Sixty percent of the patients with gastric carcinomas are candidates for surgical resection through total gastrectomy and esophagojejunostomy, the latter of which is associated with leaks in up to 12.3% of cases. There is no standardized procedure for diagnosing anastomotic leaks. The aim of the present study was to establish the diagnostic sensitivity of the contrast-enhanced swallow study for detecting esophagojejunostomy leakage after total gastrectomy.
Materials and methodsA retrospective analysis was conducted on patients that underwent total gastrectomy due to gastric adenocarcinoma, within the time frame of 2002 and 2017. Demographic, clinical, and laboratory factors were identified, emphasizing the clinical and radiologic detection of anastomotic leaks. Descriptive statistics were carried out and the sensitivity of the contrast-enhanced swallow study for diagnosing leakage was calculated.
ResultsFifty-eight patients were included in the study. Their mean age was 61.5 years. A total of 55.2% of the patients were men and 44.8% were women. Gastric adenocarcinoma was the indication for gastrectomy in 100% of the cases. Anastomotic leak presented in 31.01% of the patients. Diagnostic sensitivity of the contrast-enhanced swallow study for detecting leaks was 66%.
ConclusionsAccording to our analysis, the contrast-enhanced swallow study had limited diagnostic efficiency for detecting anastomotic leaks, with a sensitivity of 66%. We suggest maintaining high diagnostic suspicion in patients with studies that are initially negative and basing decisions on a more extensive approach.
60% de los pacientes con carcinomas gástricos son candidatos a resección quirúrgica mediante gastrectomía total y esofagoyeyuno anastomosis. Esta se asocia con fugas hasta en 12.3% de los casos. No existe un procedimiento estandarizado para el diagnóstico de fugas en anastomosis. El objetivo de este trabajo es establecer la sensibilidad diagnóstica del estudio contrastado para la detección de fugas en esofagoyeyuno anastomosis post gastrectomía total.
Materiales y MétodosAnálisis retrospectivo de pacientes sometidos a gastrectomía total por adenocarcinoma gástrico entre los años 2002 y 2017. Se identificaron factores demográficos, clínicos y de laboratorio, con énfasis en la detección de fugas de anastomosis por clínica y radiología. Se realizó estadística descriptiva y se calculó la sensibilidad del estudio contrastado para el diagnóstico de fuga.
ResultadosSe incluyeron 58 pacientes. La edad promedio fue de 61.5 años; 55.2% de los pacientes eran hombres y 44.8% eran mujeres. La indicación de la gastrectomía fue adenocarcinoma gástrico en el 100% de los casos. La fuga de anastomosis se presentó en 31.01% de los pacientes. La sensibilidad del estudio contrastado para la detección de fugas fue del 66%.
ConclusionesDe acuerdo a nuestro análisis, la eficiencia diagnóstica del estudio contrastado para detección de fugas anastomóticas es limitada, con una sensibilidad del 66%. Sugerimos mantener una alta sospecha clínica en pacientes con estudios iniciales negativos, y basar la toma de decisiones en un abordaje más extenso.
Twenty-eight thousand new cases of gastric cancer are diagnosed in the United States annually, with 10,960 gastric cancer-related deaths.1 That disease is the third cause of cancer deaths worldwide.2 The World Health Organization estimated that in 2012, 6.8% of malignant tumors (around one million cases) were related to gastric cancer, globally considered the fifth most frequent cancer, after cancers of the lung, breast, colorectum, and prostate.3
Surgery has been positioned as the best option for offering patients adequate local disease control, combined in the majority of cases with adjuvant or perioperative chemotherapy and radiotherapy.4,5 The surgical treatment for tumors located in the gastroesophageal junction is total gastrectomy, which is reconstructed with a Roux-en-Y esophagojejunal anastomosis. There are numerous complications with that procedure, the most dreaded of which is esophagojejunal anastomotic leakage (EJAL). EJAL is associated with high morbidity and mortality and its incidence has been reported in up to 12.3% of cases.6
The definition of EJAL is heterogeneous in the literature. It is generally accepted that EJAL is any clinical presentation or radiologic imaging study consistent with dehiscence of the anastomosis. However, some authors utilize more specific criteria, such as discharge of intestinal content through the surgical drains associated with signs of inflammatory response, ileus, or peritonitis, whereas others utilize radiologic parameters, such as the presence of perianastomotic collections or extravasation of contrast medium.7 The heterogeneity in the definition makes standardizing the diagnostic/therapeutic approach more difficult in those patients.
