Anal sphincter spasm contributes to the appearance of postoperative pain following hemorrhoidectomy.
AimTo determine the efficacy of topical diltiazem in the control of post-hemorrhoidectomy pain.
Material and methodsA randomized, prospective, experimental, double-blind study was conducted on 2 groups of patients in the postoperative period of closed hemorrhoidectomy. Each group consisted of 17 patients. Group A received topical diltiazem in the anal region 3 times a day and group B received a placebo. Ketorolac was administered to both groups as rescue therapy.
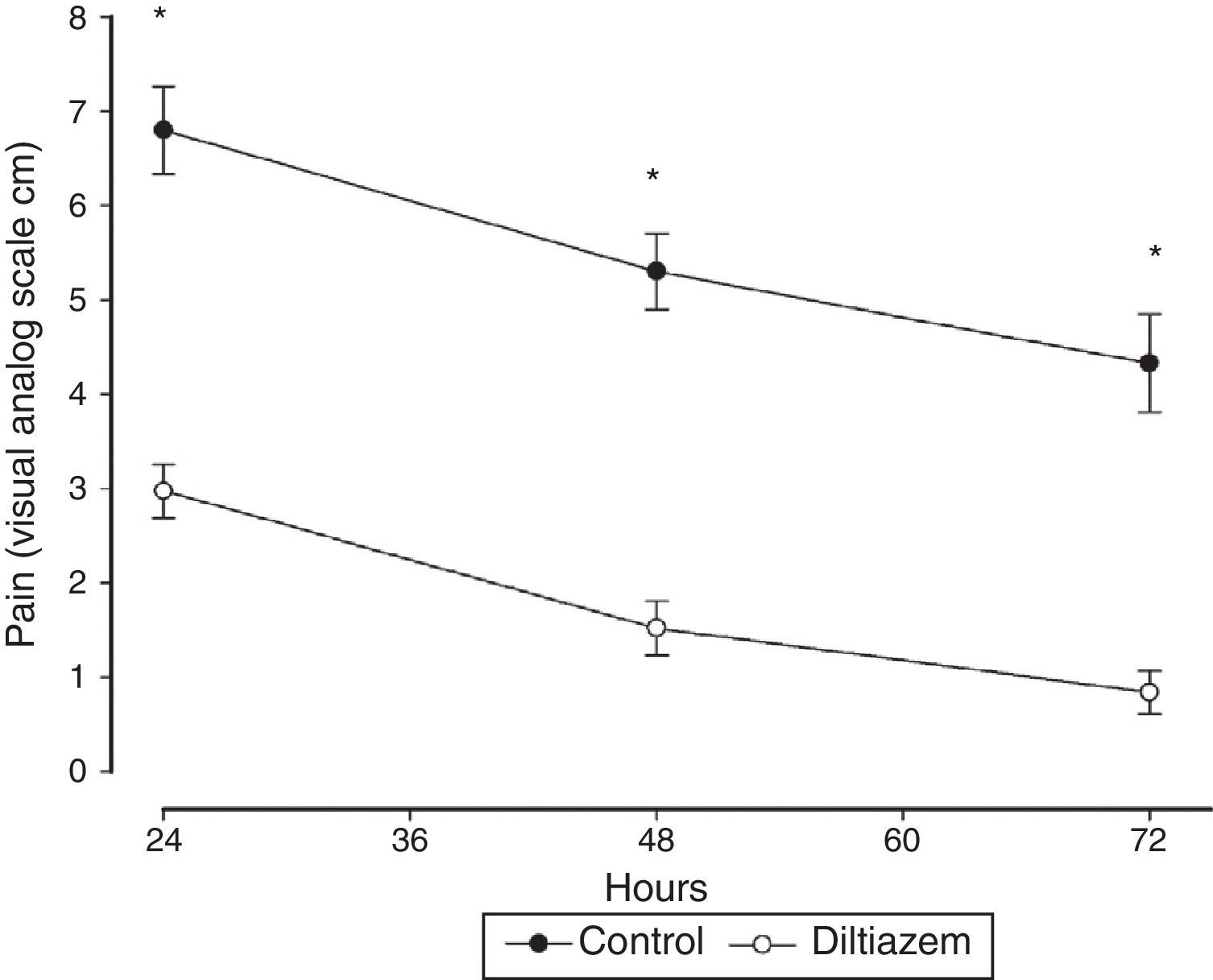
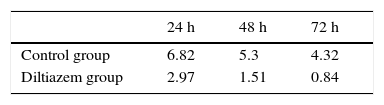
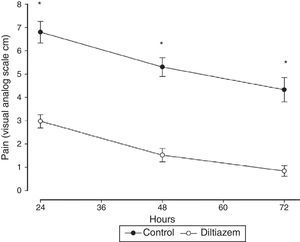
ResultsIn group A, the mean score on the visual analog scale was 2.97±1.18cm at 24h, 1.51±1.18cm at 48h, and 0.84±0.92cm at 72h. In group B, it was 6.82±1.9cm at 24h, 5.3±1.66cm at 48h, and 4.32±2.13cm at 72h (P<.001, 95% CI).
