The Bristol Stool Form Scale (BSFS) and a modified child-friendly version (M-BSFS) are frequently used in clinical practice and research. These scales have not been validated in children. 3-D stool scale models may be better adapted to the child's development.
AimsTo assess the usefulness of the BSFS, M-BSFS, and a newly developed 3-D stool scale in children.
MethodsFifty children were asked to rank the picture cards of the BSFS and 3-D models from hardest to softest and to match the pictures with descriptors for each stool type.
ResultsThirty percent of the children appropriately characterized the stools as hard, loose, or normal using the BSFS vs. 36.6% with the 3-D model (p=0.27). Appropriate correlation of stools as hard, loose, or normal consistency using the BSFS vs. the 3-D model by age group was: 6 to 11-year-olds, 27.5% vs. 33.3% (p=0.58) and 12 to 17-year-olds, 32.1% vs. 39.5% (p=0.41). Thirty-three percent correlated the BSFS pictures with the correct BSFS words, 46% appropriately correlated with the M-BSFS words, and 46% correlated the 3-D stool models with the correct wording.
ConclusionsThe BSFS and M-BSFS that are widely used as stool assessment instruments are not user-friendly for children. The 3-D model was not found to be better than the BSFS and the M-BSFS.
La Escala de Evacuación de Bristol (BSFS) y la versión modificadaamigable para pacientes pediátricos (BSFS -M) son utilizadas frecuentemente en la clínica y en la investigación. Estas escalas no han sido validadas para ser utilizadas en niños. Las modelos de escalas de Evacuación en 3D podrían ser mejor adaptadas a las etapas del desarrollo de los niños.
ObjetivoValorar la utilidad de la BSFS, M- BSFS y la recientemente creada escala de Evacuación en 3D en niños. Pacientes y Métodos: A 50 niños se les solicitó que clasificaran las tarjetas con las gráficas de la BSFS y de los modelos en 3D de las evacuaciones desde la de mayor consistencia hasta la más suelta y que relacionaran los dibujos con los descriptores para cada tipo de evacuación.
ResultadosTreinta por ciento de los niños caracterizaron correctamente las heces como duras, sueltas o normales utilizando la BSFS vs. 36.6% con el modelo en 3D (p=0.27). La correlación apropiada de la consistencia de la evacuación como dura, suelta o normal utilizando la BSFS vs. el Modelo 3D de acuerdo con la edad fue, 6-11 años de edad: 27.5% vs. 33.3% (p=0.58) y 12-17 años de edad: 32.1% vs. 39.5% (p=0.41). Treinta y tres por ciento correlacionó las gráficas de la BSFS con las palabras correctas de la BSFS, 46% las correlacionó apropiadamente con las palabras del BSFS-M y 46% correlacionó los modelos de Evacuación en 3D con las palabras correctas.
ConclusionesLas BSFS y las BSFS -M que han sido ampliamente utilizadas como instrumentos de valoración de la evacuación no son amigables para ser utilizados en niños. No se encontró que el modelo de 3D fuera más útil que el BSFS y el BSFS -M.
