A 21-year-old man, with no personal medical history, was admitted to the internal medicine service due to intermittent fever of 2-month progression, accompanied by generalized adenopathies. The patient stated he had no abdominal pain, diarrhea, or any change in bowel habit. As part of the evaluation, a fecal calprotectin test was carried out. The result was 250 µg/g, and so endoscopic studies were performed.
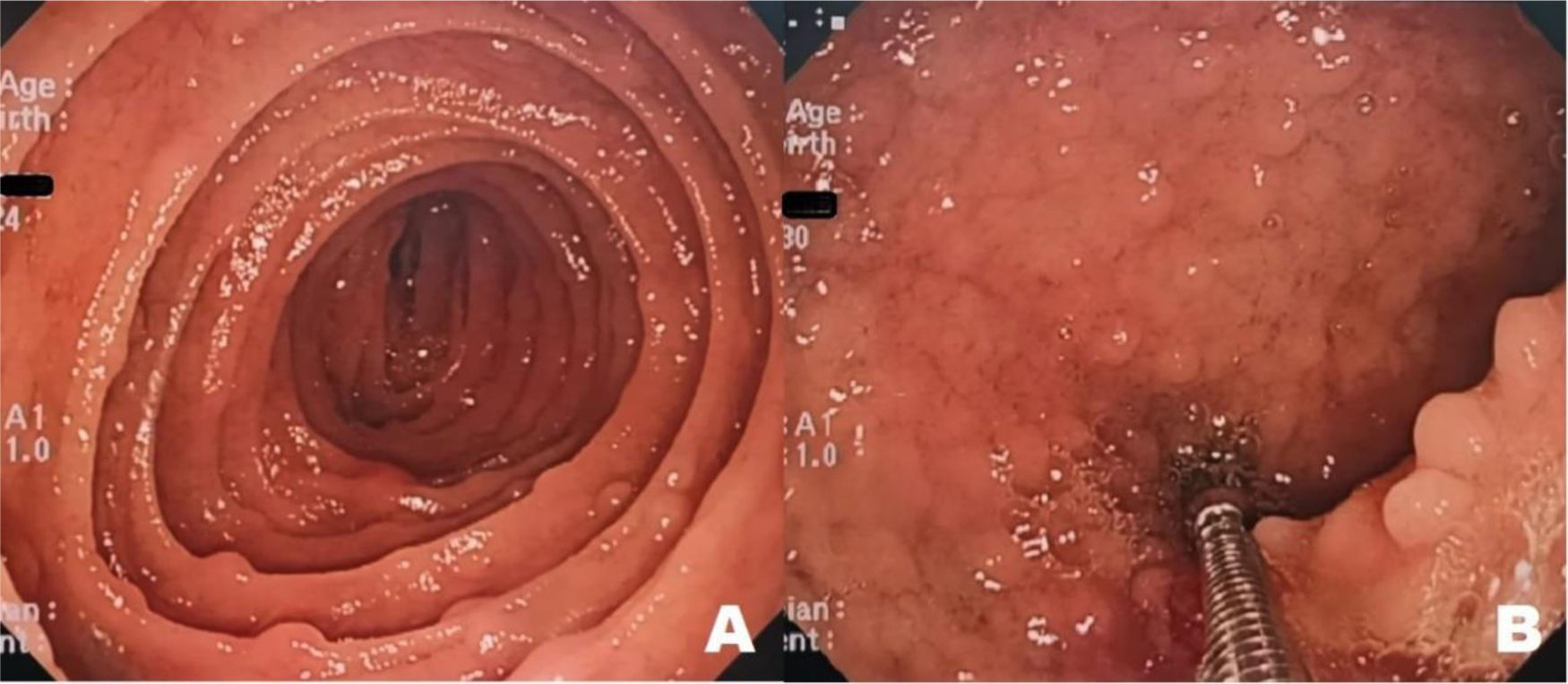
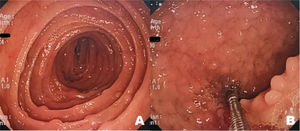
Upper gastrointestinal (GI) endoscopy revealed multiple elevated nodular lesions, smaller than 5 mm, at the level of the duodenum and the first jejunal segments. The lesions were rose-colored, as was the surrounding mucosa, and were present along the entire circumference of the organ (Fig. 1A and B).