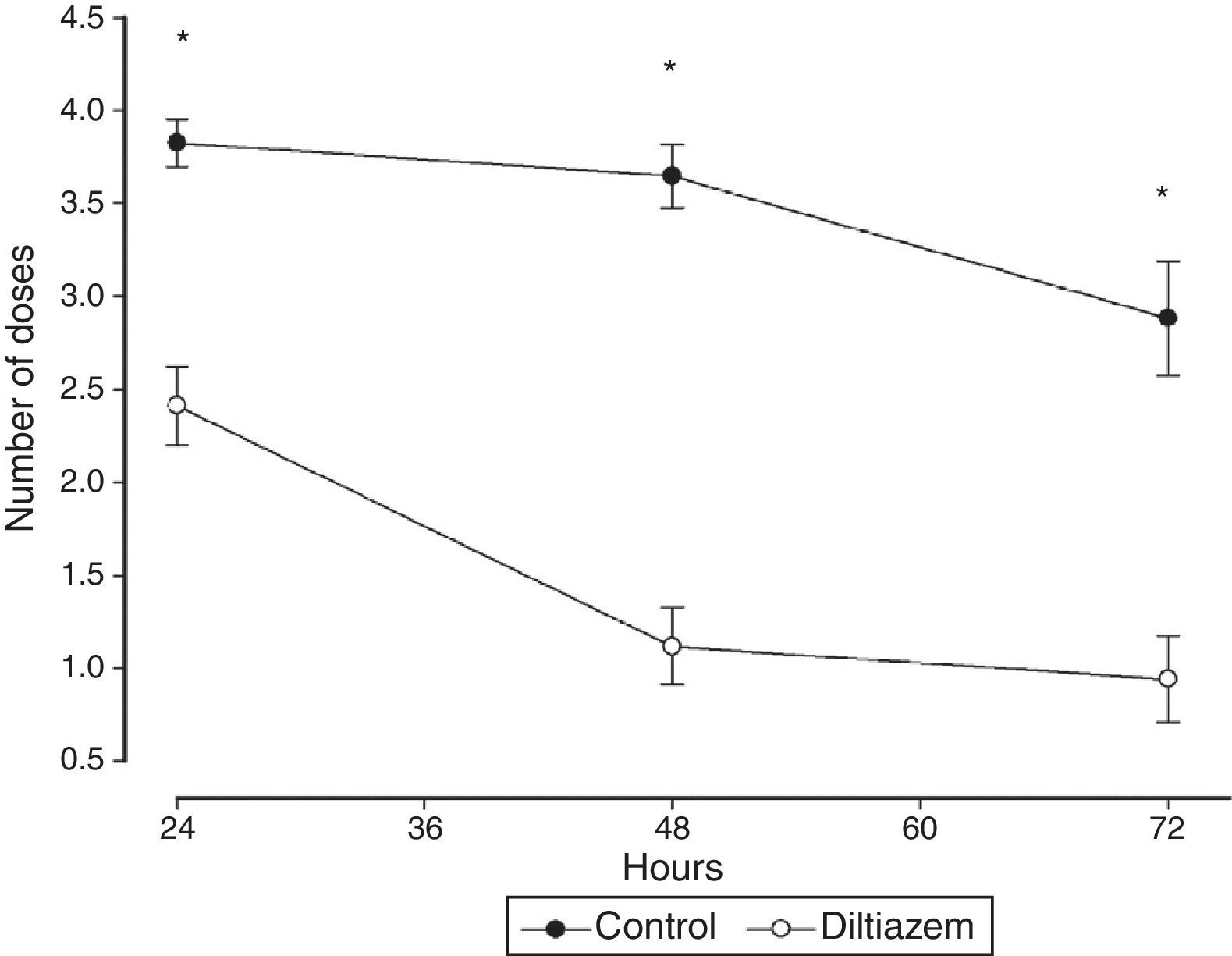
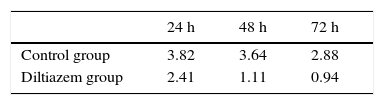
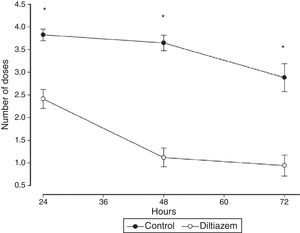
The mean number of analgesic doses in group A was 2.41±0.87 at 24h, 1.11±0.85 at 48h, and 0.94±0.96 at 72h. In group B, it was 3.82±0.52 at 24h, 3.64±0.70 at 48h, and 2.88±1.26 at 72h (P<.001, 95% CI).
