Cardiovascular disease is a growing public health problem. Forty percent of the general population will suffer from the disease by 2030, consequently requiring antithrombotic therapy. Cardiogastroenterology is a new area of knowledge that evaluates the gastrointestinal effects and complications of antithrombotic therapy. Our aim was to evaluate, through a validated questionnaire, the knowledge held by a group of specialists and residents in the areas of gastroenterology and internal medicine, about pharmacology and drug prescription, as well as gastrointestinal risks and complications, in relation to antithrombotic therapy.
Patients and methodsA validated questionnaire composed of 30 items was applied to a group of specialists and residents in the areas of gastroenterology and internal medicine. The questions were on indications, pharmacology, evaluation of risks for gastrointestinal bleeding and thromboembolic events, and use of antithrombotic therapy during endoscopic procedures. Sufficient knowledge was defined as 18 or more (≥ 60%) correct answers.
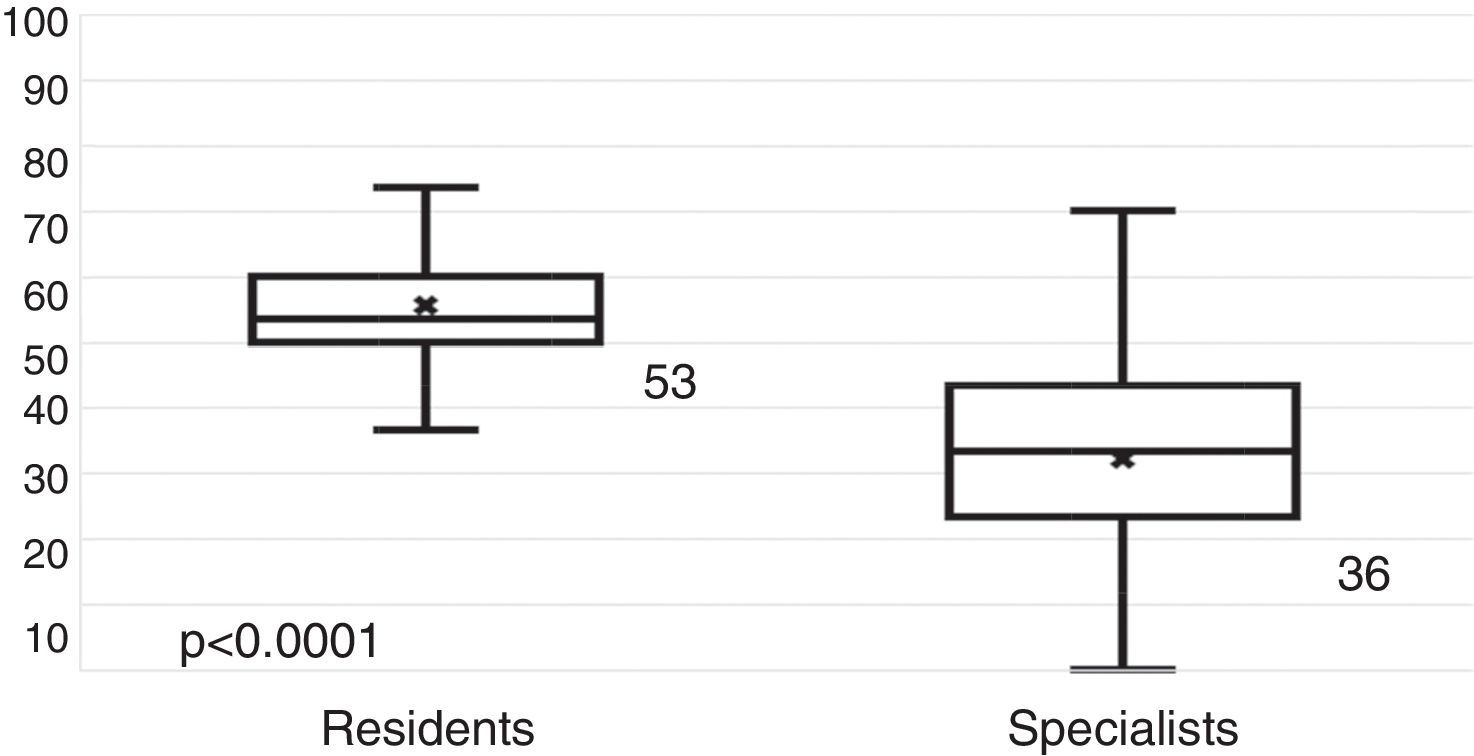
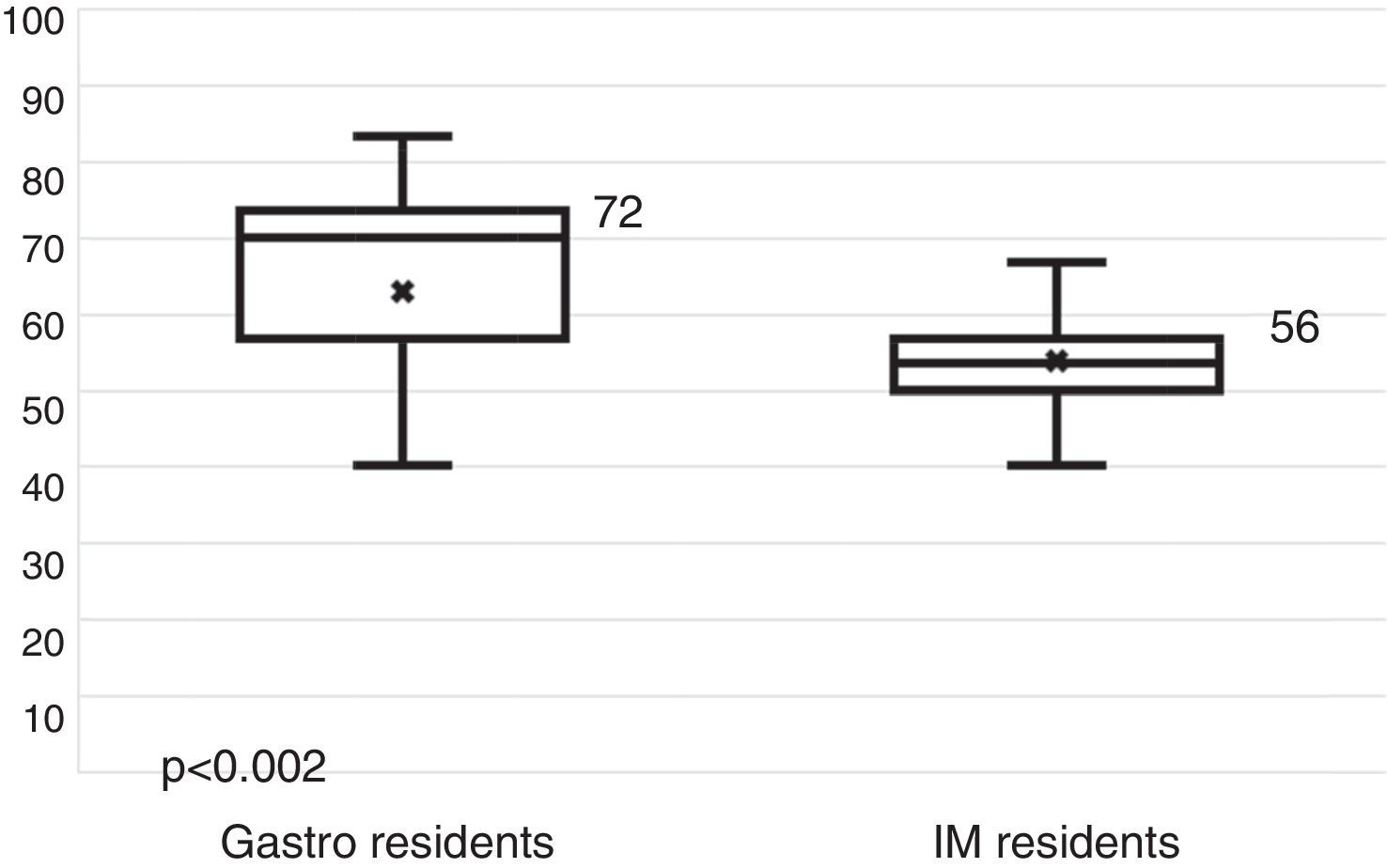
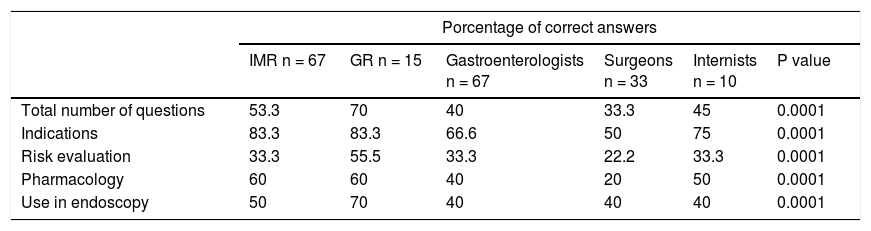
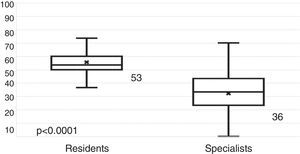
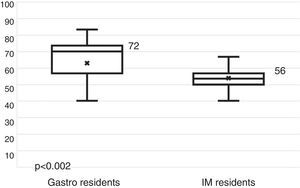
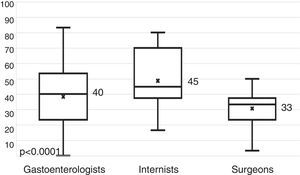
ResultsThe questionnaire was answered by 194 physicians: 82 (42%) internal medicine residents and gastroenterology residents and 112 (58%) specialists. Only 40 (20.6%) of the participants had sufficient knowledge of cardiogastroenterology. Residents had a higher number of correct answers than specialists (53 vs. 36%, P<.0001). The gastroenterology residents had more correct answers than the internal medicine residents, gastroenterologists, and internists (70 vs. 53, 40, and 46%, respectively, P<.001). Only residents had sufficient knowledge regarding pharmacology and the use of antithrombotic therapy in endoscopy (P<.0001). All groups had insufficient knowledge in evaluating the risk for gastrointestinal bleeding and thrombosis.