The performance of a routine study with contrast medium (water-soluble contrast swallow study) after the surgical procedure to evaluate the integrity of the esophagojejunal anastomosis is common practice at different hospital centers. The diagnostic efficiency of the contrast swallow for the diagnosis of leakage has been evaluated in several studies.
The aim of the present study was to determine the diagnostic efficiency of the routine water-soluble contrast swallow study in the first postoperative days for the detection of EJAL in patients that underwent total gastrectomy at a tertiary care hospital center in Mexico City.
Materials and methodsThe medical records of all the patients that underwent total gastrectomy due to gastric cancer, within the time frame of 2002–2017, were retrospectively reviewed. The definitive analysis included all the patients with complete medical record data that underwent a water-soluble contrast swallow study in the first 5–7 postoperative days. Anastomosis leak was considered when there was evidence of leakage in a radiologic study, discharge of intestinal content through the drains, or the presence of a perianastomotic collection in a computed axial tomography scan.
The statistical analysis was carried out using the IBM SPSS version 20.0. program. The quantitative variables were analyzed utilizing the ANOVA test and the chi-square test was employed for the qualitative variable analysis.
The present study was conducted in accordance with the principles established in the Declaration of Helsinki, and due to its retrospective design, was exempt from review by an ethics committee. The authors declare that they have treated all patient data with confidentiality and anonymity, following the protocols of their work center.
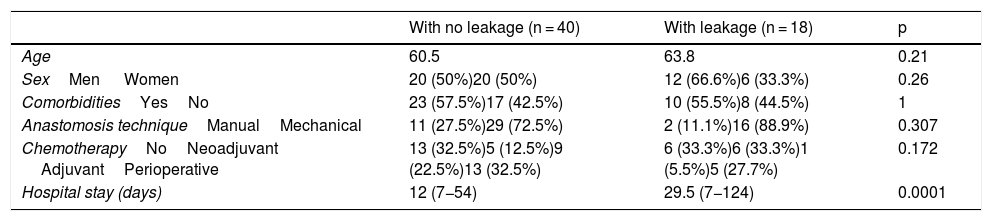
ResultsFifty-eight total gastrectomies were performed during the study period on patients diagnosed with gastric cancer. The cohort was divided into patients with no anastomotic leakage (n = 40) (68.9%) and patients with anastomotic leakage (n = 18) (31.01%). The general characteristics of the study patients are shown in Table 1. Mean age of the patients was 61.5 years (range: 29–89 years) (p = 0.21). Twenty-six of the patients were women (44.8%) and 32 were men (55.2%) (p = 0.26). A total of 43.1% of the patients did not present with any other comorbidities. The following comorbidities were found in the remaining 56.9%: systemic hypertension in 32.7%, type 2 diabetes mellitus in 27.5%, obesity in 3.5%, hypothyroidism in 3.5%, chronic obstructive pulmonary disease in 1.7%, dyslipidemia in 8.6%, and human immunodeficiency virus infection in 1.7% of the patients (p = 1).
Characteristics of the patients with esophagojejunal anastomosis.
| With no leakage (n = 40) | With leakage (n = 18) | p | |
|---|---|---|---|
| Age | 60.5 | 63.8 | 0.21 |
| SexMen Women | 20 (50%)20 (50%) | 12 (66.6%)6 (33.3%) | 0.26 |
| ComorbiditiesYesNo | 23 (57.5%)17 (42.5%) | 10 (55.5%)8 (44.5%) | 1 |
| Anastomosis techniqueManualMechanical | 11 (27.5%)29 (72.5%) | 2 (11.1%)16 (88.9%) | 0.307 |
| ChemotherapyNoNeoadjuvant AdjuvantPerioperative | 13 (32.5%)5 (12.5%)9 (22.5%)13 (32.5%) | 6 (33.3%)6 (33.3%)1 (5.5%)5 (27.7%) | 0.172 |
| Hospital stay (days) | 12 (7−54) | 29.5 (7−124) | 0.0001 |
All the study patients were diagnosed with gastric adenocarcinoma and their surgeries were performed with curative intent. The technique for the creation of the esophagojejunal anastomosis was manual in 22.5% of the cases and mechanical (with a circular stapler) in 77.5% of the cases (p = 0.307).
