We present herein the case of a 17-year-old female diagnosed with stage IV extranodal natural killer (NK)/T-cell lymphoma, nasal type, with extensive craniofacial involvement documented by computed axial tomography (CAT). After receiving the first chemotherapy regimen, she developed multiple organ failure and had a prolonged hospital stay. Due to the presence of odynophagia and intolerance to oral intake, the placement of a percutaneous endoscopic gastrostomy for feeding was ordered.
The procedure was performed with the patient under sedation in the dorsal decubitus position. During the endoscopy, an infiltrative lesion was observed on the paladar that communicated with the nasopharynx. No other alteration was observed in the rest of the study. After adequate endoscopic transillumination and digital pressure, the puncture site in the abdominal wall was located. During the procedure, the patient presented with dyspnea and so her position was modified, inclining the bed to 80°, and the procedure was completed, utilizing the pull-through technique, with no immediate complications.
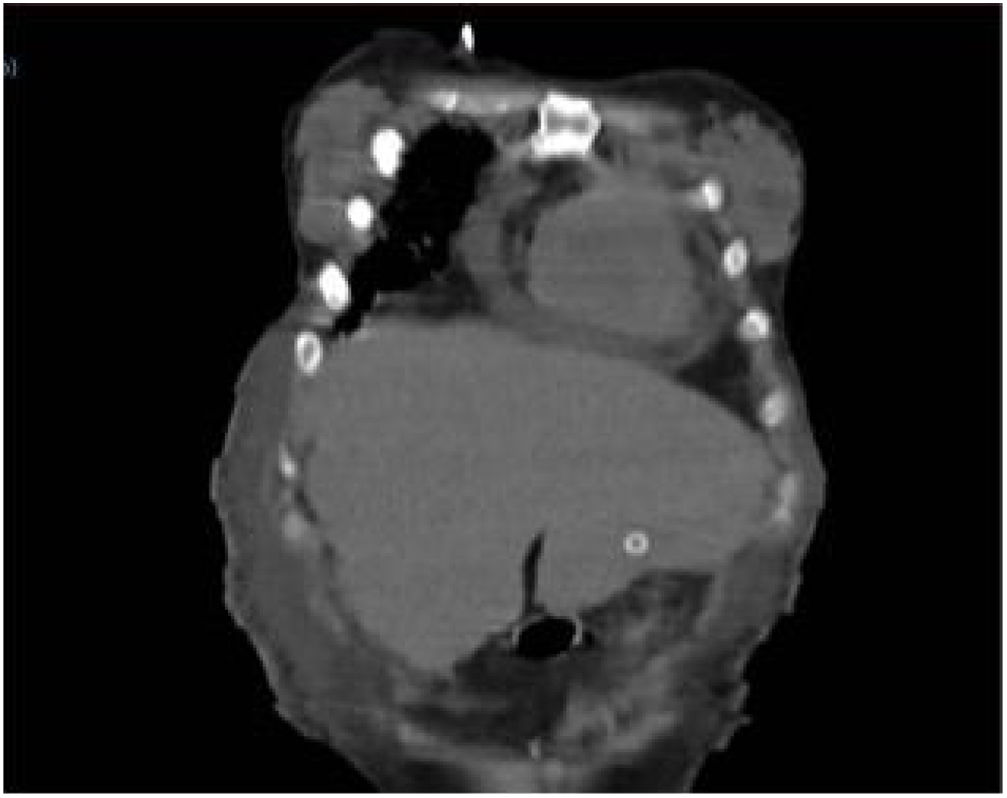
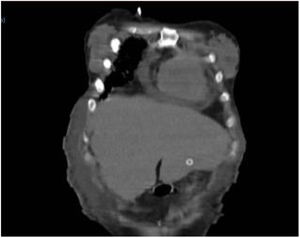
Eight hours after the procedure, nutrition was administered, with no flow or leak complications. Upon examination, the patient presented with intense abdominal pain, with no systemic inflammatory response or signs of peritoneal irritation. Laboratory test results showed no decrease in hemoglobin or leukocytosis, only the already known thrombocytopenia (88,000 platelets). Due to symptom persistence, an abdominal CAT scan was ordered, showing the tube passing through the liver (segment III) and the internal bumper in place within the stomach. There were no signs of bleeding or perforation (Figs. 1 and 2).