ConclusionsKnowledge of cardiogastroenterology was insufficient in the group of residents and specialists surveyed. There is a need for medical education programs on the appropriate use of antithrombotic therapy.
La enfermedad cardiovascular (ECV) es un problema creciente de salud pública. El 40% de la población general en 2030 presentará ECV y como consecuencia requerirá terapia antitrombótica (TAA). La cardiogastroenterología (CGE) es una nueva área de conocimiento que evalúa los efectos y complicaciones gastrointestinales de la TAA. Nuestro objetivo fue evaluar mediante una encuesta validada el conocimiento en prescripción, farmacología, riesgos y complicaciones gastrointestinales de la TAA en un grupo de especialistas y residentes de gastroenterología (RG) y medicina interna (RMI).
Pacientes y métodosSe aplicó una encuesta validada de 30 preguntas en un grupo de especialistas y RMI y RG. La encuesta incluyó preguntas de indicaciones, farmacología, evaluación de riesgo de hemorragia gastrointestinal, riesgo trombótico y el uso de TAA durante procedimientos endoscópicos. Se definió conocimiento suficiente como ≥ 18 (> 60%) aciertos.
ResultadosLa encuesta fue contestada por 194 médicos: 82 (42%) RMI y RG y 112 (58%) especialistas. Solo 40 (20.6%) tuvieron conocimiento suficiente en CGE. Los residentes tuvieron un mayor número de aciertos que los especialistas (53% vs. 36%, p < 0.0001). Los RG tuvieron más aciertos que los RMI, RG e internistas (70% vs. 53%, 40% y 46%, respectivamente, p < 0.001). Solo los residentes tuvieron conocimiento suficiente en farmacología y uso de la TAA en endoscopia (p < 0.0001). Todos los grupos tuvieron conocimiento insuficiente en evaluación de riesgo trombótico-hemorrágico.
ConclusionesExiste conocimiento insuficiente sobre CGE en este grupo de residentes y especialistas. Se requieren programas de educación médica acerca del uso apropiado de la TAA.
