Human obesity is associated with a proinflammatory state and an elevated level of mediators, such as C-reactive protein (CRP).
ObjectivesTo establish CRP levels as baseline preoperative values and then at 6 months after bariatric surgery, as well as to determine the changes in weight, body mass index (BMI), leukocytes, and glycemia.
Materials and methodsAn observational, analytical, retrospective, longitudinal, and open study was conducted. Serum CRP values were measured in 36 adults presenting with morbid obesity, and their baseline relation to weight, BMI, leukocytes, and glycemia was determined; the relation to the same parameters was established again, 6 months after bariatric surgery.
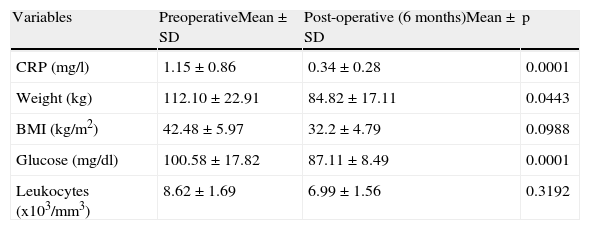
ResultsThe mean and standard deviation of preoperative and postoperative CRP (mg/L) was 1.15±0.86 and 0.34±0.28, respectively with p<0.0001; weight (kg) 112.10±22.91 and 84.82±17.11, p=0.0443; BMI (kg/m2) 42.48±5.97 and 32.2±4.79, p=0.0988; glucose (mg/dL) 100.58±17.82 and 87.11±8.49, p<0.0001, and leukocytes (× 103/mm3) 8.62±1.69 and 6.99±1.56, p=0.3192.