Regarding systemic treatment, 32.7% of the patients did not receive chemotherapy at any stage of their treatment, 18.9% received neoadjuvant treatment, 17.2% received adjuvant treatment, and 31% received perioperative chemotherapy (p = 0.172). Days of hospital stay was the only characteristic with a statistically significant difference, with 12 (7−54) days in the group with no leaks and 29.5 (7−124) days in the group with leaks (p = 0.0001).
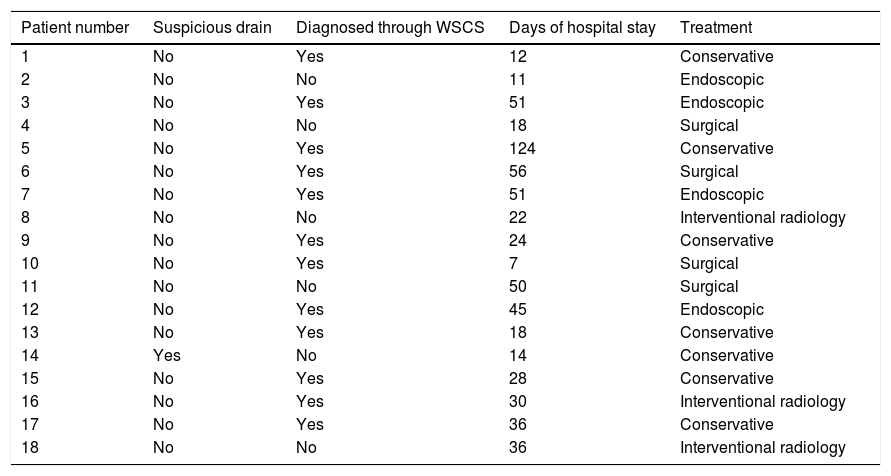
Eighteen patients were diagnosed with EJAL. Of those patients, 12 (66.6%) were diagnosed through a water-soluble contrast swallow study, the diagnosis of one patient was suspected due to drain characteristics, and the rest of the patients (n = 5) (27.7%) were diagnosed through computed axial tomography with oral and intravenous contrast medium. The diagnostic efficiency analysis of the contrast swallow study produced a sensitivity of 66%, specificity of 100%, positive predictive value of 100%, and negative predictive value of 86% at our hospital center. The treatment strategies utilized in the patients with EJAL are summarized in Table 2.
Treatment strategies in the patients with EJAL.
| Patient number | Suspicious drain | Diagnosed through WSCS | Days of hospital stay | Treatment |
|---|---|---|---|---|
| 1 | No | Yes | 12 | Conservative |
| 2 | No | No | 11 | Endoscopic |
| 3 | No | Yes | 51 | Endoscopic |
| 4 | No | No | 18 | Surgical |
| 5 | No | Yes | 124 | Conservative |
| 6 | No | Yes | 56 | Surgical |
| 7 | No | Yes | 51 | Endoscopic |
| 8 | No | No | 22 | Interventional radiology |
| 9 | No | Yes | 24 | Conservative |
| 10 | No | Yes | 7 | Surgical |
| 11 | No | No | 50 | Surgical |
| 12 | No | Yes | 45 | Endoscopic |
| 13 | No | Yes | 18 | Conservative |
| 14 | Yes | No | 14 | Conservative |
| 15 | No | Yes | 28 | Conservative |
| 16 | No | Yes | 30 | Interventional radiology |
| 17 | No | Yes | 36 | Conservative |
| 18 | No | No | 36 | Interventional radiology |
WSCS: Water-soluble contrast swallow.
The water-soluble contrast swallow study is routinely carried out after total gastrectomy at many hospital centers worldwide and is done so to evaluate the integrity of the esophagojejunal anastomosis before resuming oral diet.
