A pulse granuloma, or vegetable granuloma, corresponds to a granulomatous inflammatory response secondary to particles of food or vegetable material, with characteristic hyaline rings and multinucleated giant cells. Described in the lung in 1969, its most common site of involvement is the oral cavity (typically in the mandible of edentulous patients with dental prostheses, in the walls of odontogenic cysts, in dental caries, open dental alveoli, and in teeth with previous endodontic treatment). Its presentation in the abdominal cavity is very rare1–3.
A 48-year-old woman with an unremarkable past medical history had vague abdominal pain of 6-month progression. Upon evaluation, systemic arterial hypertension and anemia were identified. She presented with elevated serum dopamine levels (936 pg/ml), for which pheochromocytoma was suspected (serum adrenaline and noradrenaline levels were within normal ranges). Magnetic resonance imaging was carried out that reported a “left heterogeneous oval-shaped adrenal gland tumor, probably a myelolipoma, displacing the ipsilateral kidney”. An exploratory laparotomy was performed, identifying “a mass in the region of the left adrenal gland, firmly attached to the diaphragm and upper pole of the left kidney, with multiple peritoneal adhesions”. A malignant infiltrating tumor was suspected, and adrenalectomy and nephrectomy were performed.
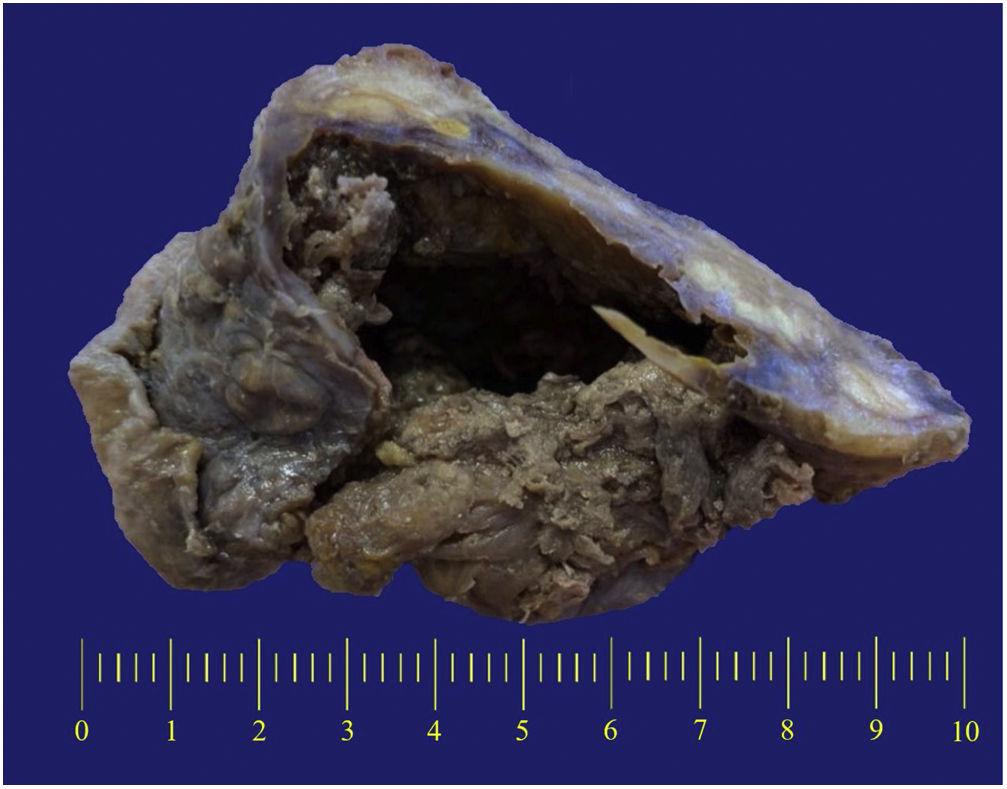
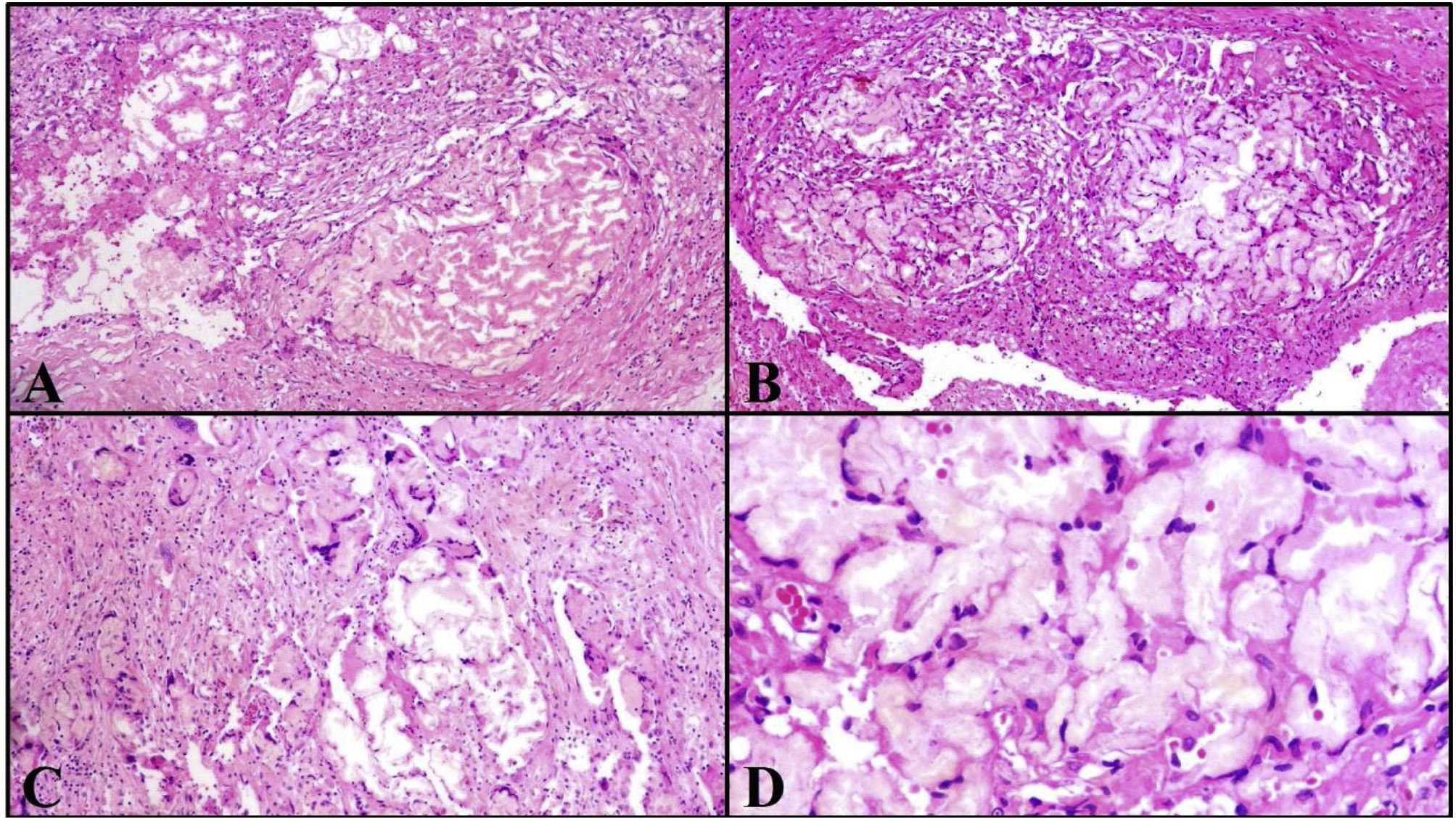
Macroscopically, the lesion had an irregular surface and borders, measured 10.0 × 8.0 × 6.0 cm, was heterogeneous, and had alternating dark brown congestive-appearing areas and yellowish-white areas. When cut, an area with central cavitation and an irregularly thick wall were revealed (Fig. 1). Microscopically, the lesion was composed of vegetable material associated with an intense xanthogranulomatous inflammatory reaction, which almost completely replaced the adrenal tissue, and was made up of multinucleated foreign body giant cells associated with acellular extracellular material that formed irregular acellular and eosinophilic rings, characteristic of pulse granuloma (Fig. 2). The inflammatory lesion bordered on the renal capsule, without affecting the parenchyma of the kidney.