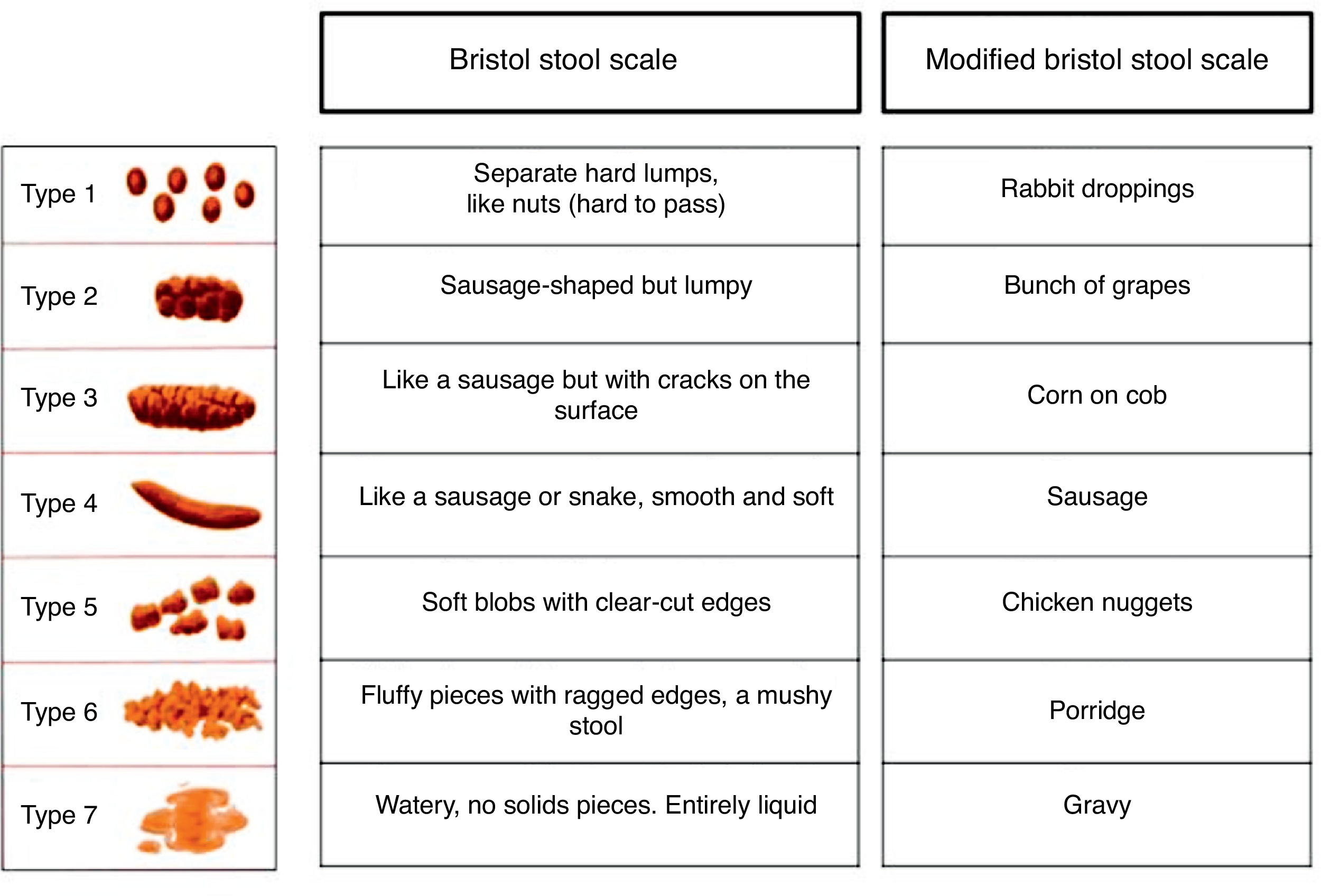
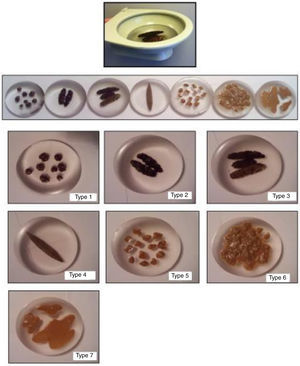
Constipation and irritable bowel syndrome (IBS) are among the most common gastrointestinal disorders in adults and children.1, 2, 3 Both of these conditions impose a substantial financial burden on the families and the healthcare system.4, 5, 6 Constipation and IBS cause physical and emotional distress and are associated with a significantly decreased quality of life.7, 8 Constipation has been shown to persist into young adulthood in one third of affected children. Approximately 50% of the children also experience at least 1 relapse within the first 5 years after initial successful treatment.9 The considerable morbidity and healthcare costs accompanying childhood constipation make it an important condition to diagnose and treat correctly. Diagnosis of constipation and IBS are clinical and based on the patient's report of symptoms and stool consistency. The patient's report of stool characteristics is used in the assessment of treatment efficacy to establish changes in medication and to evaluate clinical progress.10 In 1997, Lewis et al. developed the Bristol Stool Scale Form (BSFS) as a method of assessing intestinal transit time in adults (Figure 1).11 Since then, the BSFS has become the most widely used instrument for assessing stool characteristics.12, 13 The last edition of the Rome criteria recommends using the BSFS to evaluate stool form in adult patients with functional bowel disorders.14 Recently issued FDA draft guidelines recommended using the BSFS to assess primary end points in clinical drug trials.15 There is a need for validated stool scales to assess stool characteristics in children. Developmental limitations may hinder the child's utilization of scales specifically designed for adults. This has led to the development of a modified version of the BSFS.16 The modified version (M-BSFS) uses what were proposed as child-friendly descriptors for each of the seven pictorial stool depictions included in the BSFS (Figure 1). The psychometric characteristics of the BSFS or its modified version have not yet been studied in children. It is unclear whether children are able to conceptualize the pictures of the BSFS, whether the modified wording included in the M-BSFS is easier for children to understand, and whether other means of assessment including tridimensional models (3-D) of stools could be helpful in stool assessment by children. Evolving developmental stages make the child population unique. Piaget proposes that children progress through cognitive stages with distinct developmental differences between children 7 to 11 years of age (concrete operational state) and children older than 12 years of age (formal operational state).17 Children at the concrete operational level are at the initial stages of logical reasoning and coherent thought organization and can only think about actual physical objects, whereas they are unable to handle abstract reasoning. Children at the formal operational stage are able to think abstractly and better understand the form or structure of problems.