Cardiovascular disease is a growing public health problem. It is projected for the year 2030 that 40% of the Western population will present with some form of cardiovascular disease.1–3 And due to the increase in life expectancy, an increase in the incidence of age-associated comorbidities, which include cardiovascular disease, is also expected.3 Antithrombotic therapy (ATT) is the cornerstone of cardiovascular disease treatment. With the advent of new antithrombotic medications and the combination of antithrombotic drugs in complex regimens, the gastroenterologist is increasingly exposed to the interactions between ATT and the gastrointestinal tract.3,4 Antithrombotic therapy raises the risk for digestive tract bleeding and the combination of numerous antithrombotic drugs in a single patient results in more adverse events.5,6 In a study on 78,133 patients, Abraham et al. showed that the use of complex ATT brought about a higher number of hospitalizations and transfusions due to gastrointestinal tract bleeding.6 Likewise, there is greater risk for bleeding with the combination of antithrombotic drugs in complex regimens in patients undergoing endoscopic procedures.7 The gastroenterologist should have deep knowledge of pharmacology and the use of and indications for antithrombotic drugs. The therapeutic decisions made in patients on ATT must involve an analysis of the balance between the risk for digestive tract bleeding that is spontaneous or associated with endoscopic procedures, and the thromboembolic risk in those patients with cardiovascular disease that require modifications in the ATT for undergoing an endoscopic procedure or for presenting with acute gastrointestinal bleeding.4
Cardiogastroenterology (CGE) is a new area of knowledge that evaluates the gastrointestinal effects and complications of ATT.3,4 As a result, the American and European societies of gastrointestinal endoscopy (ASGE and ESGE) have published guidelines on the use of ATT during endoscopic procedures. The most recent versions were published in 2016.4
Evidence on the use of ATT in all the endoscopic clinical settings is heterogeneous, in addition to the fact that there is insufficient dissemination of the guidelines and physicians have suboptimum knowledge of ATT use in endoscopy. In Mexico, there is no information on the knowledge of and adherence to the guidelines on the part of physicians that manage patients requiring ATT and endoscopy.