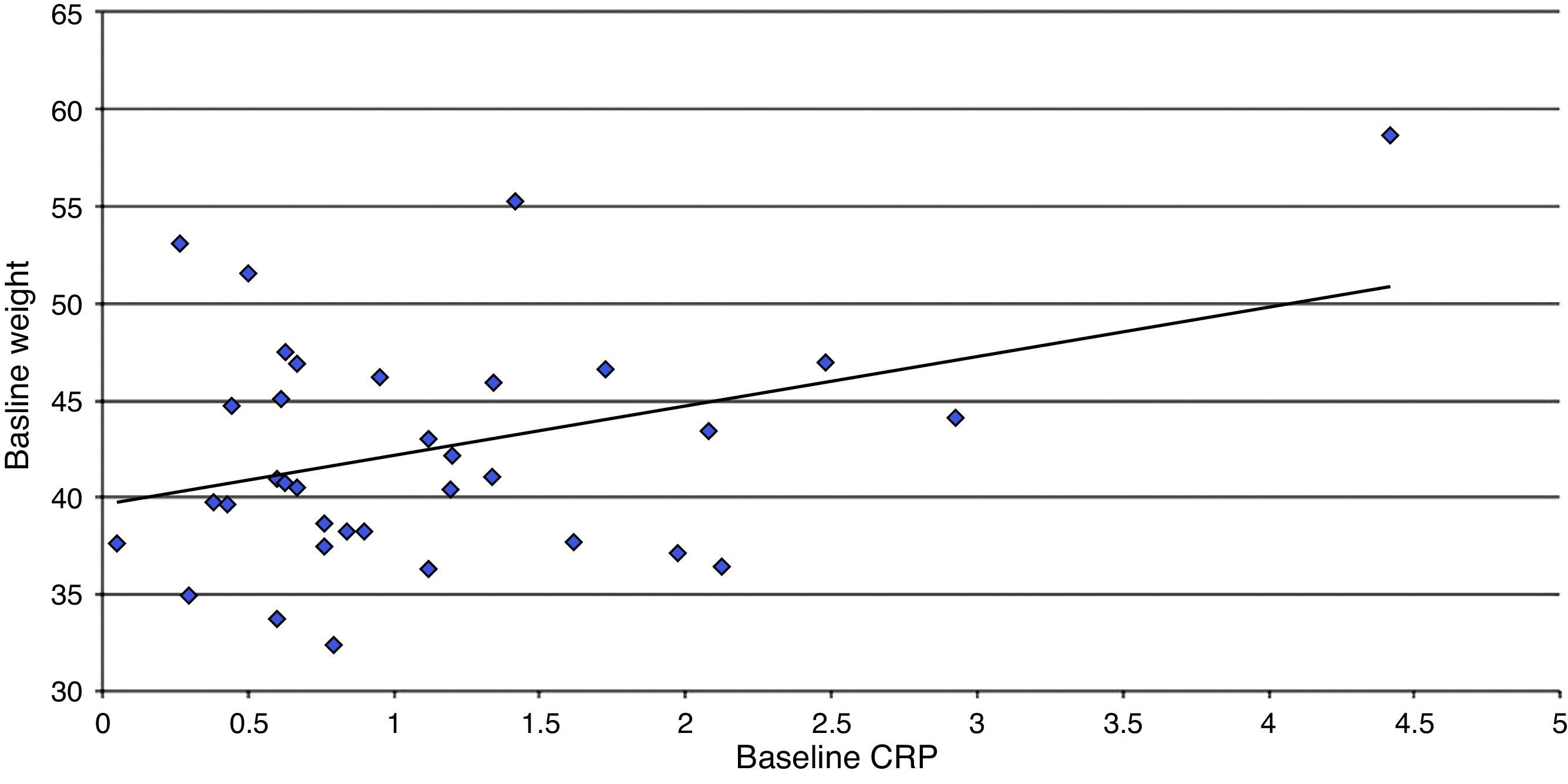
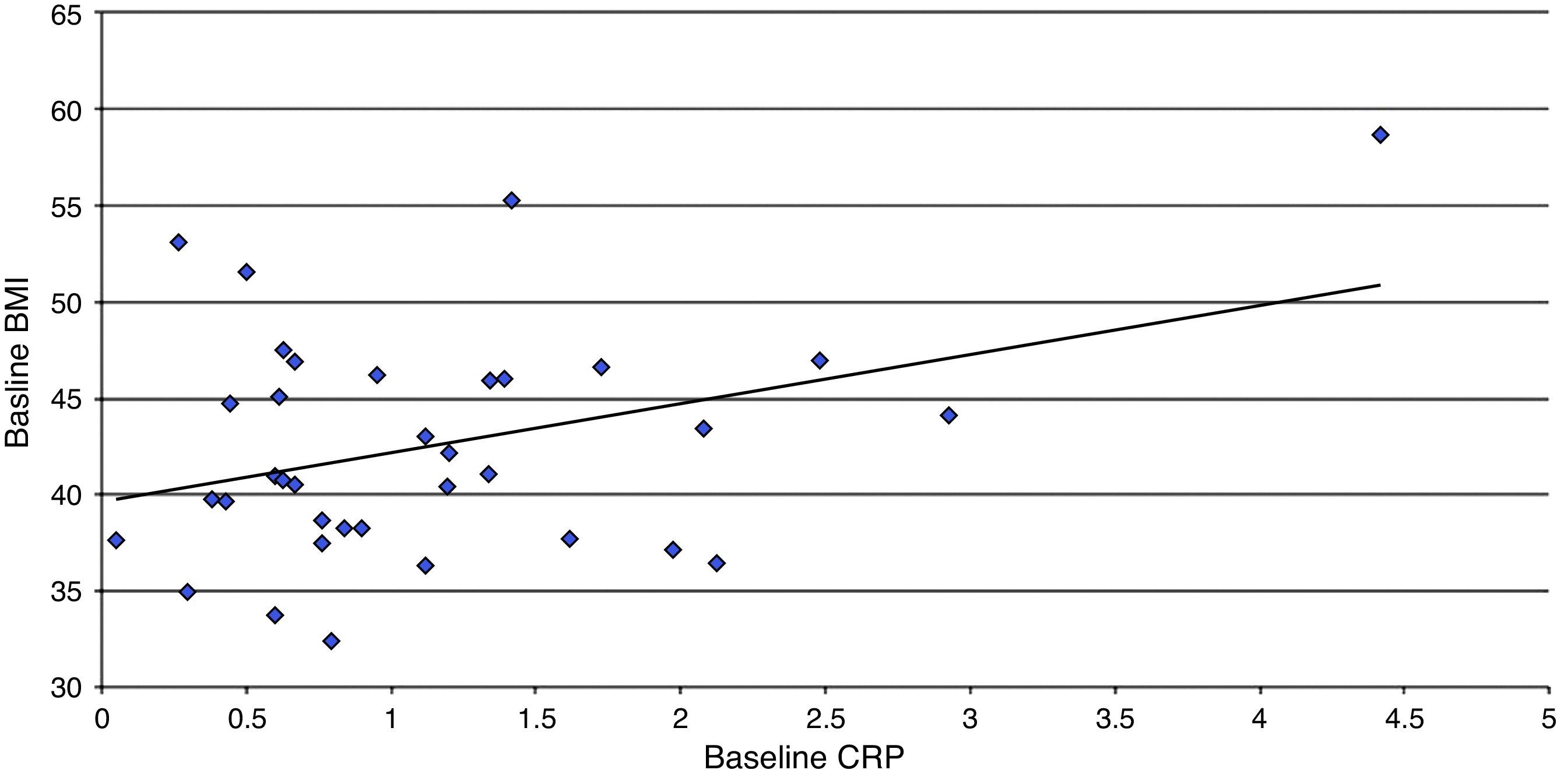
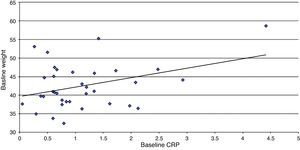
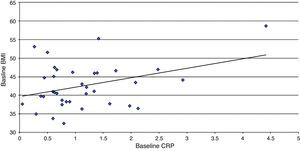
Baseline CRP only correlated with weight and BMI (p=0.047 and p=0.027 respectively) and there was no correlation between postoperative CRP and the evaluated parameters.
ConclusionsPreoperative CRP had a significant lineal relation to weight and body mass index. Patients who underwent bariatric surgery had a significant decrease in CRP, weight, and fasting glucose at 6 months after surgery.
La obesidad humana se asocia a un estado proinflamatorio reflejado en elevación de marcadores como la proteína C reactiva (PCR).
ObjetivosEstablecer los valores de PCR basales y a 6 meses de la cirugía bariátrica, así como los cambios en peso, índice de masa corporal (IMC), leucocitos y glucemia.