Figure 1. Bristol Stool Form Scale.
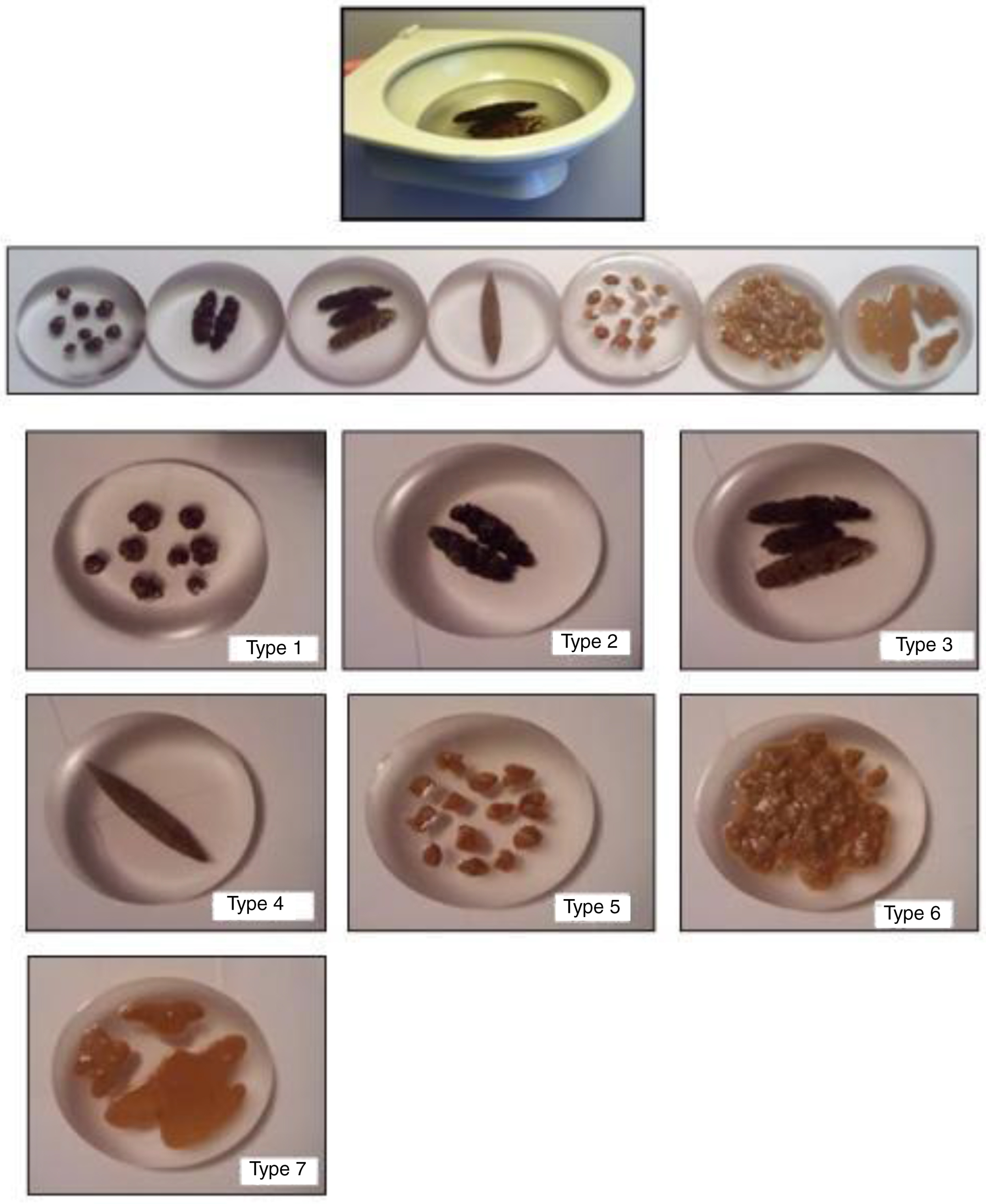
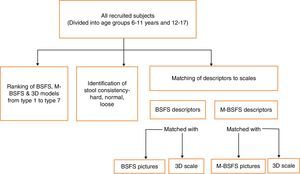
Taking into consideration these developmental stages, we designed a tridimensional stool assessment scale to evaluate whether the realistic depiction of stools influences the recognition of stool form and consistency in children. The tridimensional stool models were made out of resin, based on the BSFS pictures, with the help of a local independent artist specializing in plastic sculptures (Figure 2). We have conducted a study to compare the use of the BSFS, M-BSFS, and the newly designed tridimensional stool assessment instrument in children. Primary aim: To evaluate the use of the BSFS and M-BSFS in children. Hypothesis 1: Children are not able to accurately identify stool consistency using the BSFS or the M-BSFS. Hypothesis 2: M-BSFS descriptors do not improve the children's ability to characterize the stools in the scale. Secondary aim: To evaluate whether younger children can better identify stools types and consistency using the new tridimensional stool assessment instrument, compared with the BSFS or M-BSFS.
Figure 2. Tridimensional Stool Assessment Scale.
MaterialsBSFSThe BSFS (Figure 1) classifies stool forms into 7 categories ranging from hard stools (types 1 and 2) to loose stools (types 6 and 7) with an intermediate category considered as normal stools (types 3, 4, and 5). The BSFS is a vertical paper chart scale composed of 2-dimensional representations of the various stool types, each accompanied with a written description. The M-BSFS is an instrument available on the Internet that is currently used by some practitioners and pharmaceutical companies to characterize stools in children.16 