Prehepatic portal hypertension in children can be asymptomatic for many years. Once diagnosed, the therapeutic measures (pharmacologic, endoscopic, and surgical) are conditioned by the specific characteristics of each patient. In Mexico, there are no recorded data on the incidence of the disease and patient characteristics.
AimsTo determine the main clinical, radiologic, and endoscopic characteristics upon diagnosis of these patients at the Instituto Nacional de Pediatría within the time frame of January 2001 and December 2011.
MethodsA cross-sectional, retrolective, descriptive, and observational study was conducted in which all the medical records of the patients with portal hypertension diagnosis were reviewed.
ResultsThere was a greater prevalence of prehepatic etiology (32/52) (61.5%) in the portal hypertension cases reviewed. Males (62.5%) predominated and 11 of the 32 patients were under 4years of age. The primary reason for medical consultation was upper digestive tract bleeding with anemia (71.9%) and the main pathology was cavernomatous degeneration of the portal vein (65.6%). Splenoportography was carried out on 17 of the 32 patients. A total of 65.5% of the patients received the combination therapy of propranolol and a proton pump inhibitor. Initial endoscopy revealed esophageal varices in 96.9% of the patients, 12 of whom presented with gastroesophageal varices. Congestive gastropathy was found in 75% of the patients. The varices were ligated in 8 cases, sclerotherapy for esophageal varices was carried out in 5 cases (15.6%), and sclerotherapy for gastric varices was performed in 2 patients. Seventeen patients (53.1%) underwent portosystemic diversion: 10 of the procedures employed a mesocaval shunt and 7 a splenorenal shunt. Nine patients (28.1%) underwent total splenectomy.
ConclusionsThe primary cause of the disease was cavernomatous degeneration of the portal vein; it was predominant in males and the first symptom was variceal bleeding.
La hipertensión portal prehepática puede cursar por muchos años asintomática en niños. Las medidas terapéuticas (farmacológicas, endoscópicas y quirúrgicas) luego del diagnóstico están condicionadas por las características específicas de cada paciente. En México no existe un registro que documente la incidencia y la caracterización de estos pacientes.
ObjetivoDeterminar las principales características clínicas, radiológicas y endoscópicas al diagnóstico de estos pacientes en el Instituto Nacional de Pediatría de enero de 2001 a diciembre de 2011.
MétodoEstudio observacional, descriptivo, retrolectivo y transversal, en el que fueron revisados todos los expedientes de pacientes con este diagnóstico.
ResultadosMayor prevalencia de etiología prehepática 32/52 (61.5%) de los casos revisados con diagnóstico de hipertensión portal. Predominio de género masculino (62.5%) y con 11/32 pacientes menores de 4años. Principal motivo de consulta: sangrado de tubo digestivo alto anemizante (71.9%); principal patología: degeneración cavernomatosa de la vena porta (65.6%). La esplenoportografía se describió en 17/32 pacientes. Un 65.5% de los pacientes recibió la combinación terapéutica con propranolol e inhibidor de la bomba de protones. Endoscopia inicial: várices esofágicas en el 96.9%. De estos, 12 casos con várices gastroesofágicas. Gastropatía congestiva: 75%. Se realizó ligadura de várices en 8 casos (25%), escleroterapia de várices esofágicas en 5 casos (15.6%), y escleroterapia en várices gástricas en 2 pacientes. En 17 pacientes (53.1%) fue realizada una derivación portosistémica: en 10 ileomesocava y en 7 esplenorrenal. Un 28.1% (9 pacientes) fueron sometidos a esplenectomía total.
ConclusionesLa principal causa fue la degeneración cavernomatosa de la porta, con una predominancia en varones. El primer síntoma fue el sangrado variceal.
The portal vein is responsible for close to two thirds of the hepatic blood flow. It supplies blood rich in oxygen, nutrients, growth factors, and hormones, among other elements. The portal vein only resists low pressures and portal hypertension is defined when portal pressure exceeds 5mmHg. A continuous flow with a normal range between 15-30cm/s can be observed through Doppler ultrasound.1,2
The etiology of portal hypertension syndrome is varied. Based on its anatomic classification, it can be categorized into prehepatic, intrahepatic (presinusoidal, sinusoidal, and postsinusoidal), and posthepatic. The reported prevalence of each etiology is varied. In their studies, Poddar et al.3 and Donatone4 reported a predominance in frequency of prehepatic portal hypertension over hepatic portal hypertension: 68% versus 32% and 54% versus 46%, respectively. Disease manifestations of prehepatic portal hypertension have been described to present at an initial age of 4.6 years and those of hepatic portal hypertension at 6.9 years.