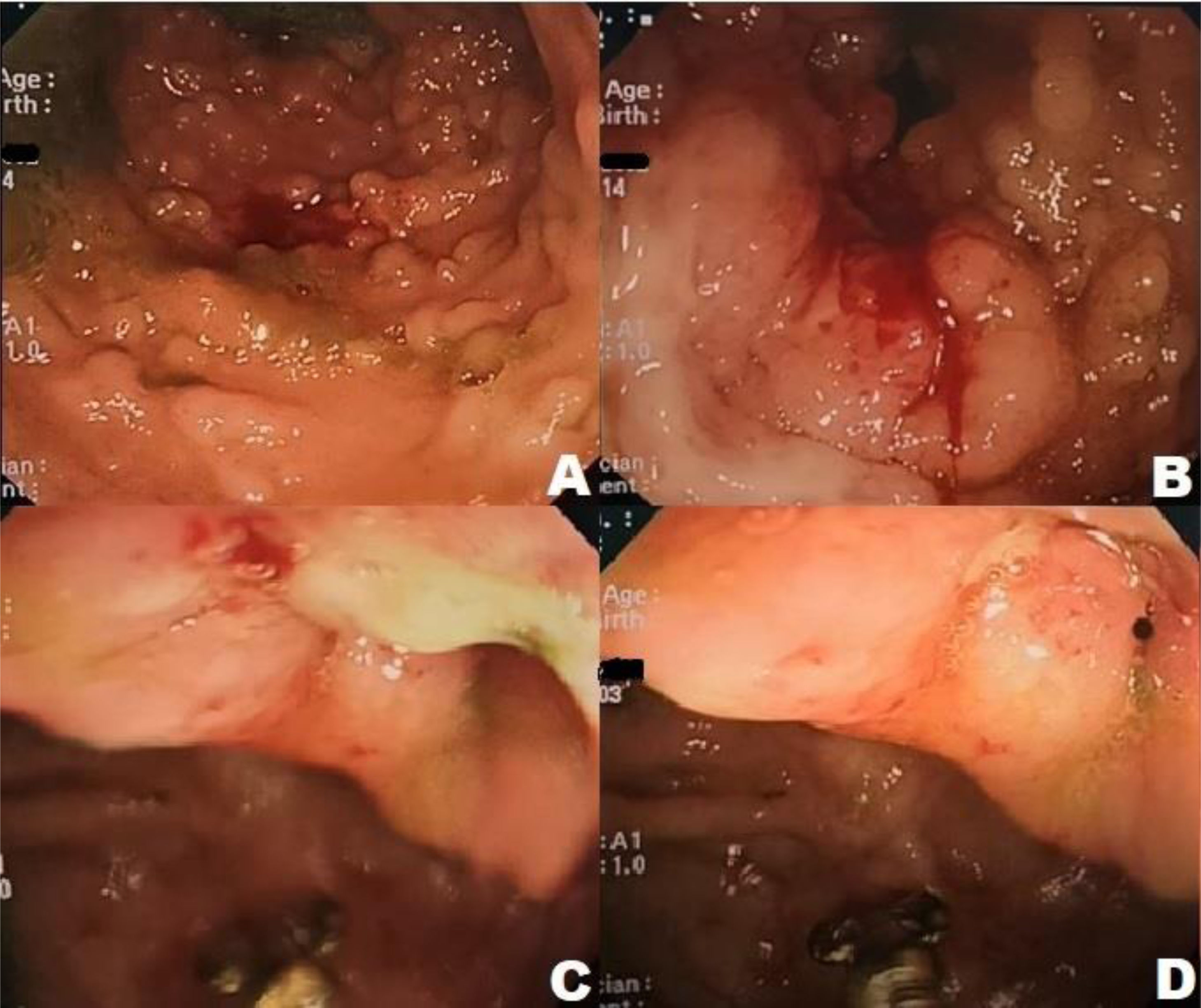
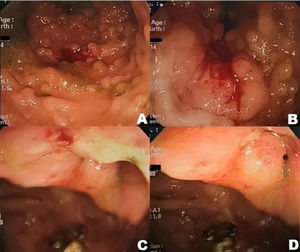
The colonoscopy study identified elevated pseudopolypoid lesions at the level of the ileum (Fig. 2A), as well as a superficial linear transverse ulcer, with a fibrinous base (Fig. 2B). An edematous ileocecal valve was observed, that had a superficial, oval-shaped ulcer, measuring approximately 1.5 cm in diameter, with irregular edges and a whitish, fibrinous base. The mucosa surrounding the ileocecal valve was normal (Fig. 2C and D). Given the endoscopic findings, inflammatory bowel disease, specifically Crohn’s disease (CD), with moderate endoscopic activity (CDEIS 10), was diagnosed.