No validation is available. The M-BSFS uses the same pictures of the BSFS with different descriptors. For this purpose the M-BSFS describes type 1 as “rabbit droppings”, type 2 as “bunch of grapes”, type 3 as “corn on cob”, type 4 as “sausage”, type 5 as “chicken nuggets”, type 6 as “porridge”, and type 7 as “gravy”.
The tridimensional stool assessment instrument: Due to the lack of information on whether children would benefit from a three-dimensional version of each stool type, a 3-D version of the BSFS was specially constructed by a local independent artist who specializes in making plastic models. He was provided with the BSFS for reference. The custom made 3-D models were constructed in resin and consisted of a 25 cm-high white mock toilet and seven 16.5 cm (diameter) × 3.5 cm (height) resin 3-D models depicting each BSFS stool type. The 3-D model included a clear material inside the mock toilet to represent water in the toilet bowl (Figure 2) and stools that “floated” or “sank” depending on the stool type. The mock toilet bowl was constructed to allow easy introduction and removal of each of the 7 types of stools from the bowl. Two focus group sessions were conducted with a group of 6 gastroenterology nurses and 6 pediatric gastroenterologists from our clinical division. Initial versions that were not immersed in clear resin (depicting water) were considered unsatisfactory by the focus group. The newer final version consisted of the stools set in clear resin which looked like stools floating/sunk in clear water in the toilet bowl. The final version of the 3-D (tridimensional stool assessment instrument) was considered to satisfactorily represent each stool type and the characteristics of children's stools.