Because of the risk for bleeding and the prognosis of the underlying disease, the decision was made not to remove the tube. The patient remained stable and with no pain. One week later, an abdominal CAT scan, with contrast medium administered via the tube, showed no evidence of leaks, with adequate passage into the gastric chamber (Fig. 3).
Diet through the gastrostomy was begun. Tolerance was good and the patient was released to her home 3 days later with no complications.
Percutaneous endoscopic gastrostomy is the method of choice for establishing long-term enteral access in patients with preserved intestinal function that are unable to have oral feeding. In 1980, Gauderer et al. described its efficacy as an alternative to placement by laparotomy.1 Its technical success rate is currently above 95%. The most frequent indications are neurologic disorders, followed by tumors of the head and neck.2 Contraindications are coagulopathy, marked ascites, abdominal wall infection, bowel obstruction, carcinomatosis, gastric varices, or the interposition of an organ.3
Around 250,000 endoscopic gastrostomy tubes are placed every year in the United States.4 A complication rate of 16% is reported, of which 81% are considered minor.5 Major complications are significant bleeding, necrotizing fasciitis, buried bumper syndrome, tumor seeding, and adjacent organ injury.6
Incidental injury to the liver is extremely rare. In 2018, Chhaparia et al. reported a total of 7 cases described up to that year.7
In all the cases reported, the traction method was performed and there were no immediate complications. Diagnosis was made after post-procedure day 4, with a range of 4–75 days, in 85% of the cases.8–11
The pivotal datum in 42% of the cases was abdominal pain, 28% of patients were asymptomatic, 14% experienced tube dysfunction 60 days after placement, 14% presented with hypovolemic shock, and 14% had elevated transaminase levels, fever, and chills. Diagnosis was made through abdominal ultrasound in 42% of the cases, through CAT scanning in 42%, and through abdominal radiography, with contrast medium administration via the tube in 14%.8–11
Management was determined by the clinical progression of the patient. In 2 of the 3 cases that manifested only with abdominal pain, management was conservative, with no need to remove the tube and no sequelae related to its transhepatic passage. Exploratory laparotomy was performed in the remaining case, with tube removal and the placement of a new tube one week later. The same management was implemented in the case that presented with tube dysfunction 2 and a half months after placement. The patients with systemic inflammatory response or bleeding required surgical management.8,10,12
To the best of our knowledge, our patient is presently the eighth case reported in the literature. The elevation of the headboard to 80° after the transillumination of the abdominal wall was a likely predisposing factor. In that position, the edge of the liver shifted underneath the costal ridge, possibly contributing to the transhepatic placement of the tube. Therefore, we recommend avoiding that position. If changing the position of the patient during the procedure is necessary, the puncture site should be newly verified through digital pressure and transillumination. Given the heterogeneity of the cases described, it is not possible to standardize a diagnostic or treatment algorithm. We propose conservative management, as long as the condition of the patient allows it. A PEG tube can even be used, when it remains functional. If the patient continues to present with symptoms or with signs of hemodynamic instability or sepsis, the tube should be removed, preferably through a surgical approach, to control injury to the hepatic parenchyma. Its replacement, if needed, can be carried out at a later date.
Ethical disclosuresInformed consent was requested of the patient to receive treatment or participate in the present study. This article contains no personal information allowing the patient to be identified.
The present article complies with the current bioethics research regulations.
Financial disclosureNo type of financial support was received.
Conflict of interestNone of the authors has a conflict of interest regarding the publication of the present article.
Please cite this article as: Picazo-Ferrera K, Escobedo-Paredes DM, Herrera-Servín MA, Hernández-Guerrero AI, Ramírez-Solis ME. Colocación incidental transhepática de una sonda de gastrostomía endoscópica percutánea. Presentación de una complicación poco frecuente y revisión de la literatura. Revista de Gastroenterología de México. 2020;85:479–481.