ConclusionsIn this study, topical administration of diltiazem resulted in a statistically significant reduction of postoperative pain in patients that underwent closed hemorrhoidectomy.
El espasmo del esfínter anal contribuye a la aparición del dolor postoperatorio después de una hemorroidectomía.
ObjetivoDeterminar la eficacia del diltiazem tópico en el control del dolor postoperatorio de hemorroidectomía.
Material y métodosSe realizó un estudio aleatorizado, prospectivo, experimental, doble ciego, en 2 grupos de pacientes en el postoperatorio de hemorroidectomía con técnica cerrada. Cada grupo incluyo a 17 pacientes, el grupo A recibió diltiazem tópico en la región anal 3 veces al día y el grupo B recibió un placebo. En ambos grupos se administró ketorolaco por vía oral como terapia de rescate.
ResultadosEn el grupo A el promedio de calificación de la escala análoga visual fue de 2.97±1.18cm a las 24 h, 1.51±1.18cm a las 48 h y 0.84±0.92cm a las 72 h. En el grupo B fue de 6.82±1.9cm a las 24 h, 5.3±1.66cm a las 48 h y 4.32±2.13cm a las 72 h (p<0.001, IC del 95%).
El promedio de número de dosis de analgésico en el grupo A fue de 2.41±0.87 a las 24 h, 1.11±0.85 a las 48 h y 0.94±0.96 a las 72 h. En el grupo B fue de 3.82±0.52 dosis a las 24 h, 3.64±0.70 dosis a las 48 h y 2.88±1.26 a las 72 h (p<0.001, IC del 95%).
ConclusionesEn este estudio, el diltiazem administrado por vía tópica disminuyó el dolor, en los pacientes postoperados de hemorroidectomía con técnica cerrada, de manera estadísticamente significativa.
Seventy-seven percent of patients are estimated to present with pain after a surgical procedure and of those, 80% refer to it as moderate-to-severe intensity.1 The pain associated with the surgical treatment of hemorrhoidal disease is not considered a complication of this procedure in itself, but it is the main reason why patients with hemorrhoidal disease avoid treatment.2
For the purpose of reducing pain in the treatment of hemorrhoidal disease, attempts have been made to improve the surgical techniques, analgesic procedures, and general postoperative management measures.3
In virtue of the fact that anal sphincter spasm could play an important role in the appearance of postoperative pain after hemorrhoidectomy, partial anal sphincter sphincterotomy has been suggested as an alternative for reducing this pain.4 Even though some authors state that there are no significant differences in relation to anal sphincter continence, when sphincterotomy is added during hemorrhoidectomy, the risk for anal incontinence in these patients is high. Therefore, sphincterotomy is not recommended in the postoperative period of hemorrhoidectomy, unless there is an associated anal fissure.2 In an effort to prevent this complication, some topical medications, such as nitroglycerine, botulinum toxin, and diltiazem (DTZ), have been used to relax the anal sphincter and reduce pain.5
The aim of this work was to determine the efficacy of topical diltiazem in the control of post-hemorrhoidectomy pain.