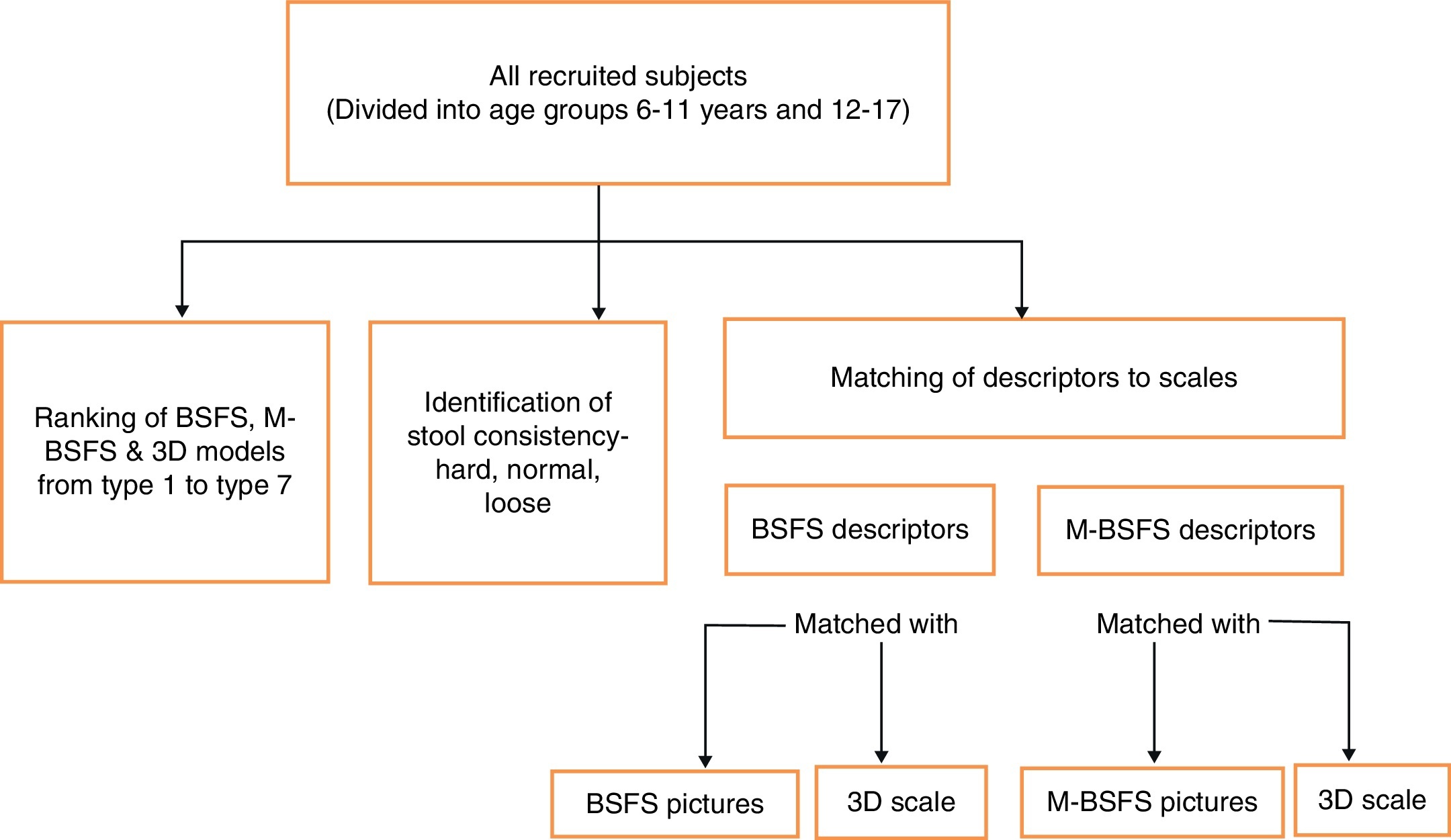
MethodsThis study was approved by the institutional review board (IRB) of Children's Memorial Hospital of Chicago. Children 6 to16 years of age seen at the pediatric gastroenterology clinic of Children's Memorial Hospital of Chicago during the time frame of 2009-2011 were invited to participate in the study during their visit. After informed parental consent was obtained, each child conducted a series of tasks to assess and compare the pictures and model depictions of the stools (A) and to compare the word descriptions of the BSFS and M-BSFS (B) (Figure 3). The parents gave their consent to a research assistant who also administered the tasks.
Figure 3. Study methodology.