Materiales y métodosSe realizó un estudio observacional, analítico, retrospectivo, longitudinal y abierto. Se midieron los valores de PCR sérica y su relación con el peso, IMC, leucocitos y glucemia de manera basal y 6 meses posteriores a cirugía bariátrica en 36 adultos con obesidad mórbida.
ResultadosLa media ± desviación estándar de la PCR pre y posoperatorio (mg/l) fue 1.15±0.86 y 0.34±0.28, respectivamente, con p<0.0001; peso (kg) 112.10±22.91 y 84.82±17.11, p=0,0443; IMC (kg/m2) 42.48±5.97 y 32.2±4.79, p=0.0988; glucosa (mg/dl) 100.58±17.82 y 87.11±8.49, p<0.0001, y leucocitos (× 103/mm3) 8.62±1.69 y 6.99±1.56, p=0.3192.
La PCR basal solo correlacionó con el peso e IMC (p=0.047 y p=0.027, respectivamente) y no hubo correlación entre la PCR posoperatoria y ninguno de los parámetros evaluados.
ConclusionesLa PCR tiene una relación lineal significativa en el preoperatorio con el peso y el IMC. Los pacientes sometidos a cirugía bariátrica presentaron disminución significativa en la PCR, el peso y la glucemia en ayuno a los 6 meses posterior a la cirugía.