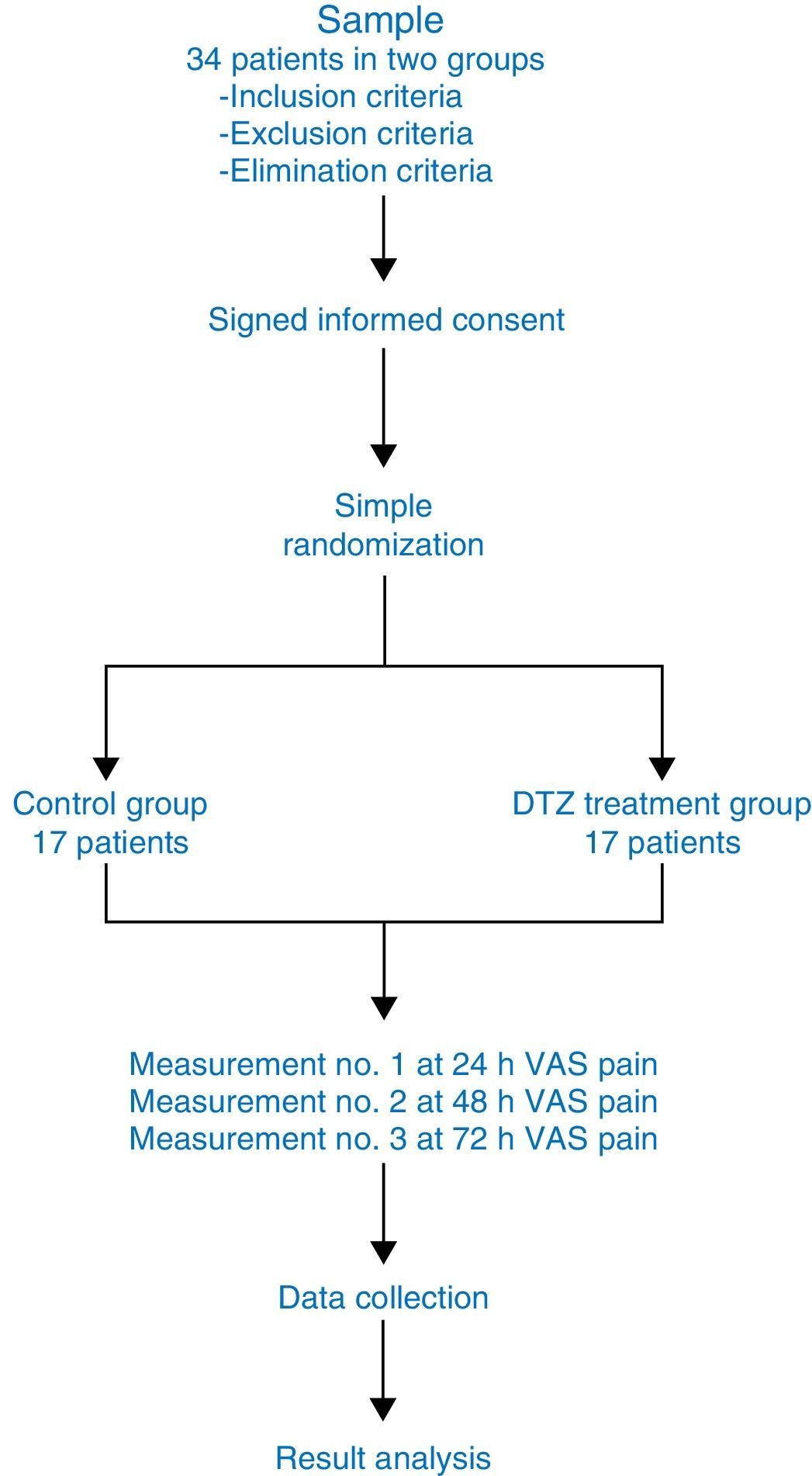
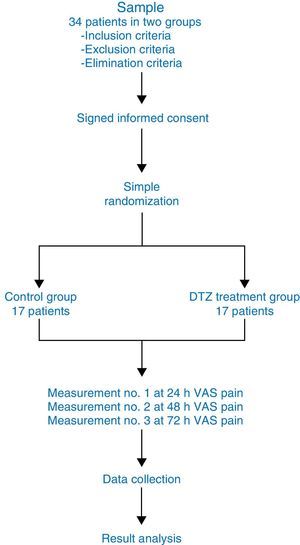
MethodsA simple, randomized, experimental, prospective, longitudinal, and double-blind study was conducted. All 34 patients that underwent the Ferguson closed hemorrhoidectomy for grade III and grade IV hemorrhoidal disease were operated on by the same surgeon. The patients were randomly divided into 2 groups of 17 patients each.