Its use has historically been described as low-cost and noninvasive for patients. However, there are specific settings in which it is not a feasible study, such as in patients that have been in the intensive care unit for a long period of time. In addition, the risk for bronchoaspiration of the contrast material when performing the study is a factor that should be taken into consideration.8,9
We found a higher rate of leaks in our case series than that reported in the literature (31 vs. 12.3%) but we believe that difference is related to the heterogeneity in the definition of anastomotic leakage, given that ours was considerably inclusive.
The evidence of leakage in a water-soluble contrast swallow study or the observation of intestinal content discharge from a surgical drain is irrefutable. However, some authors of studies do not regard perianastomotic collections in asymptomatic patients as leaks, whereas we did in our study.
On the other hand, it should be pointed out that the rate of patients that required invasive management strategies in our study was similar to that reported in the international literature.
It is striking that in the present study there was a higher incidence of leakage in the patients that underwent reconstruction with mechanical staplers. Nevertheless, the comparative analysis between the 2 groups was not statistically significant (p = 0.307), which we believe could be due to the simple fact that the majority of cases had reconstruction with mechanical staplers.
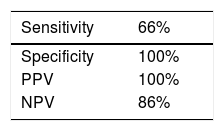
Upon examining the diagnostic yield of the water-soluble contrast swallow study for the detection of EJAL, sensitivity was 66%, specificity was 100%, positive predictive value was 100%, and negative predictive value was 86% (Table 3).
Specificity, sensitivity, positive predictive value, and negative predictive value of the water-soluble contrast swallow study for the detection of EJAL.
| Sensitivity | 66% |
|---|---|
| Specificity | 100% |
| PPV | 100% |
| NPV | 86% |
EJAL: esophagojejunal anastomotic leakage; NPV: negative predictive value; PPV: positive predictive value.
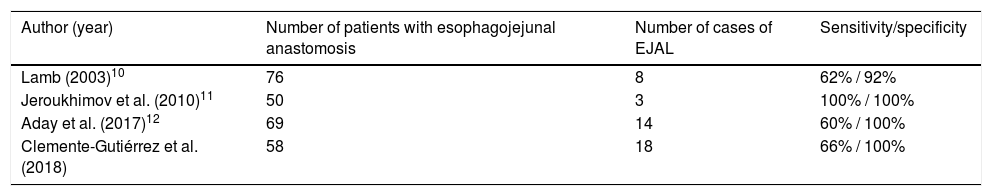
Those values are similar to the results reported in studies evaluating the same parameters, thus reaffirming the low diagnostic yield of the contrast swallow study for detecting EJAL in the Mexican population (Table 4).
Studies that analyzed the sensitivity of the water-soluble contrast swallow study for the detection of EJAL.
| Author (year) | Number of patients with esophagojejunal anastomosis | Number of cases of EJAL | Sensitivity/specificity |
|---|---|---|---|
| Lamb (2003)10 | 76 | 8 | 62% / 92% |
| Jeroukhimov et al. (2010)11 | 50 | 3 | 100% / 100% |
| Aday et al. (2017)12 | 69 | 14 | 60% / 100% |
| Clemente-Gutiérrez et al. (2018) | 58 | 18 | 66% / 100% |
EJAL: esophagojejunal anastomotic leakage.
In conclusion, the diagnostic efficiency of the contrast swallow study for the detection of EJAL is limited. With that in mind, high diagnostic suspicion should be maintained, and a more extensive approach carried out when merited, considering the consequences that most dreaded complication can have in the outcome of our patients.
Computed axial tomography with oral contrast medium is a tool that can aid in diagnosing esophagojejunal anastomotic leaks that are undetected in the water-soluble contrast swallow study.
Financial disclosureNo financial support of any kind was received in relation to this article.
Conflict of interestThe authors declare that there is no conflict of interest.
Contribution of the authorsAll the authors contributed equally to the present study, including drafting the manuscript, editing the images, discussing the cases, and commenting on the manuscript at all stages of its development.
Please cite this article as: Clemente-Gutiérrez U, Rodríguez-Chong JG, Morales-Maza J., Rodríguez-Quintero H., Sánchez-Morales G., Álvarez-Bautista FE., et al. Sensibilidad del trago de contraste hidrosoluble para la detección de fugas de anastomosis esofagoyeyunal. Revista de Gastroenterología de México. 2020;85:118–122.