Obesity is currently a pandemia. It is estimated that in 20 years obesity and its related comorbidities will be the number one health problem worldwide. From 1960 to 2000 the prevalence of obesity more than doubled, augmenting from 13.3% to 30.9%. The prevalence of morbid obesity increased from 2.9% to 4.7% between the years 1988 and 2000.1 Many studies show that obese individuals have a 50 to 100% higher risk for death due to any cause, especially cardiovascular events, compared with normal weight individuals. There is a mean 2 to 5-year decrease in the life expectancy of a moderately obese person, and that decrease is 8 to 13 years for individuals with a body mass index (BMI) above 45.2
It is a known fact that the results of the medical treatment of obesity are not very encouraging.3 The United States National Health Institute found that 95% of the patients that begin with weight loss with or without modifying their habits, return to their usual weight 2 years from the time of their maximum weight loss. Because of this, two long-term weight control treatments are recommended: vertical banded gastroplasty or gastric cuff and Roux-en-Y gastric bypass.4
Human obesity is associated with a chronic low-grade proinflammatory state manifested by an increase in the plasma levels of the interleukin 6 (IL-6) and tumor necrosis factor alpha (TNFα) inflammatory cytokines, as well as elevated acute phase enzymes and high levels of endothelial cell dysfunction and activation markers. Weight loss attenuates this proinflammatory state.5
Likewise, obesity is associated with diminished longevity and increased morbidity due to a large number of illnesses such as type 2 diabetes mellitus (DM2), cardiovascular diseases, high blood pressure, and hyperlipidemia.6 The basis of the relation between obesity and the development of these diseases is not very clear. An increase in the circulating levels of inflammatory mediators has been demonstrated in obese individuals. These findings are interesting in the context of a pathophysiologic role suggested for the inflammatory mediators in the development of obesity-related morbidity, such as insulin resistance and cardiovascular diseases.7
Massive accumulation of body fat in morbid obesity has been associated with hyperinsulinemia and insulin resistance (IR), which appear to be the cornerstones of obesity-related metabolic syndrome. Obesity and IR are associated with high marker levels of circulating endothelial dysfunction, such as the intercellular adhesion molecule-1 (ICAM-1), soluble E selectin, and the von Willebrand factor, as well as endothelial vasoactive peptides, like angiotensinogen and the angiotensin-converting enzyme (ACE).8
In addition, there is evidence suggesting the role of low-grade inflammation as the association factor between obesity and IR, with endothelial dysfunction. An increase in the levels of serum inflammatory markers such as C-reactive protein (CRP) has been reported in obese subjects and it has been associated with the degree of IR and endothelial dysfunction. Numerous mechanisms for explaining the low-grade inflammation related to obesity have been suggested.8 First, fatty tissue is an important source of proinflammatory cytokines, such as TNFα and IL-6, and of anti-inflammatory cytokines, such as adiponectin. Second, IR can cause inflammation by interfering with the anti-inflammatory effect of insulin. And finally, obesity is characterized by oxidative stress, mainly through excessive ingestion of macronutrients or through an increase in the metabolic rate, which can be partially responsible for the inflammatory response. In fact, a glucose or lipid load in normal or obese subjects causes an increase in inflammation and a decrease in vascular reactivity.8 Controversially, dietary restriction in obese patients causes a significant reduction in oxidative stress and inflammation.9
Van Dielen et al. demonstrated a correlation between the levels of the inflammatory mediators, the acute phase proteins, and body weight. Even though a causal relation has not been found, it suggests that elevated levels of CRP are prognostic for the development of cardiovascular disease. Other proteins related to inflammation, such as the plasminogen activator inhibitor-1 and the macrophage migration inhibitory factor, are associated with the development of obesity-related diseases.10
It has been suggested that weight loss after bariatric surgery causes a reduction of metabolic stress, which in turn reduces the inflammatory markers and acute phase proteins in subjects presenting with morbid obesity. 11
During weight loss from restrictive gastric surgery, there is an eventual decrease in practically all the measured inflammatory mediators; and it has been shown that after that, obesity surgery significantly reduces the comorbidities related to obesity, such as cardiovascular disease and diabetes mellitus.12
CRP is a classic and highly sensitive acute phase protein whose plasma levels typically increase 100 times or more during inflammation. CRP is a strong predictor for cardiovascular risk and indirect evidence indicates that it can be directly related to atherosclerosis.13
Our hypothesis was that the patients that underwent bariatric surgery would present with significant CRP reduction 6 months after the procedure.
The principal aim of this study was to establish the baseline CRP values and then those at 6 months after bariatric surgery, as well as the changes in weight, body mass index (BMI), leukocytes, and glycemia. Another aim was to determine whether there was any correlation between CRP values and weight, BMI, leukocytes, and glycemia.
MethodsAn open, analytic, observational, longitudinal, and retrospective study was conducted. It included patients seen at the Hospital General Dr. Manuel Gea González that were diagnosed with morbid obesity. They underwent bariatric surgery within the time frame of January 2009 to January 2012. The inclusion criteria were patients diagnosed with morbid obesity with no comorbidities, surgically treated with gastric by-pass or sleeve gastrectomy and treated at the abovementioned hospital, and whose medical records included measurements of weight, glycemia, leukocytes, and CRP at the baseline and 6 months after surgery.