A) Since the BSFS and M-BSFS utilize the same 2-D depictions (pictures) and the 3-D model utilizes resin models, tasks A1-A2 (see below) allowed us to i) assess the ability of children to identify stool consistencies using the BSFS and M-BSFS pictures and ii) to evaluate whether the use of the newly created 3-D models provided a comparative advantage in the assessment of stool consistency in children. For this purpose, the children were presented with the different stool types of the BSFS and 3-D model in random order. The 7 stool types of the BSFS were separated from the chart and enlarged to produce 7 independent 2-dimensional colored picture cards with white backgrounds measuring 5 × 3 cm corresponding to each stool type. The 7 stool types of the 3-D model were then presented in the mock toilet bowl in random order. Due to the relevance of the stool consistency construct in the assessment of constipation, children were assigned various tasks to determine their ability to understand this concept through (1) ordinal ranking of stool consistency and (2) identification of stool consistency through the BSFS and M-BSFS pictures and 3-D models.
Ordinal ranking of stool consistencyChildren were asked to identify decreasing stool consistency through the BSFS pictures and 3-D models. First, the children were asked to rank the picture cards of the BSFS from hardest to softest (type 1 to type 7). For this purpose, they were presented with the seven pictures in random order by a member of the research team. To explore whether a 3-D model was a suitable representation for children, the subjects were asked to rank the resin stool models from hardest to softest (type 1 to type 7). For this purpose, they were presented with the seven resin models depicting stool types of the BSFS in the mock toilet bowl water in random order by a member of the research team. Correlation between rank order of the BSFS and the subject's ranking was analyzed for the 2-dimensional colored picture cards and 3-D models.
Identification of stool consistencyTo assess the children's ability to correctly identify stool consistency using the BSFS pictures and 3-D models, we established whether the children's characterization of each stool type could be correctly considered as hard, loose, or normal. For this purpose, stool type determination was considered correct if the children identified the picture or 3-D model with a stool type in the range of hard stools (type 1, 2), loose stools (type 6, 7), or normal stools (type 3, 4, 5).
To assess the ability of children at different developmental stages to characterize stools as hard (type 1, 2), normal (type 3, 4, 5), and loose (type 6, 7), we compared two age groups: Group 1- preadolescent children, 6 to 11 years old and Group 2- adolescent children, 12 to 17 years old. B) Because the BSFS and M-BSFS use the same pictures but different words to describe the stools, tasks B1-B4 (See below) allowed us to compare and establish whether M-BSFS descriptors (that were intended to be easier to understand by children) behaved differently from BSFS descriptors that were originally designed to be used in adult patients.
1- To assess the ability of the BSFS descriptors to characterize the different stool types of the BSFS, the children were asked to match picture cards with the descriptions for each of the 7 stool types of the BSFS.
2- To assess the ability of the “child-friendly” descriptors of the M-BSFS to characterize the different stool type pictures, the children were asked to match the picture cards with the descriptions for each of the 7 stool types of the M-BSFS.
3 and 4- To further assess the behavior of the descriptors used in the BSFS and M-BSFS, children were asked to match each of the descriptors with the stool types of the 3-D model.
A sample size calculation showed that differences between age groups would have been significant for the BSFS with a sample of 199 children, using a power of 0.8 with a level of significance of 0.05. We limited the size of our recruited subject sample since this was a pilot study that we hope will lead to bigger multicenter studies to validate the various stool scales. Categorical differences were analyzed by chi-square and Fisher's exact tests. The P value was calculated using the unpaired two-tailed t test.
ResultsA total of 50 children with a mean age of 12.3 years (range 6-16 years) and 50% of which were girls participated in the study.
A-1: Ordinal ranking of stool consistencyOnly two percent of the children (one 15-year-old child) ranked all the BSFS picture cards correctly from hardest (type 1) to softest (type 7), and two percent of the children (one 17-year-old child) ranked the 3-D models correctly from hardest to softest. Only stool types 6 and 7 on the picture cards and the 3-D models were ranked correctly by >70% children. Children had 40.6% (SD 19.2%) correct answers when they ranked the picture cards versus 42.8% (SD 18.7%) with the 3-D models.
A-2: Identification of stool consistencyAn average of 30% of correct answers was found using the BSFS vs. 36.6% of correct answers with the use of the 3-D models (p = 0.27).
