrointestinal wall.12 Endoscopic ultrasound also provides information on the vascularity of the polyp.13
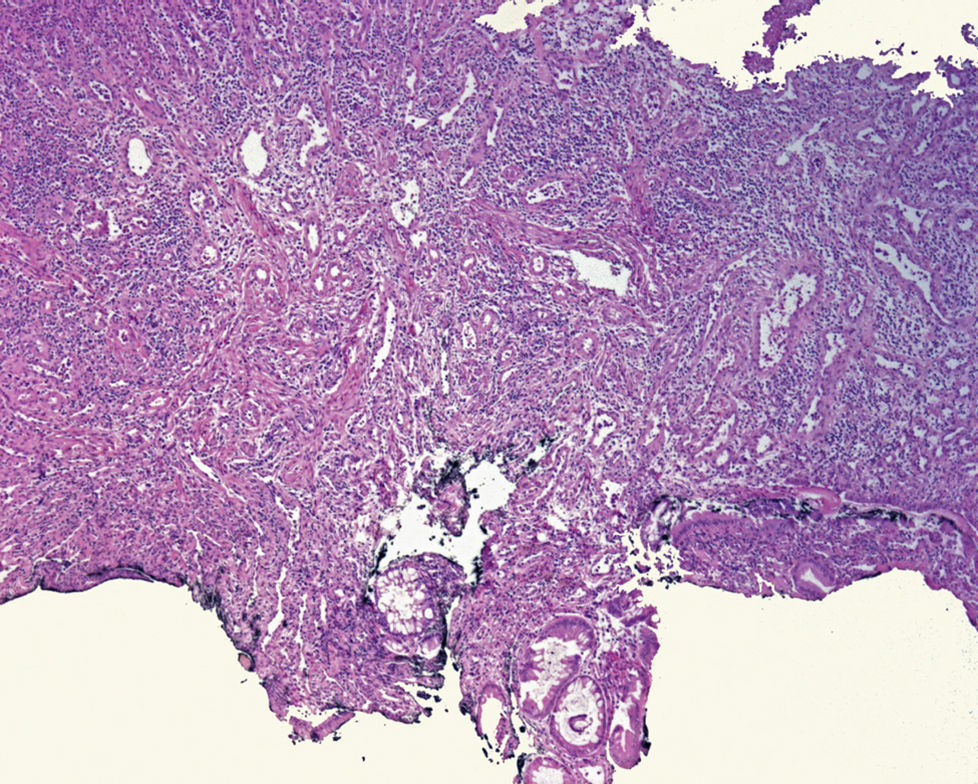
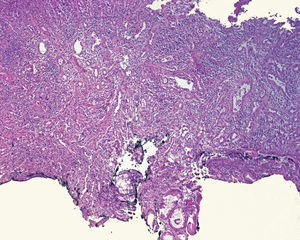
Definitive diagnosis is made through the histopathology study. IFPs are characterized by fusiform, mesenchymatous cells with concentric condensation (onion skin), no necrosis or significant mitosis, as well as by fibroblast and neovessel proliferation and an inflammatory infiltrate rich in eosinophils, lymphocytes, plasma cells, and mastocytes.11,12 Immunohistochemistry studies show important positivity for CD34 and negativity for CD117 (c-kit) in the fusiform cells. IFPs usually display positivity for fascine (a dendritic cell marker), D1 cyclin (a cell cycle regulation defect marker), calponin, and vimentin and variable reactivity for actin, CD68, desmin, and the S100 protein.13 The differential diagnosis must be made with gastrointestinal stroma tumor (GIST). Even though both are positive for CD34 and vimentin, GISTs are positive for CD117 (c-kit) and IFPs are not. IFPs should also be distinguished from schwannoma, fusiform cell leiomyoma, and inflammatory myofibroblastic tumor. Schwannomas are positive for S100 and negative for CD34. Fusiform cell leiomyoma is positive for desmin and actin and only 10 to 15% are positive for CD34. Inflammatory myofibroblastic tumor displays positivity for actin and CD34. Inflammatory fibrosarcoma and spindle-cell carcinoid tumor are other diagnoses that should be considered.3,4,12,13
Currently, the majority of cases can be treated with polypectomy and the others require surgery. Their long-term prognosis is excellent.13 Endoscopic polypectomy is adequate for treating small-diameter polyps. Larger polyps require surgical resection because they cause complications such as intussusception or obstruction that need emergency surgery.9 They do not recur after surgery.2 No recurrence has been reported in our patients.
There are two case reports on IFP in a Mexican population. In 2008, Aguilar-Davidov et al. reported on the case of a 9.1cm gastric polyp included in their case series.17 In 2011, Morales-Fuentes et al. described a 42-year-old man with abdominal pain with terminal ileum intussusception identified by abdominal computerized tomography scan. Laparoscopy was performed, finding a 3cm IF in the ileum 15cm from the ileocecal valve.18
IFPs are extremely rare in the Mexican population. They usually present with weight loss and iron deficiency anemia and are more frequently located in the stomach and small bowel. They require a multidisciplinary approach and their prognosis is excellent. The present case series on IFP is the largest to be reported in a Mexican population.
Ethical responsibilitiesProtection of persons and animalsThe authors declare that no experiments were performed on humans or animals for this study.
Data confidentialityThe authors declare that no patient data appear in this article.
Right to privacy and informed consentThe authors declare that no patient data appear in this article.
Financial disclosureNo financial support was received in relation to this study.
Conflict of interestThe authors declare that there is no conflict of interest.
The authors wish to thank Dr. Miguel Ángel Ramírez-Luna and Dr. Rubén Cortés-González for their participation in the esophageal IFP case.
Please cite this article as: Romano-Munive AF, Barreto-Zuñiga R, Rumoroso-García JA, Ramos-Martínez P. Pólipo fibroideo inflamatorio del tracto gastrointestinal: 10 años de experiencia del Instituto Nacional de Ciencias Médicas y Nutrición Salvador Zubirán. Revista de Gastroenterología de México. 2016;82:134–140.