The inclusion criteria were: patients with grade III and grade IV hemorrhoidal disease and mixed hemorrhoidal disease that were surgically treated through closed hemorrhoidectomy.
The non-inclusion criteria were: patients under treatment with calcium channel blocking agents, patients that complained of previous collateral effects with the use of calcium channel blockers, and patients with a history of ischemic heart disease, pregnancy, severe high blood pressure, and orthostatic hypotension.
The exclusion criteria were applied as follows: patients with hemorrhoidal disease grades I and II and patients with hemorrhoidal disease grades III and IV that were treated with some other surgical procedure (circular stapler, transanal dearterialization, open hemorrhoidectomy). Finally, the elimination criteria corresponded to patients that did not give their informed consent.
The sample size of this study took into account that the current worldwide estimate of hemorrhoidal disease in the general population is 6%. Nevertheless, it is calculated that with the use of conservative measures and nonsurgical treatment procedures such as elastic band ligature, infrared photocoagulation, and sclerotherapy, only a quarter of the patients presenting with hemorrhoidal disease will require some type of surgical treatment. In other words, only 1.5% of the general population will require some type of surgical procedure. Closed hemorrhoidectomy is currently the most frequently performed surgical procedure for the treatment of hemorrhoidal disease, used in 70% of the cases. This implies that of the 1.5% of patients requiring surgical treatment, only 70% will be operated on with the closed technique. That is to say, 0.0105% of the population will require closed hemorrhoidectomy and therefore the p value (the population presenting with the characteristic) in this study was equal to 0.0105. The Z value for calculating sample size was 1.96.
Topical diltiazem (gel at 2%) was administered to group A in the immediate postoperative period (when the anesthetic effect ended) and treatment was continued for 72h, administering the medication in the same manner 3 times a day. Placebo was administered to group B with the same indications used in group A.
Both the diltiazem gel at 2% and the placebo had the same physical characteristics and they were presented to the patients in a dosing syringe. They were instructed to apply 0.5ml of the product in the anal region, the equivalent of 10mg per dose. Because the analysis was a double-blind study, neither the patient nor the researcher knew which syringes contained diltiazem or placebo.
The syringes were marked with progressive numbers and randomly assigned to each patient, with no knowledge of the contents. An independent assistant made a list identifying the syringes that contained diltiazem and those that contained placebo, and did not reveal that information to anyone. The list was kept in a closed envelope until the end of the study.
Both groups received the standard treatment for pain control in the postoperative period of the hemorrhoidectomy during the time of the study: sitz baths in warm water every 6h and 10mg of oral ketorolac every 6h in the event of pain.
The results were evaluated through the visual analog scale (VAS) on a straight line from 0 to 10 by the patients themselves for quantifying pain intensity. Pain was measured at 24, 48, and 72h.
Rescue therapy for pain in the postoperative closed hemorrhoidectomy period was registered by writing down the doses of ketorolac required by the patients at 24, 48, and 72h.
This study was approved by the Ethics Committee and the Research and Teaching Administration of the Hospital Juárez de México number HJM2146/12-A and was carried out at the Hospital Juárez de México and the Postgraduate Studies and Research Section of the School of Medicine of the Instituto Politécnico Nacional.
Statistical analysis: The Mann-Whitney U test was used to determine whether there were differences in age and sex between the two groups. The postoperative patient VAS values and number of analgesic doses were analyzed by the variance analysis test (ANOVA). Figure 1 shows the flowchart of the study.
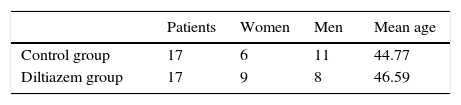
ResultsNineteen of the study patients were men and 15 were women. Their mean age was 45.67 years with a range of 28 to 74 years.
The mean age of the patients in the control group was 44.77 years and it was 46.59 years in the diltiazem group. There was no statistically significant difference in age between the two groups p=0.657, with a 95% confidence interval (CI). In the control group, 6 patients were women and 11 were men, and in the diltiazem group 9 patients were women and 8 were men. There was no statistically significant difference in relation to sex between the two groups p=0.317, with a 95% CI (Mann-Whitney U test) (Table 1).