A-3: Conceptualization of stool consistency by age groupsThe analysis of the ability of different age group children to correctly classify each of the stool groups according to consistency categories was: Group 1- preadolescent children, 6 to 11 years old using the BSFS picture cards: hard (4.4%), loose (69.6%), and normal stools (8.7%); and the correct classification using the 3-D model: hard (8.7%), loose (82%), and normal stools (8.7%) (Table 1). Group 2- adolescent children, 12 to 17 years old using the BSFS picture cards: hard (3.7%), loose (88.9%), and normal (3.7%); and the correct classification using the 3-D model: hard (11.1%), loose (96.3%), and normal (11.1%) (Table 1). The correct characterization of all stool types using the BSFS was 27.5% in the children of the younger age group (6-11 years) and 32.1% in the older age group (12-17 years) (p = 0.59). The correct characterization of all stool types as hard, loose, or normal consistency using the 3-D models was 33.3% in children of the younger age group (6-11 years) and 39.5% in the older age group (12-17 years) (p = 0.49). When we compared the conceptualization of stool in children 6-11 years of age we found a cumulative correct assessment with the BSFS (27.5%) vs. the 3-D models (33.3%) (p = 0.58). In older children (12-17 years), we found similar results for the 3-D models (39.5%) in the appropriate classification of stool consistency in comparison with the BSFS (32.1%) (p = 0.41). The lack of significant difference using the BSFS and 3-D models in each age group suggests a similar level of understanding of the BSFS and the 3-D model between younger and older children.
Table 1. Characterization of stools: hard (type 1, 2, 3), loose (type 5, 6, 7) and normal (type 4).
| Hard | Loose | Normal | ||||||||||
| Group 1 n=23 (46%) | Group 2 n=27 (54%) | Overall correct response | Group 1 n=23 (46%) | Group 2 n=27 (54%) | Overall correct response | Group 1 n=23 (46%) | Group 2 n=27 (54%) | Overall correct response | ||||
| BSFS | 1 (4.3%) | 1 (3.7%) | 4% | P= 0.43 | 16 (69.6%) | 24 (89%) | 80% | P = 0.26 | 2 (8.7%) | 1 (3.7%) | 6% | P=0.71 |
| 3-D | 2 (8.7%) | 3 (11.1%) | 10% | 19 (82%) | 17 (96.3%) | 90% | 2 (8.7%) | 3 (11.1%) | 10% | |||
There was >70% agreement between the stool pictures and the appropriate words from the BSFS for stool types 2, 3, 4, 6, and 7. Eighteen subjects (33%) correlated the stool picture cards with the appropriate BSFS words.
Correlation between the picture cards and M-BSFS wordingAgreement between the stool pictures and the words from the M-BSFS were >70% for stool types 1, 3, 4, 5, 6, and 7. Twenty-four subjects (46%) correlated stool picture cards with the appropriate M-BSFS words. No significant difference was found upon comparing the correlation of the pictures cards with the BSFS and M-BSFS wording.
Twelve percent of the children (4 boys, 2 girls, mean age 14.5 years) correlated the stool picture cards with both the appropriate BSFS and M-BSFS words.
3 and 4- Correlation between the BSFS and M-BSFS wording with the 7 stool types of the 3-D modelTwenty-four subjects (46%) correlated the 3-D stool models with the appropriate BSFS words. Twenty-six subjects (52%) correlated the 3-D stool models with the appropriate M-BSFS words. BSFS and M-BSFS wording correlated equally with the 7 stool types of the 3-D model (p = 0.7).
There was >70% agreement between the 3-D stool models and the appropriate words from the BSFS for all stool types except type 5 and with the appropriate words from M-BSFS for all stool types except type 2. Twenty-eight percent of the children (8 boys, 6 girls, mean age 15.3 years) correlated 3-D stool models with the appropriate BSFS and M-BSFS words.
The results of the various assessments of this section suggest poor behavior of the wording of the BSFS and M-BSFS and no benefit from the wording of the M-BSFS in children when compared with the original wording of the BSFS.
DiscussionThe BSFS is widely used in patients with functional gastrointestinal disorders (FGIDs) in clinical care. Adults and children with IBS and constipation are often asked to maintain a stool diary to evaluate their stool consistency and to make necessary changes in their treatment. The BSFS has been used along with stool diaries to help the patients record the type of stools. The BSFS has also been endorsed by the FDA and the Rome criteria to evaluate stool form in adult patients with functional bowel disorders14, 15. Despite its widespread use few studies have validated the BSFS in adults or children for these purposes10, 18, 19. We have found that the BSFS and the proposed modification of the instrument, the M-BSFS, did not perform well in children. Children of all ages demonstrated a poor ability to correctly rank stool consistency with both the 2-D and 3-D based instruments (BSFS/M-BSFS and tridimensional stool assessment scale). Children were only able to satisfactorily characterize loose stools using the BSFS/M-BSFS, whereas their characterization of hard and normal stools was very poor. This is particularly troublesome as the instrument is mostly used and recommended to diagnose constipation and IBS-C (the most common type of IBS in children). We found that children of all ages could use the BSFS and the 3-D stool models equally and there was no advantage of the 3-D models over the BSFS and M-BSFS pictures. The word descriptors performed poorly with the BSFS, the M-BSFS pictures, and also the tridimensional stool assessment scale. There was no significant difference between the ability of the children to correctly correlate the stool depiction using the BSFS wording and the supposedly child-friendly wording of the modified version (M-BSFS).
