Achalasia is a primary motor disorder of the esophagus characterized by an increase in the relaxation pressure of the lower esophageal sphincter (LES) and esophageal aperistalsis.1 Its incidence is 1/100,000/year.2 The symptoms include dysphagia, weight loss, regurgitation, and chest pain, resulting in a negative impact on quality of life.2 The cause is unknown, but there is an autoimmune component at the level of the myenteric plexus.2,3
Diagnosis is manometric and high resolution manometry (HRM) subclassifies the disease into 3 types:4 type I (classic), type II (pressurized), and type III (spastic). Management is focused on reducing the LES pressure, for which there are 3 types of treatment: medical, endoscopic, and surgical.5 The latter is the gold standard and consists of a laparoscopic Heller myotomy (LHM) with a partial fundoplication; its efficacy is 86% and it remains up to 70% at 5 years.6 The first peroral endoscopic myotomy (POEM) carried out on humans was reported in 2010.7 This technique consists of the performance of an endoscopic myotomy of the circular layer of the esophagus and LES, utilizing a submucosal tunnel with an opening at the entrance of the proximal esophagus.8 Its preliminary results have been similar to those of the LHM, with the advantages of being less invasive, less expensive, and with fewer days of hospital stay.9 Our objective was to report the experience of implementing POEM in a Mexican patient presenting with achalasia.
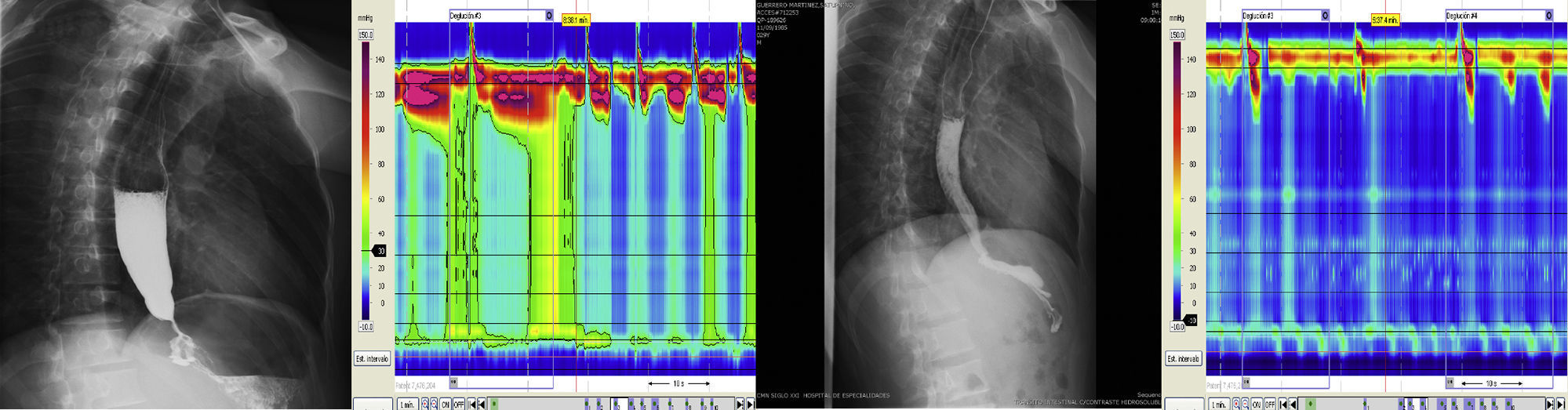
A 29-year-old man had dysphagia of one-year progression, together with regurgitation, chest pain, and weight loss of 20kg. The esophagogastroduodenal series (EGDS) showed a dilated esophagus. Endoscopy and tomography ruled out other lesions. HRM confirmed type II achalasia. The Eckardt score determines the grade of dysphagia through a point system in which a higher number represents a more serious disease. It uses 4 variables and each one has a maximum value of 3. Success is defined as an index ≤ 3 points. Our patient had a score of 12.10 Before the procedure was performed, it was approved by the hospital ethics committee and the patient signed a statement of informed consent.