The baseline CRP, leukocyte, and glucose measurements were determined at 7:00h the day of the surgery, prior to the procedure, provided that the patients had agreed to enroll in the study and had signed statements of informed consent.
The SYNCHRON LX system was used for measuring CRP by a turbidimetric method. In the reaction, CRP is combined with a specific antibody to form insoluble antigen-antibody complexes. The system controls the change of absorbance at 340 nanometers, which is directly proportional to the CRP sample concentration and is used for calculating the concentration, based on a predetermined calibration curve and a single point.
Patients that had been operated on at a different hospital or that did not have the baseline and postoperative CRP measurements were excluded from the study. A sample size of 36 patients was calculated and a detected correlation coefficient of at least 0.4 was expected, with a 95% confidence interval and an 80% test potential (Epidat 4.0).
The case records of the study population were reviewed. A database was formed that included the sex and age of the patients, the type of surgery performed, patient weight, height, and BMI, white blood cells, and glycemia, along with the preoperative CRP and the postoperative CRP at 6 months after surgery. The difference between the baseline variables and those at 6 months was analyzed, as well as the correlation of CRP with weight, BMI, glycemia, and leukocytes. The existing linear correlation between CRP and weight, BMI, glucose, and leukocytes was determined using the Pearson correlation coefficient.
The statistical analysis was done with the Excel and StatCalc programs and means ± standard deviation were obtained. The differences between the baseline and postoperative values at 6 months were analyzed using the paired Student's t test. The Pearson correlation coefficient was employed to determine the correlation between the variables. Statistical significance was considered when p<0.05.
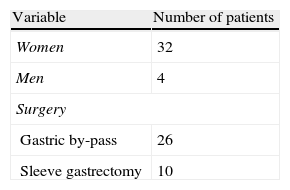
ResultsA total of 36 patients were included in the study. All the patients without comorbidities that underwent bariatric surgery within the time frame described accepted to participate in the study and their baseline CRP and postoperative CRP values at 6 months were measured. The preoperative variables are shown in Table 1.
Preoperative Variables (n=36).
| Variable | Number of patients |
| Women | 32 |
| Men | 4 |
| Surgery | |
| Gastric by-pass | 26 |
| Sleeve gastrectomy | 10 |
| Mean ± standard deviation | |
| Age (years) | 37±7.94 |
| CRP (mg/l) | 1.15±0.86 |
| Weight (kg) | 112.1±22.91 |
| Height (m) | 1.62±0.08 |
| BMI (kg/m2) | 42.48±5.97 |
| Glucose (mg/dl) | 100.58±17.82 |
| Leukocytes (x103/mm3) | 8.62±1.69 |
BMI: Body mass index; CRP: C-reactive protein.
The preoperative and postoperative values of the variables were compared, as shown in Table 2. There was a statistically significant decrease between the preoperative and the postoperative values of CRP, weight, and fasting glucose. The mean percentage of the CRP decrease between the preoperative value and that at 6 months after surgery was 65%. Despite the fact that there was a decrease in the BMI in relation to the preoperative and postoperative values (42.48 and 32.2, respectively), there was no statistical significance; with a larger sample size a p<0.05 probably would have been reached.
Comparison of preoperative and post-operative values (n=36).
| Variables | PreoperativeMean±SD | Post-operative (6 months)Mean±SD | p |
| CRP (mg/l) | 1.15±0.86 | 0.34±0.28 | 0.0001 |
| Weight (kg) | 112.10±22.91 | 84.82±17.11 | 0.0443 |
| BMI (kg/m2) | 42.48±5.97 | 32.2±4.79 | 0.0988 |
| Glucose (mg/dl) | 100.58±17.82 | 87.11±8.49 | 0.0001 |
| Leukocytes (x103/mm3) | 8.62±1.69 | 6.99±1.56 | 0.3192 |
SD: standard deviation; BMI: body mass index; CRP: C-reactive protein.
The preoperative CRP correlation coefficient with the variables analyzed was: weight r=0.33, p=0.047 (Fig. 1); BMI r=0.37, p=0.027 (Fig. 2); glucose r=0.30, p=0.071; and leukocytes r=0.03, p=0.22; the first 2 values were statistically significant. The CRP and postoperative variables did not show high correlation coefficients.