The mean VAS value in the control group was 6.82±1.9cm at 24h, 5.3±1.66cm at 48h, and 4.32±2.13cm at 72h, and it was 2.97±1.18cm at 24h, 1.51±1.18cm at 48h, and 0.84±0.92cm at 72h in the diltiazem group (Table 2).
The statistical analysis for the VAS values between the two groups was carried out with the ANOVA test, finding a p < 0.001 with a 95% CI (fig. 2).
The mean number of analgesic doses used in the control group was 3.82±0.52 doses at 24h, 3.64±0.70 doses at 48h, and 2.88±1.26 at 72h, and it was 2.41±0.87 at 24h, 1.11±0.85 at 48h, and 0.94±0.96 at 72h in the diltiazem group (Table 3). The ANOVA test was also used in the statistical analysis for comparing the number of doses between the 2 groups, finding a p < 0.001 with a 95% CI (fig. 3).
No adverse reactions were observed in any of the patients in the control group or the diltiazem group during the time of the study.
Given that the sample included older adult patients, to prevent toxicity secondary to the use of ketorolac as rescue therapy, the study was not extended for a longer period of time.
DiscussionClosed hemorrhoidectomy with the Ferguson technique continues to be the best treatment for hemorrhoidal disease, with a low recurrence rate and a greater patient satisfaction rate in relation to results.6 Postoperative pain following hemorrhoidectomy is considered one of the 25 main causes of postoperative pain.7
Topical nitroglycerine has been shown to reduce pain in the postoperative period of patients that underwent hemorrhoidectomy. However, it is associated with a greater incidence of side effects, the most bothersome of which is headache. Wasvary et al.8 conducted a randomized study on 39 patients divided into 2 groups for evaluating the efficacy of topical nitroglycerine at 0.2% in the control of postoperative pain after hemorrhoidectomy. Topical nitroglycerine was administered to a group of 19 patients and placebo was given to the control group of 20 patients. The authors found that topical nitroglycerine at 0.2% reduced the analgesic doses with statistical significance on the second postoperative day. However, 8 of the 19 patients treated with topical nitroglycerine presented with headache, resulting in greater morbidity in this group, compared with the control group (p < 0.05). In a more recent study by Karanlik et al.,9 2 groups of 30 patients each were evaluated. One group used topical nitroglycerine at 0.2% and the other placebo. There were significant differences in the reduction of postoperative pain following hemorrhoidectomy on the first, third, and seventh postoperative days (p < 0.05). The authors also found a statistically significant lower cicatrization time in the nitroglycerine group than in the control group. In a meta-analysis carried out by Ratnasingham et al.10 that included a total of 5 clinical trials with a total of 333 patients, they compared topical nitroglycerine against placebo for postoperative pain reduction after hemorrhoidectomy. The results were statistically significant on postoperative days 3 and 7 (p of 0.029 and 0.014, respectively). Nevertheless, there were no significant differences on the first postoperative day. This meta-analysis also showed that cicatrization time was reduced in patients that used nitroglycerine, with an odds ratio of 3.57 (p < 0.0001) at 3 weeks. No adverse reactions, such as headache, anal pruritus, or perianal cutaneous irritation, were observed in our patients.
On the other hand, botulinum toxin, which also produces anal sphincter relaxation, could be a useful alternative in postoperative pain reductions in patients undergoing hemorrhoidectomy. In a randomized, double-blind study by Davies et al.,11 50 patients were divided into 2 groups of patients having undergone hemorrhoidectomy with the Milligan and Morgan technique. Twenty IU of botulinum toxin diluted in 0.4ml of saline solution were administered to one group of patients and only saline solution was injected into the internal anal sphincter of the control group patients. The authors found significant differences in relation to pain reduction on day 6 (p < 0.05) and day 7 (p < 0.05). In another study by Patti et al.,12 the efficacy of botulinum toxin was compared with that of topical nitroglycerine for reducing postoperative pain in patients that underwent hemorrhoidectomy. Thirty patients were divided into 2 groups of 15 patients each. Twenty IU of intrasphincteric botulinum toxin was administered to one group and 300mg of nitroglycerine at 2% was administered to the other group 3 times a day for 30 days. The authors found significant differences in relation to pain reduction in repose in the group treated with botulinum toxin. There were no differences in regard to pain during bowel movements or in cicatrization time. Headache presented as a side effect only in the group treated with nitroglycerine. Despite the good results published, botulinum toxin use is an invasive and a more expensive procedure. In our patients, the use of topical diltiazem at 2% was not an invasive procedure.
