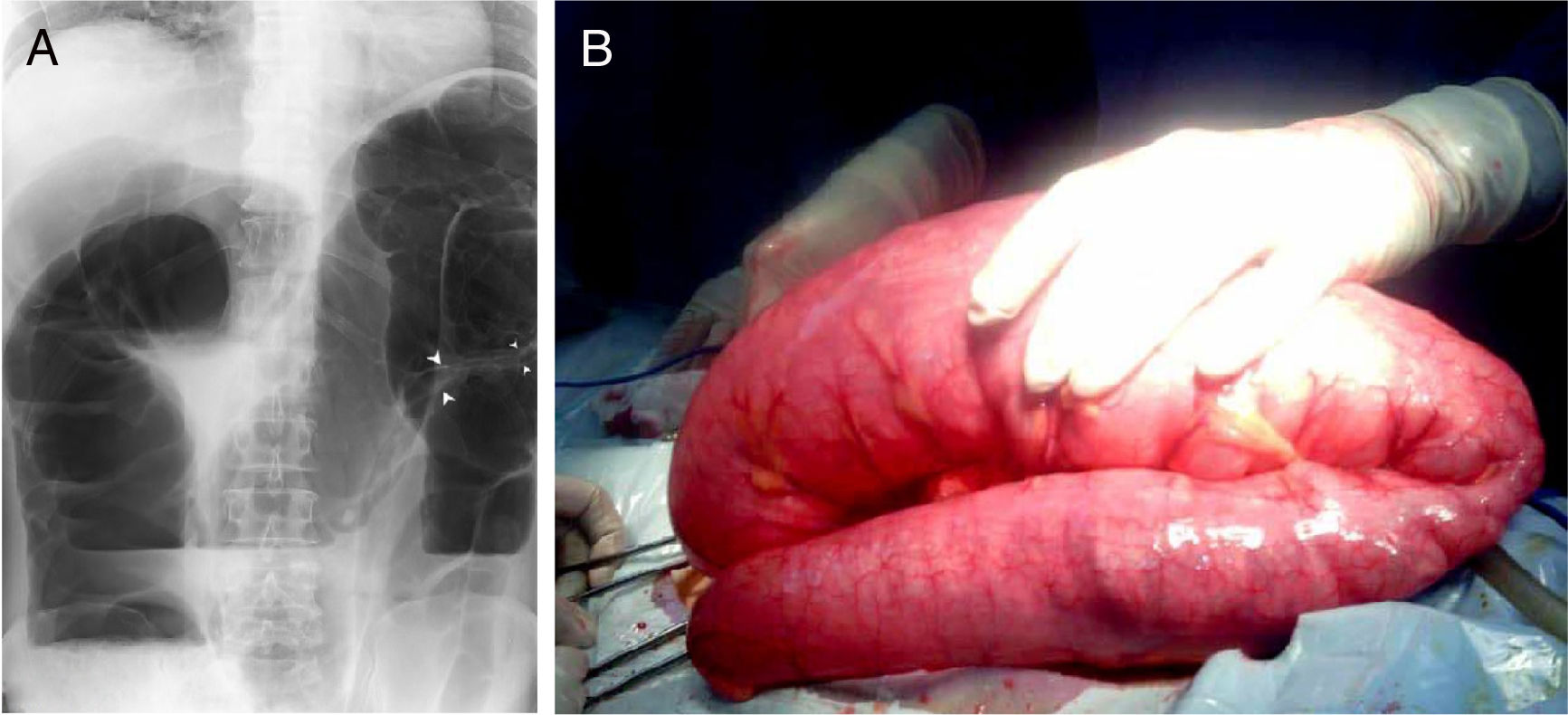
A 67-year-old man with a past medical history of irritable bowel syndrome, sought medical attention on 17/06/2018, due to the sudden onset 2 days prior of colicky, moderate-to-strong abdominal pain located in the left iliac fossa that radiated to the hypogastrium, with no respite. He presented with concomitant nausea, 9 episodes of vomiting of the upper intestinal content, and absence of defecation since the beginning of symptomatology. Upon physical examination, the patient was hemodynamically stable, and his general condition was regular. He was dehydrated, with skin and mucous membrane pallor, and a capillary refill time of > 3 s, diaphoresis, and eupnea. He also presented with abdominal distension, predominantly left asymmetry, diminished bowel sounds, tympanitic sound upon percussion, which was painful, and signs of peritoneal irritation. Laboratory test results: leukocytosis of 19,000mm3, with a left shift. Abdominal x-ray was suggestive of sigmoid volvulus (fig. 1A). The digestive tract decompressed with the placement of a nasogastric tube and the fluid and electrolyte balance was restored. The patient was then operated on, resulting in the following findings: a) approximately 100 cc of free fluid in the peritoneal cavity, b) sigmoid volvulus of 360° (fig. 1B), conditioned by multiple air-containing lesions on the wall (fig. 2A), not ruling out GIST, affecting 20cm of the sigmoid colon, c) distension of the entire colon, diameter > 15cm, d) redundant sigmoid colon measuring one meter in length, e) greatly distended segment of the terminal ileum (probable incompetent ileocecal valve), and f) undamaged remaining intra-abdominal organs. Exploratory laparotomy was performed, carrying out partial sigmoidectomy, resection, and end-to-end anastomosis of the sigmoid colon due to the sigmoid volvulus.
A Abdominal x-ray taken in the standing position suggestive of sigmoid volvulus. The image also shows a double-contour in the wall in the twisted segment of the colon (arrows), a grossly distended colon, and air-fluid levels. B) Sigmoid colon volvulus of 360° of an approximately 90cm segment, conditioned by multiple lesions on the wall of the sigmoid colon.