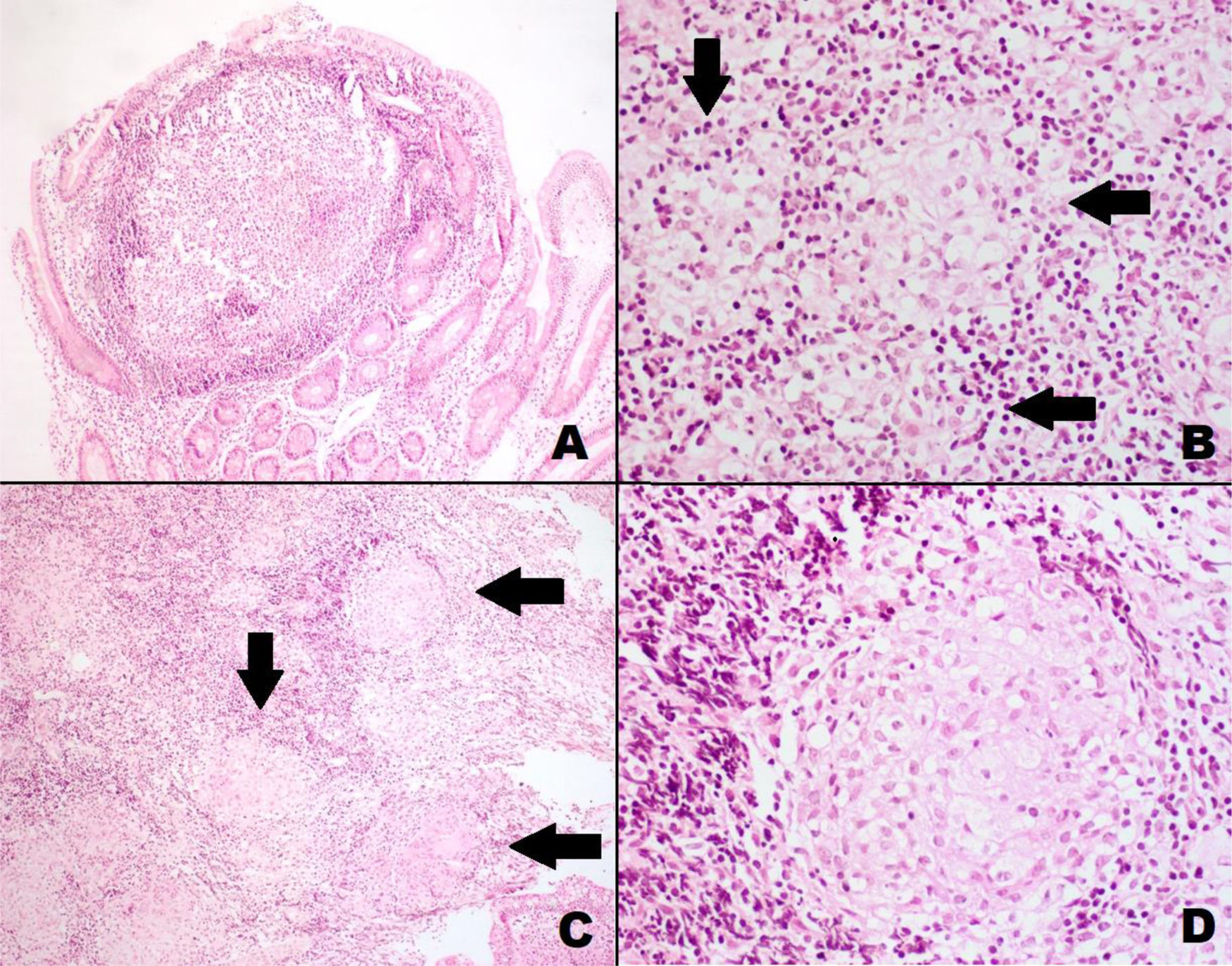
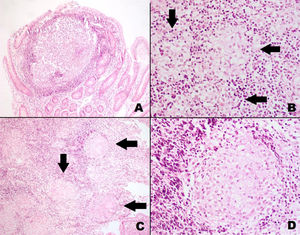
The histology study of the lesions documented in the upper GI endoscopy reported tuberculoid granulomatous chronic duodenojejunitis and tuberculoid granulomatous chronic enterocolitis with ulceration, which are results consistent with tuberculous infection (Fig. 3A–D).