Carapeti et al.13 showed that topical diltiazem reduced the maximum resting pressure of the internal anal sphincter in volunteer healthy subjects, reaching a greater effect at a 2% concentration. The calcium blockers administered orally reduced anal pressure, but the required dose (60mg) was approximately 7 to 8 times higher than the required dose when applied topically (8 to 10mg). This means that topical treatment has a lower probability of causing systemic side effects.14
Silverman et al.15 carried out a randomized, prospective, double-blind study on 18 patients that underwent hemorrhoidectomy, dividing the patients into 2 groups of 9 patients each. Topical diltiazem at 2% in unguent form was used in one group and placebo in the other group. The results showed statistically significant reduced postoperative pain (p < 0.001) during the first 7 postoperative days. A more detailed analysis of their results showed that this effect was reached from days 1 and 2 with VAS values of 5.2±2.4 for the diltiazem group and 8.8±1.2 for the control group (p < 0.001). In addition, this effect was maintained for the rest of the study. For days 3, 4, and 5, the group treated with diltiazem had a VAS value of 3.7±2 and the control group had a value of 6.8±2. For days 6 and 7, the values in the group treated with diltiazem were 2.3±1.2 and for the control group were 5.2±1.7 (p < 0.001). Some of our study results coincided with those reported by Silverman et al. We found a statistically significant reduction in postoperative pain after hemorrhoidectomy from the first day in the group treated with topical diltiazem at 2%, with a mean VAS value of 2.97±1.2 and a value of 6.82±1.95 for the control group (p < 0.001, 95% CI). Likewise we observed that this effect was maintained for the 3 days of the study with mean VAS values on days 2 and 3 of 1.51±1.16 and 0.84±0.87, respectively, in the group treated with diltiazem, and of 5.3±1.68 and 4.32±2.17, respectively, in the control group (p < 0.001, 95% CI). Silverman5 found no significant differences in the use of analgesics in the postoperative period between the group treated with diltiazem compared with the control group. In contrast, we found significant differences in our study in the use of analgesics between the group treated with topical diltiazem and the control group (p < 0.001, 95% CI).
In a more recent randomized and prospective study by Chauhan et al.16 on postoperative hemorrhoidectomy patients, they compared internal lateral sphincterotomy with topical diltiazem at 2% for the control of postoperative pain. They studied 102 patients divided into 2 groups of 50 and 52 patients. The results showed a significantly lower VAS value in patients that underwent internal lateral sphincterotomy versus those that received topical diltiazem at 2% (2.23 vs 3.72; p=0.031). Likewise, the need for analgesics was lower in the group treated with sphincterotomy (10.54 vs 15.40; p=0.01). However, the incidence of complications was greater in the group treated with sphincterotomy (11.5% vs 3%; p=0.488). Despite the conclusion of the authors that lateral sphincterotomy provided greater postoperative pain reduction than diltiazem, a higher number of complications could be a limiting factor for using sphincterotomy as a measure for post-hemorrhoidectomy pain reduction.
ConclusionsThe groups analyzed in this study were comparable in relation to age and sex. There were significant differences with respect to the VAS values and the number of analgesic doses between the two groups, p < 0.001 with a 95% CI (utilizing the ANOVA test for the statistical analysis).
In our study, the application of topical diltiazem at 2% reduced postoperative pain in patients that underwent closed hemorrhoidectomy, compared with those that were given placebo. The results were clinically and statistically significant.
Ethical responsibilitiesProtection of persons and animalsThe authors declare that the procedures followed conformed to the ethical standards of the responsible committee on human experimentation and were in accordance with the World Medical Association and the Declaration of Helsinki.
Data confidentialityThe authors declare that they have followed the protocols of their work center in relation to the publication of patient data.
Right to privacy and informed consentThe authors declare that no patient data appear in this article.
Financial disclosureNo financial support was received in relation to this study.
Conflict of interestThe authors declare that there is no conflict of interest.
Please cite this article as: Rodríguez-Wong U, Ocharán-Hernández ME, Toscano-Garibay J. Diltiazem tópico en el dolor postoperatorio de hemorroidectomía con técnica cerrada. Revista de Gastroenterología de México. 2016;82:74–79.