The aim of the present study was to evaluate the knowledge about the use of ATT and its complications in a group of residents and specialists in the areas of Internal Medicine and Gastroenterology.
Materials and methodsA comparative cross-sectional study was conducted by applying a written, validated, 30-item questionnaire on the use of antiaggregants and anticoagulants to gastroenterologists, internists, and surgeons (see Appendix). Four areas of knowledge about the use of ATT were evaluated: indications, thromboembolic and bleeding risk assessment, pharmacokinetics, pharmacodynamics, and use in endoscopic procedures. The questionnaire was formulated using the information in the guidelines on the use of ATT in endoscopic procedures published by the ASGE and ESGE.4,8,9 Content validity of the questionnaire was determined through its application to 2 cardiologists and 2 gastroenterologists.
The questionnaire was applied at an international Latin American congress on gastroenterology and at a tertiary care hospital center in Mexico City.
The variables analyzed were age, sex, length of time of medical practice, specialty, and number and proportion of correctly answered items. Sufficient knowledge was considered at a value of ≥18 correct answers (60%). For the statistical analysis, the quantitative variables were compared using the Mann-Whitney U test and the qualitative variables were compared through the chi-square test, employing the IBM SPSS version 22 software.
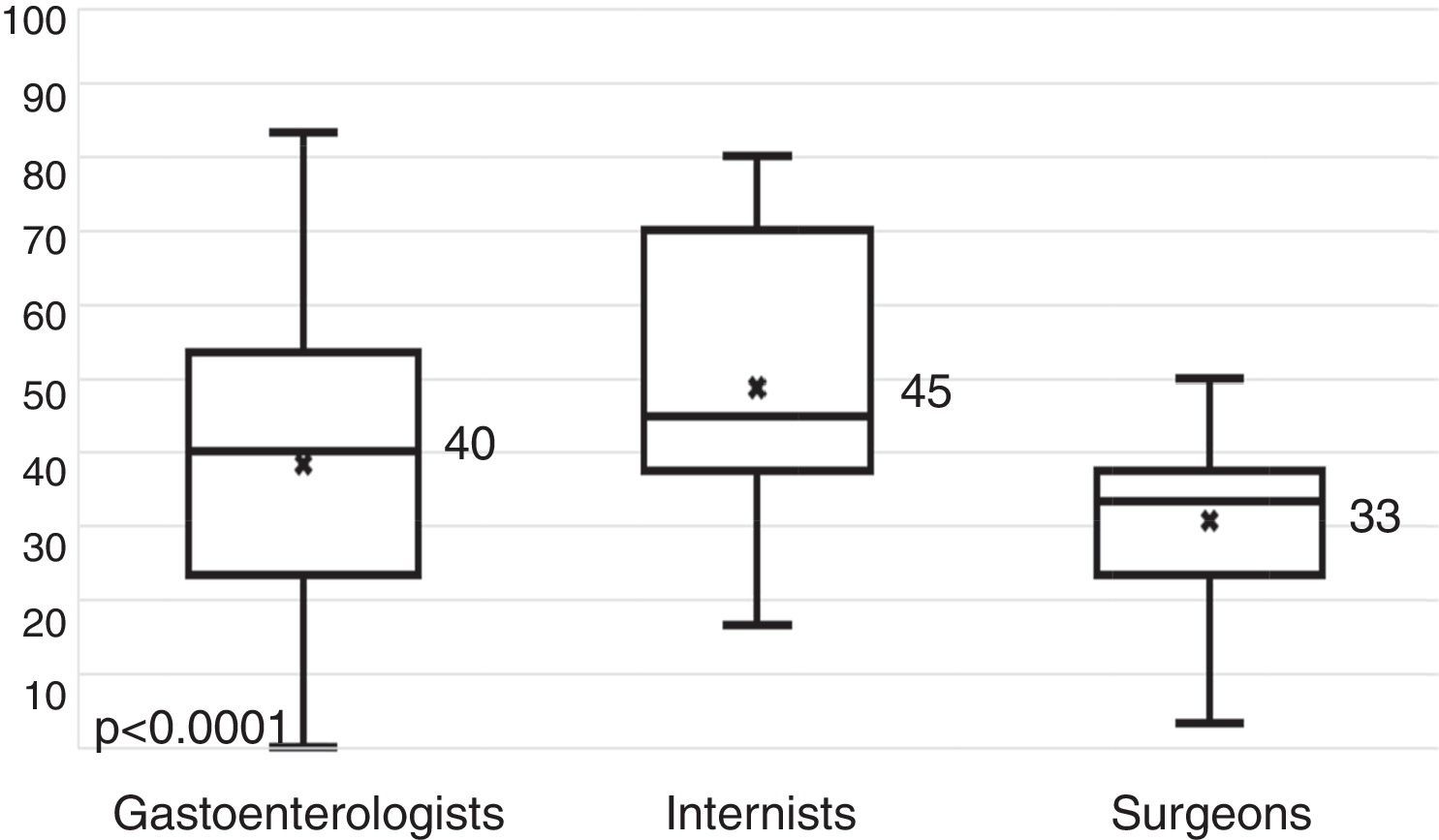