The age groups in our study closely resemble Piaget cognitive development age groups. We attempted to establish whether 3-D models would help younger children to evaluate stool consistencies better than picture-based scales. We found no obvious advantage of using 3-D models in any age category. We found that the percentage of children at the formal operational stage that could correctly characterize the various stool types was similar to the percentage of children that were able to correctly characterize the various stool types at the concrete operational stage. When compared with the BSFS, the use of our newly designed tridimensional stool assessment instrument resulted in an almost equal percentage of correct stool type characterization as hard, loose, and normal stools.
The poor performance of the currently used instruments (BSFS and M-BSFS) in our study, especially with younger children, is challenging. We can interpret our data as demonstrating an evidence of non-superiority of the 3-D stool model scale in its current form over the BSFS. Uncertainty about the validity of available instruments is not limited to the pediatric population. Studies have shown that adult patients are often confused when using the BSFS.20 Inadequate expectations not based on children's developmental abilities may be a consequence of using adult-based instruments in children. It may be unrealistic to expect children to be able to classify stool types into 7 different categories. The tridimensional stool assessment instrument may constitute a better instrument if some of the stool types were eliminated and it could then be potentially used at various ages without developmental distinction. A modified pediatric version of the BSFS by Chumpitazi et al. has been recently developed. This 5 stool form-type version of the BSFS has been shown to be reliable in a sample of 191 children.10 It is possible that a 5 stool-type version of our tridimensional stool assessment instrument may result in a more accurate characterization of stool types. We found >70% of correct agreement between the tridimensional stool assessment instrument and the BSFS wording for all stool types except type 5. Interestingly, Chumpitazi et al. also exclude type 5 from their abbreviated version of the BSFS. The authors did not compare their abbreviated version with the original BSFS version.
The strengths of our study include the comparison of our newly developed tridimensional stool assessment instrument with the widely used BSFS and M-BSFS and the investigation of the psychometric characteristics of the currently used scales at different ages. Cognizant of children's developmental stages, we have investigated the use of 3-D models as diagnostic tools in pediatric gastroenterology for first time. The use of focus groups has helped us guarantee the accuracy of our models by ensuring that they are truly representative of the stool types and that they look realistic. Due to concerns that 2-D pictures may not be appropriate for characterizing stools in children with a limited capacity for abstraction, we have placed all stool types in a mock toilet bowl to simulate the stools in a real-world setting. We believed that the use of 3-D models could maximize the child's capability of identifying the different types of stool forms, however we did not find an advantage in using 3-D models.
This was a prospective study with children recruited from the pediatric GI clinics at our hospital. Limitations of our study include the lack of multicenter evaluation. Our study population might not represent the entire pediatric population.
The limited size of our sample may have resulted in the study being underpowered. A larger study is certainly warranted to evaluate the properties and practical utility of these scales.
Future studies should compare the validity of 5-type and 7-type stool scales and our newly developed tridimensional stool assessment instrument with the 5 stool- type version developed by Chumpitazi et al.
ConclusionWe have shown that available and widely used stool assessment instruments are not user-friendly in children. The use of a tridimensional stool assessment instrument should be further investigated.
Financial disclosureNo financial support was received in relation to this study.
Conflict of interestThe authors declare that there is no conflict of interest.
Received 14 March 2013
Accepted 17 April 2013
Corresponding author: Division of Pediatric Gastroenterology, Hepatology, & Nutrition,Ann & Robert H. Lurie Children's Hospital of Chicago, 225 E. Chicago Ave, PO box # 65, Chicago, IL 60611. Tel.: +312 227 4607; fax: +312 227 9391. achogle@luriechildrens.org