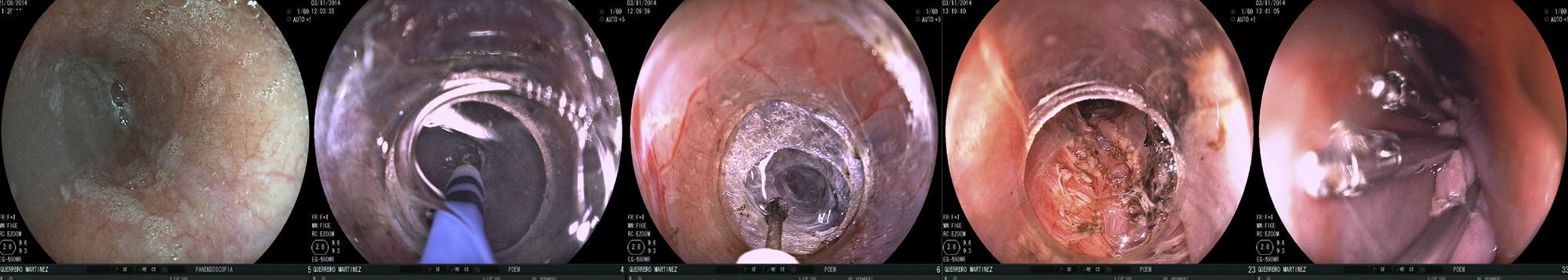
The patient was admitted to the hospital 2 days prior to the POEM. He was first given 1g of cefotaxime IV every 12h, a liquid diet, and then fasted for 12h before the procedure. We used a model EG590WR endoscope (Fujinon, Tokyo, Japan), a model DH-28GR hood (Fujinon, Tokyo Japan), and ERBE VIO Model 200D equipment with a hybrid knife (Tübingen, Germany). The following 3 effects were employed: elevation (ERBEJET effect 2 at 30 w), incision (ENDOCUT Q effect 3, cut duration 3 and an interval of 3), tunnelization (SWIFT COAG effect 3 at 70 w), myotomy (effect 4 at 60 w), and for hemostasis (FORCED COAG effect 2 at 50 w). Closure was performed with 10 hemoclips (Boston Scientific, USA). The 5 steps of POEM were carried out:
- 1.
Revision and injection: the level of the gastroesophageal junction (GEJ) was registered and a combination of injectable water and carmine indigo at 0.5% was injected 15cm proximal to that point.
- 2.
Incision: a 2cm longitudinal incision was made with the hybrid knife at that point.
- 3.
Tunnelization: the submucosa was dissected from the entrance site up to 2cm under the GEJ.
- 4.
Myotomy: the circular muscle of the esophagus was dissected 2cm under the entrance site and continued up to 2cm under the GEJ.
- 5.
Closure: 10 hemoclips were placed at the entrance site. Total procedure duration was 110min. There was mild bleeding during tunnelization and myotomy that was controlled endoscopically (figure 1).
There were no posterior complications. The EGDS at 24h showed no perforation data. The HRM at 48h revealed a reduction in the residual pressure of the LES (48mmHg pre-POEM vs 18mmHg post-POEM) and pressurization loss (figure 2). Liquid diet was begun at 36h and normal diet at 48h. The patient was released on the third day with no complications. At the follow-up at 1 month, the patient had an Eckardt score of 4.
This case demonstrates the safety and efficacy of POEM in a Mexican patient with achalasia, objectively confirmed by EGDS, HRM, and the Eckardt scale pre and post-POEM. Hospital stay was only 5 days and the patient had a rapid return to normal daily activities. The clinical effects of the POEM were immediate and the later HRM showed improvement in the LES pressure and pressurization disappeared. We believe the short-term results of this technique are safe and effective, in addition to the functional and esthetic advantages for the patient. Nevertheless, it should only be performed in centers with adequate experience and satisfactory cardiothoracic surgery service support, in the event that there is some type of complication. The mid and long-term results in these patients remain to be seen in order to determine the actual role of POEM in the treatment of achalasia.
Financial disclosureNo financial support was received in relation to this study.
Conflict of interestThe authors declare that there is no conflict of interest.
Please cite this article as: Hernández-Mondragón OV, González-Martínez MA, Blancas-Valencia JM, Altamirano-Castañeda ML, Muñoz-Bautista A. Miotomía peroral endoscópica en acalasia. Reporte del primer caso realizado en México. Revista de Gastroenterología de México. 2015;80:165–166.