(A–B) At medium magnification, the irregular accumulation of hyaline material surrounded by connective tissue and inflammatory cells can be seen (hematoxylin and eosin ×100). (C) Granulomatous inflammation with foreign body giant cells is identified in other areas (hematoxylin and eosin ×100). (D) At a higher magnification, the hyaline material can be seen to form acellular and eosinophilic ring-like structures (hematoxylin and eosin ×400).
The patient is asymptomatic at three years from the surgery.
The clinical presentation of pulse granuloma is variable, predominating in the oral cavity and lungs, in middle-aged men (a mean of 34.4 years)1, and ranges from asymptomatic nodules to lesions that mimic malignant infiltrating tumors, as occurred in our patient. Its presentation apparently depends on the antigenic potential of the vegetable material that initiates the inflammatory response2.
Its etiology has been discussed over the years. The presence of hyaline rings has been proposed to be secondary to a vascular degeneration process or granulomas with a long period of evolution, with degenerative changes. However, the strongest evidence suggests that the hyaline rings arise from exogenous vegetable material1,3, and are secondary to the enzymatic degradation of the component of starch and the preservation of the component of cellulose, forming the rings, whose centers can be slightly variable, with an amorphous, fibrillar, or inflammatory cell matrix2,3.
Pulse granuloma outside of the oral cavity and lung is rare, with a small number of reports on its presence in the gastrointestinal tract and abdominal cavity4, rectum, fallopian tube and ovary, knee, intrahepatic portal vein5, abdominal lymph nodes, sigmoid mesocolon6, and pelvic region3.
Its presentation in the abdominal cavity is attributable to the entrance of vegetable content by way of its passage from the digestive tract lumen through continuity defects in the wall, such as perforated diverticula7, wall microabscesses, fistulous tracts, intestinal wall perforation4, perforated gastric ulcers, or Crohn’s disease6. Importantly, in some cases, the perforation site can be undefined and the patient asymptomatic. In our case, magnetic resonance imaging reported no alteration in the morphology of the digestive tract, ruling out diverticular disease, and identified no apparent signs of a perforation site.
Microscopically, pulse granuloma is characterized by the presence of acellular eosinophilic hyaline rings, associated with an inflammatory reaction typically composed of foreign body giant cells. Vegetable material immersed in the lesion can sometimes be identified, but not always. Even though there are characteristic findings, in some cases, vegetable material is limited, and giant cells are scarce. The differential diagnosis can be made by the presence of an amyloid deposit, which can be determined histochemically through Congo Red dye, which is negative in hyaline rings7.
The inflammatory reaction can mimic neoplasia. A reported case of pulse granuloma presented as a pelvic tumor with nodules in the peritoneal cavity, simulating carcinomatosis or peritoneal tuberculosis3. It can sometimes mimic neoplasia, such as colon cancer4, or as in our case, an adrenal gland tumor, a site that has not previously been reported in the literature. The correct diagnosis was made after the histopathologic analysis was carried out.
In conclusion, knowledge of this entity and the fact that it can present outside of the oral cavity are important. Pulse granuloma can mimic neoplastic processes, causing patients to undergo unnecessary medical or surgical procedures.
Ethical considerationsThe present work meets the current bioethical research norms. Because it was an observational study that involved no diagnostic or therapeutic interventions on the patient, approval by an ethics committee was not required. The authors declare that this article contains no personal data in the text or its annexes that could identify the patient.
Financial disclosureNo specific grants were received from public sector agencies, the business sector, or non-profit organizations in relation to this scientific letter.
Conflict of interestThe authors declare that there is no conflict of interest.
Please cite this article as: Teco-Cortes JA, Santos-Torres SB, Aristi-Urista GB. Granuloma vegetal en cavidad abdominal simulando un tumor en glándula suprarrenal. Rev Gastroenterol Méx. 2023;88:181–183.