A) Pseudopolypoid lesion in the small bowel. The formation of a nodule can be seen, with a central accumulation of histiocytic cells and a periphery of lymphocytes (H&E ×100). B) Small bowel with histiocytic clear cells, grouped and organized with a tendency to form microgranulomas (arrows) (H&E ×200). C) Small bowel with multiple solid granulomas (arrows) and diffuse lymphocytic infiltrate (H&E ×100). D) Solid granuloma in the small bowel, with multinucleated giant histiocytic cells and clear cytoplasm (H&E ×200).
The patient had two positive sputum cultures (code 8). A chest x-ray identified small well-defined nodular lesions, with central distribution in the upper lobe of the right lung, and the presence of mediastinal adenopathies. Those data confirmed extrapulmonary tuberculosis (TB), exposing the misdiagnosis resulting from the endoscopic examinations. The patient was given anti-tuberculosis treatment and discharged.
TB is a prevalent disease in developing countries and is currently on the rise in developed countries, as a consequence of the increase in immunocompromised patients, patients with AIDS, and migration.1 Intestinal TB accounts for 0.5–2%1 of the types of TB. It is a rare presentation, corresponding to 11%2 of the extrapulmonary forms.
Endoscopic images of TB are very similar to those seen in CD, making endoscopic diagnosis a challenge, resulting in misdiagnoses, as occurred in the case presented herein. Histologic study is very useful for making the definitive diagnosis.
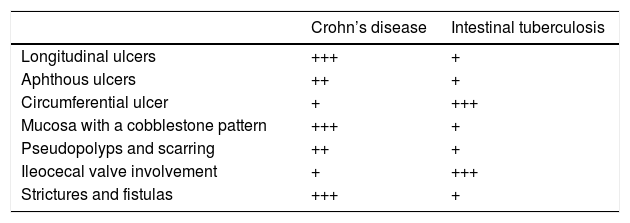
Both entities can affect any part of the digestive tract, from the esophagus to the rectum.3 There are endoscopic characteristics that differentiate CD from intestinal TB. Longitudinal, linear, or serpiginous, deep, aphthous ulcers are more frequent in CD and contrast with the transverse, circular, oval-shaped, shallow ulcers of TB. The presence of pseudopolyps, strictures, or nodular mucosa present in the two entities but do not differentiate one disease from the other.3–4 In addition, TB has a greater predilection for affecting the ileocecal valve, compared with CD, which more commonly affects the terminal ileum.4–5Table 16,7 summarizes the characteristics and frequency of presentation of the two diseases.