The main causes of prehepatic portal hypertension are: portal vein thrombosis, cavernomatous degeneration of the portal vein, and splenic vein thrombosis. Other causes, to a lesser degree, are congenital malformations of the portal vein and Klatskin tumor. The first 2 of the abovementioned pathologies are the most studied. The primary initial clinical manifestation of prehepatic portal hypertension is upper gastrointestinal bleeding; close to 90-95% of these patients have esophageal varices and 35-40% have gastric varices.5
Doppler USG, splenoportography, magnetic resonance angiography, and angiotomography are among the diagnostic studies utilized for this disease.
There are 2 important treatment aspects: a)medical treatment, with medications like propranolol, ranitidine, or a proton pump inhibitor; 2)endoscopic treatment of varices; there are few pediatric studies comparing ligation versus sclerotherapy, and 3)surgical treatment, with portosystemic shunts (total or selective), splenectomy, or partial embolization.
The primary aim of this study was to determine the main clinical, radiologic, and endoscopic characteristics of patients upon diagnosis with prehepatic portal hypertension at the Instituto Nacional de Pediatría within the time frame of January 2001 and December 2011.
MethodsAn observational, descriptive, retrolective, and cross-sectional study was conducted. The protocol was accepted by the Research and Ethics Committee of the Instituto Nacional de Pediatría. A search of the Clinical Archive database of all the medical records with confirmed diagnosis was carried out. Fifty-two clinical case records were obtained of patients seen at the institution from January 1, 2001 to December 31, 2011. Of these, 32 had prehepatic etiology and were included in the review. Demographic, clinical, imaging, and treatment (medical and surgical) variables were analyzed. Employing the SPSS software version 19.0, the quantitative variables were analyzed through the descriptive statistics of measures of central tendency, dispersion, and normality tests and the categorical variables through frequencies and percentages.
ResultsThe diagnoses contained in the 52 medical records initially reviewed were distributed as follows:
Prehepatic portal hypertension: 32 patients (61.5%).
Presinusoidal intrahepatic portal hypertension: 6 patients (11.5%), all diagnosed with hepatoportal sclerosis.
Sinusoidal intrahepatic portal hypertension: 12 patients (23%). The reported diagnoses were: biliary atresia (5), autoimmune hepatitis (3), neonatal hepatitis (1), lysosomal disease (1), liver abscess (1), and alpha1 antitrypsin deficiency (1).
Posthepatic portal hypertension: 2 patients (4%): one patient with scimitar syndrome and the other with altered flow of the inferior vena cava.
Thirty-two patients diagnosed with prehepatic portal hypertension were included in this study: 12 patients (37.5%) were female and 20 (62.5%) were male. The median age at the time of diagnosis was 107 months (minimum of 3 months and maximum of 181 months), of which 4 children (12.5%) were 0 to 12 months old, 15 (46.88%) between 1 and 4 years old, 7 (21.88%) between 5 and 9 years old, 5 (15.62%) between 10 and 13 years old, and one case (3.12%) between 14 and 18 years old. The median weight was 17kg (a minimum of 4.06 and maximum of 62kg). The median height was 102cm (a minimum of 58cm and maximum of 162cm).
Clinical symptomsThe main reason medical consultation was sought was upper gastrointestinal bleeding with anemia (defined as a reduction in hemoglobin of more than 2g from the baseline value or hemodynamic repercussion) in 23 cases (71.9%); hypersplenism in 5 cases (15.6%) (characterized by leukopenia and thrombocytopenia), upper gastrointestinal bleeding without anemia in 2 cases (6.3%), and isolated splenomegaly in 2 cases (6.3%).
DiagnosisThe principal diagnosis was cavernomatous degeneration of the portal vein in 21 cases (65.6%), followed by portal vein thrombosis in 6 cases (18.8%), and splenic vein thrombosis in 5 cases (15.6%). The previous placement of an umbilical catheter was reported in only 10 cases, and proteinC and S deficiency was found in only 2 cases.
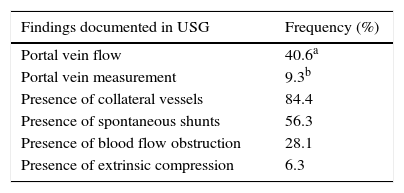
Imaging studiesDoppler USG was carried out on all the patients. Portal vein flow measured in cm/s with a minimum value of 11, a maximum value of 50, and a median value of 21.3 was described in 13 patients (40.6%). In order of frequency, the USG reported the presence of collateral circulation in 27 patients (84.4%), blood flow obstruction in 18 patients (56.3%), spontaneous shunts in 9 patients (28.1%), and extrinsic compression in 2 patients (6.3%) (table 1).