ResultsThe questionnaire (Appendix) was applied to 194 physicians, 67 (34.5%) of whom were internal medicine residents (IMRs), 15 (7.8%) were gastroenterology residents (GRs), and 112 (57.7%) were specialists. Of the specialists, 67 (34.5%) were gastroenterologists, 33 (17%) were surgeons, and 10 (5.1%) were internists. A total of 154 (79.6%) of the participants were men and 40 (20.4%) were women. Their median age was 36 years. The specialists had been practicing medicine for a median of 19 years and 21% had a sub-specialty. Prior to the survey, 32% of the participants were familiar with the term CGE, 72% of whom knew the correct definition. Only 20.6% of the physicians surveyed had sufficient knowledge about CGE (>60% of items answered correctly). Residents had a higher percentage of correct answers than specialists (53 vs. 36%; p < 0.0001) (fig. 1). The GRs had a higher percentage of correct answers, compared with the IMRs (70 vs. 53%; p < 0.002) (fig. 2), gastroenterologists (70 vs. 40%; p<0.0001), and the rest of the physicians surveyed (70 vs. 46%; p < 0.001). There were no differences between the IMRs and GRs in the number of correct answers per academic year. The surgery specialists had a median of fewer correct answers (33%) than the gastroenterologists (40%) and internists (45%) (fig. 3). Regarding the knowledge of ATT indications, only the surgeons had insufficient knowledge. In contrast, the GRs, IMRs, gastroenterologists, and internists had sufficient knowledge. The residents had sufficient knowledge of ATT pharmacology and only the GRs had sufficient knowledge of ATT use in endoscopy. Finally, none of the medical groups surveyed had sufficient knowledge in relation to the evaluation of thromboembolic and bleeding risks (Table 1).
Percentage of correct answers per evaluated area between specialists.