Endoscopic characteristics for differentiating Crohn’s disease from intestinal tuberculosis.6,7.
| Crohn’s disease | Intestinal tuberculosis | |
|---|---|---|
| Longitudinal ulcers | +++ | + |
| Aphthous ulcers | ++ | + |
| Circumferential ulcer | + | +++ |
| Mucosa with a cobblestone pattern | +++ | + |
| Pseudopolyps and scarring | ++ | + |
| Ileocecal valve involvement | + | +++ |
| Strictures and fistulas | +++ | + |
With respect to endoscopic location as a predictive factor for differentiating between the two entities, involvement of the perianal region, rectum, and sigmoid colon is predictive of CD, whereas involvement of the ileocecal valve is predictive of TB. Involvement of the ileum, cecum, and the ascending, transverse, and descending colon is not significantly different in the two diseases.4,8
The fecal calprotectin test is useful for discriminating between an organic and a functional digestive pathology and has 84–90% sensitivity and 66–79% specificity, with a cutoff value >200 µg/g.9 Fecal calprotectin levels are 5 to 40-times higher in inflammatory and organic diseases. The test can be very useful for diagnosing inflammatory bowel disease, when it reports very high values. Nevertheless, it is limited by the fact that levels can also be high because of other causes and factors, such as intestinal infections. The present case was a bacterial infection due to intestinal TB.7,10–11
The clinical characteristics of patients with TB are broad and varied, which is why it is known as the “great simulator”. Abdominal pain, fever, and anorexia are common symptoms in TB and CD. Purely symptomatologic orientation in the present case was complex. In several studies, the presence of perianal disease, extraintestinal manifestations, diarrhea, and rectal bleeding was more frequent in CD, whereas fever, night sweats, and weight loss were more frequent in intestinal TB.8 Symptom duration and characteristics are important because they can aid in guiding the physician toward the diagnosis. CD has a long progression, with episodes of flares and remission. However, the symptoms are not pathognomonic of either disease and cannot be used on their own, in the differential diagnosis of CD and TB. Table 2 summarizes the clinical symptoms of both entities and their presentation frequency.6–8
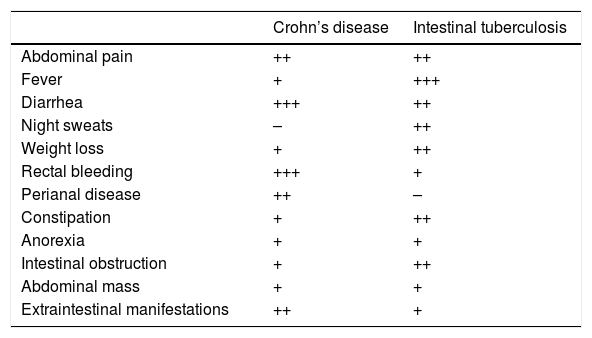
Clinical characteristics of patients with Crohn’s disease and intestinal tuberculosis.6–8.
| Crohn’s disease | Intestinal tuberculosis | |
|---|---|---|
| Abdominal pain | ++ | ++ |
| Fever | + | +++ |
| Diarrhea | +++ | ++ |
| Night sweats | – | ++ |
| Weight loss | + | ++ |
| Rectal bleeding | +++ | + |
| Perianal disease | ++ | – |
| Constipation | + | ++ |
| Anorexia | + | + |
| Intestinal obstruction | + | ++ |
| Abdominal mass | + | + |
| Extraintestinal manifestations | ++ | + |
Even though the clinical and endoscopic characteristics described herein are not characteristics of each entity, they are valuable for orienting the physician toward an accurate diagnosis, thus reducing the number of cases of intestinal TB misdiagnosed as CD. The usefulness of the fecal calprotectin test in the differential diagnosis of CD and TB is limited, given that both entities have elevated values of the biomarker, albeit very high values are suggestive of CD. Its main usefulness is in aiding the physician to determine a functional pathology, and in turn, make the decision to perform endoscopy.
Ethical considerationsThe authors declare that they met all ethical responsibilities regarding data protection, right to privacy, and informed consent.
Approval by an institutional ethics committee was not required, given that patient anonymity norms were not broken, nor were any experimental procedures performed that could have put the patient at risk.
The authors declare that the present article contains no personal information that could identify patients.
Financial disclosureNo financial support was received in relation to this article.
Conflict of interestThe authors declare that there is no conflict of interest.
Please cite this article as: Aguirre-Padilla LM, Madrid-Villanueva BE, Ugarte-Olvera ME, et al. Tuberculosis y enfermedad de Crohn. Desafío en el diagnóstico endoscópico. Reporte de caso. Revista de Gastroenterología de México. 2022;87:113–116.