Splenoportography was carried out on 17 of the 32 patients; it revealed a «balled up» image characteristic of portal vein cavernomatous degeneration in 7 cases (21.9%); an image of «blocked flow» was observed in 15.6% of the cases, corresponding to portal vein thrombosis; splenic vein obstruction was identified in 4 cases (12.4%); and the presence of collateral vessels was shown in only one case (3.1%).
Angiotomography was performed on only 5 patients (15.62%) and revealed splenomegaly in all of them, collateral vessels in 4, blood flow obstruction in 2, and spontaneous shunts in one case.
Magnetic resonance angiography was carried out on 14 patients (43.75%) and identified splenomegaly and collateral vessels in 13 patients, blood flow obstruction in 7 patients, and spontaneous shunts in 6 patients.
Medical and surgical treatmentIn relation to medical treatment, 65.5% of the cases (21 patients) received the combination of propranolol (dose of 1-2mg/kg/day) and a proton pump inhibitor (1mg/kg/day); 34.5% (11 patients) received propranolol and ranitidine at the time of diagnosis.
Initial panendoscopy reported: gradeiiesophageal varices in 12 patients (37.5%), gradeiii in 19 patients (59.4%), and no esophageal varices in one case (3.1%); gastroesophageal varices in 12 cases (37.5%), 9 of them with the GOV1 classification and 3 with GOV2 classification. Seventy-five percent of the patients (24 cases) presented with congestive gastropathy.
Variceal ligation was performed in 8 cases (25%) and sclerotherapy of esophageal varices in 5 cases (15.6%); the sclerotherapy was paravariceal in one of the cases and not specified in the other 4 cases. Sclerotherapy of gastric varices was carried out on 2 patients (6.2%); it was paravariceal in one of the cases and not specified in the other case.
Portosystemic shunting was performed on 17 patients (53.1%); 10 of those patients had mesocaval shunt placement and 7 had a splenorenal shunt. Nine patients (28.1%) underwent total splenectomy. Performing shunt placement in children depends more on the age of the patient than the diagnosis, on the caliber and anatomic situation of the vessels (analyzed through an imaging study that aids in evaluating the collateral veins and in determining which vein is the most appropriate for performing the diversion) and finally, the experience of the surgeon.
DiscussionIn our study, we found a 61.5% prevalence of prehepatic etiology in the portal hypertension cases, which is in accordance with the values described in the literature.3,4 Nevertheless, we believe there is an under-registering of cases of biliary atresia and other etiologies that progress to cirrhosis, and consequently to cases of intrahepatic portal hypertension; therefore we cannot affirm that prehepatic portal hypertension is the most frequent cause of all the portal hypertensions.
We found a higher frequency in males (62.5%) in our case series, which was interesting, given that this predisposition is not observed in other published reports. At the time of diagnosis, the values of the age, weight, and height variables were very different, which also is in contrast with that reported in the literature; in the majority of the studies, the patients are older than 4years of age, whereas in our series, 19 patients (59%) were diagnosed under the age of 4years.3–9
Upper gastrointestinal bleeding secondary to esophageal varices was the primary clinical manifestation at the time of diagnosis, correlating with that reported in the literature.3–9 Bleeding together with anemia was found in the majority of the cases (71.9%) and bleeding without anemia in 6.3%. This also correlates with studies in the literature stating that at the time of diagnosis, the majority of patients require transfusions of blood derivatives in order to achieve hemodynamic stability, resulting in a 2 to 5% mortality rate.5 It is striking that in the patients that were initially evaluated due to hypersplenism or isolated splenomegaly, the etiology was regarded as hematologic and oncologic. However, it should be kept in mind that that the cause could be prehepatic portal hypertension, as occurred with our patients. The leading case series7,8,10 describe cavernomatous degeneration and portal vein thrombosis as the main etiologic factors of this pathology, which is in accordance with the findings of our case series, in which we found that 84.4% of the cases, as a whole, corresponded to these pathologies.