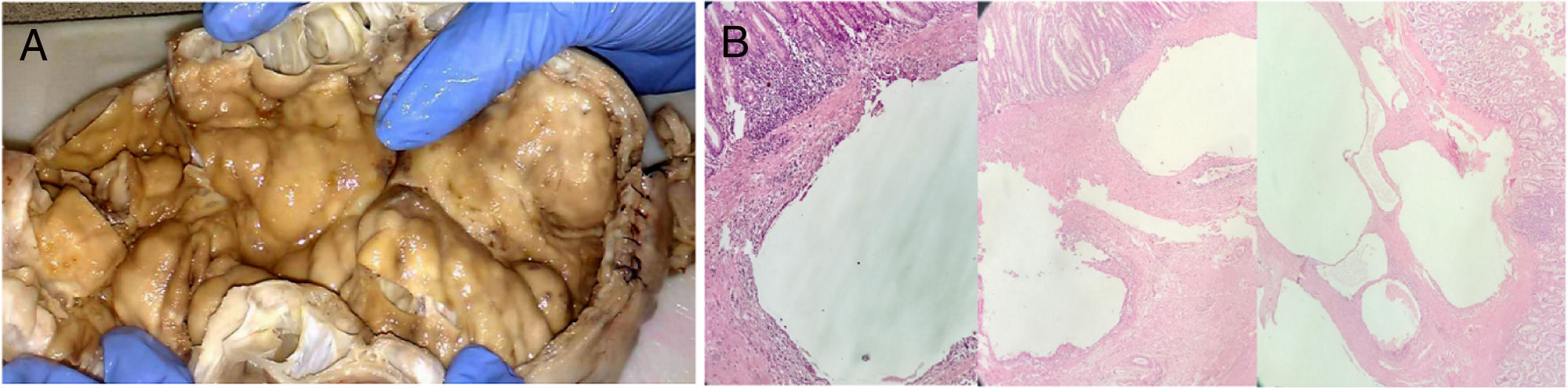
A) Photograph of the bowel segment, showing the 22cm x 8cm diameter of the sigmoid colon with multiple air-filled cystic lesions on the colonic wall. B) Photomicrography showing the histologic aspect of the bowel wall: cystic spaces located predominantly in the submucosa, internally lined with macrophages, lymphocytes, plasma cells, abundant multinucleated cells, and areas of fibrosis (hematoxylin & eosin staining).
The patient had torpid postoperative progression, with ileus that delayed the commencement of oral diet. He tolerated liquids and solids on postoperative day 6 and was released from the hospital with unobstructed bowel transit and satisfactory general health. At present, the patient's general condition continues to be good and he returned to work 40 days after surgery.
The anatomopathologic study reported a thick bowel segment with a yellow superficial surface covered with adipose tissue and signs of false diverticula. Slicing revealed multiple intramural cystic formations with a serous-like fluid content (fig. 2A), and bowel wall fragments with numerous cavities in the submucosa with scant inflammatory content. False diverticula with a mixed inflammatory infiltrate were identified. Consistent findings: 1) pneumatosis cystoides intestinalis (PCI) in the sigmoid colon and 2) diverticulosis with signs of diverticulitis (fig. 2B).
PCI was first described at necropsy in 1783 by Du Vernoi,1 and its present name was coined by Mayer in 1835.2 It is defined as the presence of multiple cysts with gas, located in the subserosa or submucosa. It is rarely located in the tunica muscularis of the gastrointestinal tract.3 The most frequent location is the small bowel, reported at 42%, followed by the large bowel, at 36%. Mixed location is described in 2% of cases.4,5
There are 2 known variants, and the secondary type accounts for 85% of the cases associated with COPD or immunosuppression. Other associated pathologies are inflammatory, obstructive, or infectious bowel disorders. Primary pneumatosis is not associated with other lesions, and it occurs in 15% of cases.3
From the epidemiologic perspective, it affects children and adults, as well as males and females. There is controversy as to the male:female ratio, which ranges from 3:1 to 5:1.6,7 The disease presents from the 2nd to the 7th decade of life, at a mean patient age of 56 years. Symptoms are complication-related and 3% of patients present with complications associated with obstruction, volvulus, invagination, and bowel perforation.8
The majority of cases respond satisfactorily to conservative treatment with antibiotic therapy, parenteral nutrition, and hyperbaric oxygen therapy.2 Surgery is performed when there are complications.9 The present case was consistent with secondary PCI. It was related to the patient's pathologic history, the lesions were at the second most frequent location, and the disease presented as a complication in the form of obstructive volvulus of the intestine.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that the procedures followed were in accordance with the regulations of the ethics committee on responsible human experimentation and with the World Medical Association and the Declaration of Helsinki.
Confidentiality of dataThe authors declare that they have treated all patient data with confidentiality and anonymity, following the protocols of their work center.
Right to privacy and informed consentThe authors have followed the protocols of their work center in relation to the publication of patient data, preserving patient confidentiality and anonymity.
Financial disclosureNo financial support was received in relation to this study/article.
Conflict of interestThe authors declare that there is no conflict of interest.
Please cite this article as: González-Rodríguez IC, Morales-Uribe JA, Colmenares-Chacón ML. Neumatosis quística intestinal secundaria complicada con vólvulo intestinal, revisión de la literatura a propósito de un caso. Revista de Gastroenterología de México. 2019;84:416–418.