| Porcentage of correct answers | ||||||
|---|---|---|---|---|---|---|
| IMR n = 67 | GR n = 15 | Gastroenterologists n = 67 | Surgeons n = 33 | Internists n = 10 | P value | |
| Total number of questions | 53.3 | 70 | 40 | 33.3 | 45 | 0.0001 |
| Indications | 83.3 | 83.3 | 66.6 | 50 | 75 | 0.0001 |
| Risk evaluation | 33.3 | 55.5 | 33.3 | 22.2 | 33.3 | 0.0001 |
| Pharmacology | 60 | 60 | 40 | 20 | 50 | 0.0001 |
| Use in endoscopy | 50 | 70 | 40 | 40 | 40 | 0.0001 |
The international endoscopy societies have published numerous guidelines on the indications, pharmacology, and use of ATT during endoscopic procedures. Because of the emergence of new drugs, new evidence is produced rapidly. The most extensively disseminated and widely used guidelines are those of the ASGE and the ESGE, and their most recent versions are from 2016.4,9
Despite numerous efforts on the part of the medical societies involved, at times the guidelines are not completely practical or there is still not enough evidence to cover all the daily practice settings encountered by the endoscopist. In one study, a systematic search of ATT management guidelines during gastrointestinal tract bleeding was conducted.10 In spite of the great number of articles found in the initial search (81,320), almost none had useful recommendations in relation to strategies for the use of anticoagulants and antiplatelet agents in digestive tract bleeding. Of all the articles retrieved in the search, only 76 were eligible, and after their review, only 4 had useful information on the subject at hand.10
Likewise, and in accordance with our study results, knowledge of the physicians involved appears to be suboptimal. In a study published in 1996, a questionnaire containing 22 items was applied to 3,300 members of the ASGE and great heterogeneity in the management of aspirin, NSAIDs, and anticoagulants during the periendoscopic period was found.11 That study provided key evidence for the first published guidelines on ATT and endoscopy, but even so, in 2004 a German study revealed that despite the dissemination of guidelines, periendoscopic management of patients with ATT was heterogeneous.12 Finally, in 2014, a study was conducted that showed suboptimal adherence to the guidelines on ATT in endoscopy, especially in patients under treatment with warfarin.13 Those results, together with ours, reveal the necessity of developing a strategy to strengthen the knowledge about CGE. Conferences, courses, and workshops on the evaluation of gastrointestinal and cardiovascular risks, as well as on the pharmacology and clinical use of ATT are essential in the education of today's specialist.
Among the limitations of the present study are: 1) The questionnaire was applied to residents and specialists at a tertiary care hospital center and to physicians attending an international gastroenterology congress, and so the results cannot be extrapolated to other populations of specialists that work at other levels of medical care and 2) Cardiology and Neurology specialists were not surveyed, and they are physicians that commonly utilize ATT and anticoagulants. A future study evaluating the degree of knowledge of CGE in physicians with those specialties is required.
With the results of the present study, we conclude that there is insufficient knowledge about CGE on the part of the specialist and there should be greater guideline dissemination. There should also be more continuing medical education courses, as well as studies that analyze that area of weakness in Mexican physicians, so that the necessary strategies to improve the management of patients with ATT that require endoscopy can be developed.
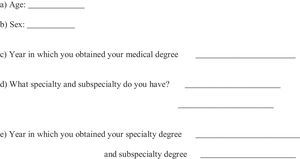
The following is an anonymous questionnaire to evaluate participant knowledge about cardiovascular risk, gastrointestinal risk, and use of antiaggregants and anticoagulants. Part One examines the demographic data and professional activity of the participant. Part Two is a knowledge-examining questionnaire.
Part One
f) What type of professional activity do you perform?
- a)
Private practice
- b)
Institutional
- c)
Both
g) Do you perform academic (teaching) professional activities?
- a)
Pregraduate professor
- b)
Postgraduate professor
- c)
None
h) What type of patient care activities do you provide?
- a)
Outpatient care
- b)
Hospitalized patient care
- c)
Both
i) How many patients do see per month that are under antiplatelet treatment?
- a)
None
- b)
1 to 10 patients
- c)
11 to 20 patients
- d)
21 to 30 patients
- e)
More than 30 patients
j) How many patients to you see per month that are under oral anticoagulant treatment?
- a)
None
- b)
1 to 10 patients
- c)
11 to 20 patients
- d)
21 to 30 patients
- e)
More than 30 patients
k) Are you familiar with the term cardiogastroenterology?
- a)
Yes
- b)
No
l) What is cardiogastroenterology?
- a)
A gastroenterologist with a subspecialty in cardiology
- b)
A gastroenterologist with an advanced specialty in cardiology
- c)
An area of gastroenterology that studies the effects of antiaggregant and anti-coagulant drugs used in cardiologic disorders on the gastrointestinal tract
- d)
An area of cardiology that studies the effects that gastrointestinal diseases have on the cardiovascular apparatus
- e)
It does not exist
Mark the letter of the correct answer with an “x”. Answer all questions.
Part Two
1. What percentage of the adult population over 50 years of age presents with cardiovascular disease?
- a)
10%
- b)
20%
- c)
40%
- d)
60%
2. Which one of the following sentences defines the term primary prophylaxis in cardiovascular disease?
- a)
Anticoagulant use in a patient with a history of a cerebrovascular event (CVE)
- b)
Double antiaggregant use in a patient with a history of acute myocardial infarct (AMI)
- c)
Anticoagulant use in a patient with no history of cardiovascular events
- d)
Antiaggregant use in a patient with no personal history of cardiovascular events at risk for a cardiovascular event
3. In which one of the following endoscopic procedures should aspirin be suspended in patients at risk for a cardiovascular event?