Doppler ultrasound is the first imaging study that should be carried out in the initial approach to these patients,11 because it enables the measuring of flow velocity (measured in cm/s); according to the literature, the diagnosis of portal hypertension is made when there are values above 25-30. In our study, flow velocity was measured in just 13 of the patients, only 3 of which met the portal hypertension criterion of that value described in the literature. This is also an interesting finding, given that high sensitivity and specificity have been reported for this diagnostic study. However, it is possible that these values were actually higher, if we take into account the fact that the majority of patients presented with gradeii and iii esophageal varices at the time of diagnosis. Published reports indicate that USG reliably shows the presence of collateral veins and enables a nonspecific determination of the flow obstruction site. This concurs with our findings of collateral vessels (84.4% of the imaging studies) and blood flow obstruction (56.3%).5,11
Splenoportography was performed on approximately half of the documented patients (53%), and was the main diagnostic study in this group of patients from 2001 to 2006, the first 5years of the time frame of our analysis. As described in the literature, this technique stopped being used and has been replaced by angiotomography and magnetic resonance angiography because they provide the same information and are noninvasive studies,11–13 explaining why splenoportography was not indicated for the patients at the Instituto Nacional de Pediatría during the period of time corresponding to the last 5years of our study time frame.
There are no studies in the literature that compare angiotomography and magnetic resonance angiography and indicate that one diagnostic method is better than the other for this pathology. Both methods define images characteristic of collateral vessels, flow obstruction, spontaneous shunts, and splenomegaly; magnetic resonance angiography has a slightly higher sensitivity and specificity,11 depending on the researcher and the institution carrying out the study. Magnetic resonance angiography is performed more frequently (43.75%) than angiotomography; collateral vessels and splenomegaly were the most frequent findings in each of these methods.
Propranolol is mentioned in the literature as a regular part of medical treatment,14–17 and was indicated for 100% of the study patients. In recent studies, proton pump inhibitors are used to inhibit hydrochloric acid (taking into account their mechanism of action). Nevertheless, in our institution they were only prescribed to 65.5% of the patients. Ranitidine was indicated for the rest of the patients; this drug has not been the treatment of choice for the last few years, not only because of its limited action compared to that of the proton pump inhibitors, but also due to its high risk for tachyphylaxis.
Upper gastrointestinal bleeding secondary to esophageal varices is regularly described in the literature, reporting a prevalence of up to 90-95% in the patients with prehepatic portal hypertension.5 In our study, the presence of gradeii and iii esophageal varices made up 97% of the cases, explaining the high risk for bleeding and the reason for the first medical consultation. It has been stated that gastric varices may be present in up to 40% of cases; gastroesophageal varices were found in 37.5% of cases at the Instituto Nacional de Pediatría, but not a single case of isolated gastric varices. Gastropathy has been directly correlated with the degree of liver involvement;5 almost all of these patients present with gradeii and iii esophageal varices, which is directly correlated with the 75% prevalence of congestive gastropathy in this study.
The use of ligatures or sclerotherapy in the treatment of esophageal varices is controversial and there are few pediatric studies on this subject. Some reports have described both procedures as having long-term management efficacy, but ligation has been shown to reduce the number of sessions required and has a lower percentage of bleeding recurrence and secondary complications.16–18 In the present study, ligation was documented in 8 patients and sclerotherapy in 5. In the follow-up period, 4 more patients received sclerotherapy treatment. This is explained by the fact that in the first 5years covered in our review (2001 to 2006) the patients were quickly treated with portosystemic shunt placement, considerably reducing the grade of esophageal varices, and thus resulting in a smaller number of procedures. It is interesting to point out that although ligatures have been available at the Institute for only 5years, this procedure has been carried out more frequently than sclerotherapy, according to the data we collected.
We found no study indicating a predominance of a specific portosystemic shunt in this disease. They are recommended to always be evaluated individually, after documenting the collateral vessels, their distribution, and flow velocities and they should not be considered an emergency procedure.15,19 Portosystemic shunt was carried out on 17 cases (53%) in the present analysis. It is striking that all of the patients receiving a mesocaval shunt underwent this procedure during the first month of evaluation. Certain advantages to distal splenorenal shunt have been reported in relation to the rest of the total shunts,6,19 but mesocaval shunt (10 cases) predominated over distal splenorenal shunt (7 cases) in this study. The surgical option of splenectomy was contemplated in 9 patients, though it is not a first choice procedure in the follow-up of these patients.6
ConclusionsPrehepatic portal hypertension is an entity with a high morbidity rate, and therefore it is important that the physician be familiarized with this disease so that the patient can be referred to a tertiary care center for opportune diagnosis and treatment.
Financial disclosureNo financial support was received in relation to this study/article.
Conflict of interestThe authors declare that there is no conflict of interest.
Please cite this article as: Zárate Mondragón F, Romero Trujillo JO, Cervantes Bustamante R, Mora Tiscareño MA, Montijo Barrios E, Cadena León JF, et al. Características clínicas, radiológicas y endoscópicasal diagnóstico de los pacientes con hipertensión portal prehepática en el Instituto Nacional de Pediatría del 2001 al 2011. Revista de Gastroenterología de México. 2014;79:244–249.