- a)
Endoscopic sphincterotomy
- b)
Endoscopic polypectomy
- c)
Endoscopic gastrostomy
- d)
None of the above
4. Which is the most widely used primary prophylaxis medication?
- a)
Acetylsalicylic acid
- b)
Clopidogrel
- c)
Ticagrelor
- d)
Rivaroxavan
5. Which one of the following endoscopic procedures has a greater risk for bleeding?
- a)
Colonoscopy with biopsies
- b)
Polypectomy of a colonic polyp < 1cm in diameter
- c)
Peptic esophageal stricture dilation
- d)
Biliary stent placement without sphincterotomy
6. The taking of biopsies during endoscopy increases the risk for bleeding in patients using ATT (monotherapy or combination therapy).
- a)
True
- b)
False
7. What is the definition of an endoscopic procedure with a high risk for bleeding?
- a)
>10% of bleeding associated with the procedure
- b)
>1% of bleeding associated with the procedure
- c)
>5% of bleeding associated with the procedure
- d)
>20% of bleeding associated with the procedure
8. Of the following settings, which one has the greater risk for thrombosis upon anticoagulation suspension?
- a)
History of deep vein thrombosis 6 months prior
- b)
Mechanical aortic stent
- c)
Mechanical mitral stent
- d)
Isolated atrial fibrillation
9. In over-anticoagulated patients (INR >4) with gastrointestinal bleeding, what is the probability in an endoscopic study of finding a lesion that explains the cause of the bleeding?
- a)
50%
- b)
80%
- c)
60%
- d)
30%
10. In a stable patient anticoagulated with warfarin or acenocoumarol for a nonvalvular indication that requires urgent endoscopic therapy, the ideal INR should be:
- a)
normal INR
- b)
INR <2.5
- c)
INR <1.5
- d)
The procedure can be performed without considering the INR, given that it is an urgent intervention
11. Which one of the following drugs does not have an appropriate antidote for reversing the anticoagulant effect?
- a)
Warfarin
- b)
Acenocoumarol
- c)
Rivaroxaban
- d)
Non-fractioned heparin (conventional heparin)
12. What is the recommended treatment duration of dual antiplatelet therapy in patients with a drug-eluting stent in the coronary arteries?
- a)
6-8 months
- b)
4 weeks
- c)
12 months
- d)
For life
13. How long before an endoscopic procedure with high risk for bleeding should warfarin be suspended in a patient with a low thromboembolic risk?
- a)
1- 2 days
- b)
0 - 8 days
- c)
3 - 5 days
- d)
It does not need to be suspended
14. Which one of the following statements is true in relation to the new oral anticoagulants (dabigatran, rivaroxaban)?
- a)
They have a shorter half-life than warfarin
- b)
It is easy to reverse their effect in case of bleeding
- c)
They have multiple pharmacologic interactions
- d)
Their main elimination site is the liver
15. What is the appropriate action to take in a patient with a history of AMI 3 years prior, who takes aspirin and will undergo polypectomy for a 2.5cm sessile polyp in the transverse colon?
- a)
Suspension of aspirin 5 days before the procedure
- b)
Aspirin should not be suspended
- c)
Continue aspirin and transfuse platelets during the procedure
- d)
Suspend aspirin 10 days before the procedure
16. Which one of the following statements corresponds to secondary prophylaxis in cardiovascular disease?
- a)
Treatment with platelet anti-aggregant in patients with a history of deep vein thrombosis
- b)
Treatment with platelet anti-aggregant in patients with prior AMI or CVE
- c)
Treatment with anticoagulant in patients with no personal history of cardiovascular disease at high risk for presenting with cardiovascular disease
- d)
Treatment with platelet anti-aggregant in patients with no prior AMI or CVE
17. In a patient with acute coronary syndrome and upper gastrointestinal bleeding causing hemodynamic instability, what is the most appropriate action to take based on the mortality risk in acute coronary syndrome?
- a)
Stabilize the patient and perform endoscopy after 72h
- b)
Stabilize the patient and perform endoscopy within the first 48 to 72h
- c)
Stabilize the patient and do not perform endoscopy due to unacceptable mortality risk
- d)
Immediate endoscopy for endoscopic treatment of the bleeding
18. Of the thienopyridines (P2Y12 antagonists), which one reversibly inhibits the P2Y12 receptor?
- a)
Clopidogrel
- b)
Prasugrel
- c)
Ticagrelor
- d)
All of the above
19.- Of the thienopyridines (P2Y12 antagonists), which one has the longest half-life?
- a)
Clopidogrel
- b)
Prasugrel
- c)
Ticagrelor
- d)
Ticlopidine
20. What is the critical post-myocardial infarct time without intervention (no angioplasty or stent) with the greatest possibility for a new acute coronary syndrome (ACS) if clopidogrel is suspended?
- a)
The first 6 months
- b)
The first month
- c)
The first 3 months
- d)
The first 12 months
21. In acute bleeding from peptic ulcer treated endoscopically in a patient with a history of AMI, when should aspirin use be reinitiated?
- a)
Never. It is contraindicated.
- b)
Reinitiate aspirin when the bleeding is under control
- c)
Never. It should be changed to clopidogrel
- d)
After 30 days
22. In patients that require dual antiplatelet therapy through a drug-eluting stent, that have a colonic polyp, which one of the following courses of action is the most appropriate?
- a)
Defer polypectomy until one year after coronary stent placement
- b)
Defer polypectomy up to 3 months after coronary stent placement
- c)
If the patient accepts the risk for late hemorrhage, perform polypectomy and place a hemostatic clip
- d)
Suspend the 2 antiaggregants and bridge with Fraxiparine to perform the polypectomy
- e)
a and c are correct
23. Which one of the following outcomes is more common with the use of combination antithrombotic therapy?
- a)
Upper gastrointestinal bleeding
- b)
Lower gastrointestinal bleeding
- c)
Bleeding with transfusion requirement
- d)
Bleeding with hospitalization requirement
24. How long after an acute gastrointestinal bleed is it recommended to reinitiate warfarin?
- a)
1-3 days
- b)
15-30 days
- c)
10-14 days
- d)
4-7 days
25. In a patient with normal kidney function, how long should the new anticoagulants (dabigatran, rivaroxaban) be suspended before performing an endoscopic procedure with a high risk for bleeding?
- a)
3-5 days
- b)
5-7 days
- c)
10 days
- d)
1-2 days
26. With respect to proton pump inhibitor and clopidogrel interaction, which one of the following statements is correct?
- a)
The interaction is explained by a common metabolism in the CYP2C19 cytochrome
- b)
The two drugs do not interact
- c)
It has been demonstrated in randomized clinical trials that the combination of clopidogrel and omeprazole increases the risk for myocardial infarction
- d)
Interaction with clopidogrel is the same for all proton pump inhibitors
27. In a patient with indication for receiving undefined antiplatelet therapy, which maneuver reduces the risk for gastrointestinal bleeding?
- a)
Adding misoprostol to the treatment
- b)
Utilizing clopidogrel instead of aspirin
- c)
Eradicating Helicobacter pylori (H. pylori) in all positive patients
- d)
Eradicating H. pylori only if there is a history of gastric or duodenal ulcer
28. A 50-year-old patient taking warfarin because he has a mechanical aortic stent arrives at the emergency room with hematemesis. His BP is 100/60 and the INR is 2.3. In addition to resuscitation, what is the best course of action?
- a)
To perform endoscopy, anticoagulation must be reversed to an INR of 1.5
- b)
Endoscopy can be performed without reversing the anticoagulation
- c)
Endoscopy should be postponed until the INR is normal
- d)
Vitamin K should be administered immediately
29. What does bridging anticoagulation before an invasive procedure mean to you?
- a)
Warfarin suspension before the procedure.
- b)
Warfarin suspension and temporary use of heparin up to one day before the procedure
- c)
Warfarin suspension and temporary use of aspirin/clopidogrel up to one day before the procedure
- d)
Continue warfarin and reverse the effect of vitamin K the day of the procedure
30. In a patient under anticoagulant therapy, which one of the following factors should be considered before performing an endoscopic procedure and modifying the anticoagulation regimen?
- a)
Anesthetic risk and cardiovascular risk
- b)
Hemorrhagic risk and anesthetic risk
- c)
Thromboembolic risk and hemorrhagic risk
- d)
Anesthetic risk and thromboembolic risk
The authors declare that no experiments were performed on humans or animals for this study.
The authors declare that no patient data appear in this article.
The authors declare that no patient data appear in this article.
No financial support was received in relation to this study/article.
The authors declare that there is no conflict of interest.
Please cite this article as: Aguilar-Nájera O, Valdovinos-García LR, Tepox-Padrón A, et al. ¿Cuánto sabe el especialista sobre cardiogastroenterología? Revista de Gastroenterología de México. 2018;83:98–105.