Six months after surgery there was a considerable decrease in CRP; the mean value was 0.34mg/l, which was within the normal range. The difference with respect to the baseline value was statistically significant. There were also statistically significant decreases in weight and glucose after the surgery. The decrease in the leukocyte value was not significant, nor was it correlated with the CRP values. The correlation of the baseline values of CRP with weight and BMI was statistically significant.
The mean of the CRP baseline value of 1.15mg/l was above the normal value, which according to laboratory standards and the turbidimetric methods used in the SYNCHRON LX, should be<0.8mg/l. Moreover, the mean glucose value was 100.58, slightly above the upper limit of the test.
There were no significant differences in the results according to the type of surgery performed. Therefore, the data analysis was carried out using the sample total.
The Pearson correlation coefficient between variables does not show a cause-and-effect relation, but rather the degree of intensity of the possible relation between the variables. In the present case, the relation between the preoperative values of CRP and weight and CRP and BMI was linear and statistically significant (Figs. 1 and 2). The correlation coefficient between CRP and glucose was not statistically significant, which was probably due to the sample size, but there was a linear correlation between them. There was no linear relation between CRP and leukocytes or between CRP and the postoperative variables, which could be because the postoperative CRP changes were multifactorial and had no direct relation with the study variables. Furthermore, the postoperative CRP values were within normal ranges and so its sensitivity as an inflammation marker at that particular moment, was probably low.
Given that the preoperative leukocyte values were not high, their postoperative values were not expected to decrease significantly. There is no evidence that they are chronic inflammation markers, but their values are high in acute inflammatory processes.
There is little reported in the literature on the decrease of CRP after bariatric surgery in Mexican patients. Herrera et al.14 studied the effect of omentectomy on bariatric surgery and as a secondary aim, they measured the baseline and postoperative CRP values in 22 patients. They found no differences in performing omentectomy or not; a decrease in CRP was documented in both groups, but it was not statistically significant. In contrast, in the present study, the number of patients studied was over 50% higher (n=36) and the difference in preoperative and postoperative CRP was statistically significant. In addition, there was a statistically significant preoperative linear correlation between CRP and weight and BMI. Without a doubt, both studies provide some preliminary evidence in relation to inflammation and bariatric surgery in obese patients in the Mexican population. The similarities and differences in the behavior of the inflammation mediators among this population and others that have been widely studied in this respect remain to be explained.
Numerous studies on other populations worldwide have shown a decrease in CRP after bariatric surgery. Agrawal et al.15 conducted a retrospective study on a sample of 62 obese patients in which they evaluated the decrease in albuminuria and CRP levels after bariatric surgery. They found a statistically significant decrease of both values that was directly proportional to weight loss. In our study, there was a statistically significant correlation between the baseline values of CRP and weight and BMI, but not in the values at 6 months after surgery. As we have already mentioned, it was interesting that there was no postoperative linear correlation between these variables, reflecting the different and complex factors that intervene in the decrease of CRP values after bariatric surgery.
There are other inflammation mediators that have been studied postoperatively in gastric bypass patients. Orea et al.16 conducted a prospective study on 50 obese patients, measuring the serum concentrations of CRP and ICAM-1, before bariatric surgery and at 3, 6, and 12 months after the procedure, and found a significant decrease in both values. On the other hand, Illán et al.17 measured the serum values of adiponectin, CRP, TNFα, and IL-6 in 60 obese patients before laparoscopic gastric bypass surgery and at 6 and 12 months after the procedure; they found an increase in anti-inflammatory factor adiponectin and a significant decrease in IL-6 and CRP, but not in TNFα. Likewise, Pardina et al.18 found that the decrease in TNFα after bariatric surgery was not significant, whereas, CRP was statistically significant in serum, as well as in tissue. In addition, Saleh et al.19 corroborated the significant decrease in CRP and glucose in a study conducted on non-diabetic obese patients. They also observed a decrease in the carotid artery intima-media thickness and improvement in lipid metabolism.
It should be emphasized that in the present study, surgery achieved a 65% decrease in the baseline CRP levels at 6 months after the procedure. In a meta-analysis by Raghavendra,20 published in 2012, they included observational studies that evaluated changes in CRP, TNFα, and IL-6 in obese patients after bariatric surgery. There was a decrease in the CRP values of 66%, which was very similar to what we reported, as well as a 27% decrease in IL-6, and a non-significant decrease in TNFα.
ConclusionsCRP had a significant preoperative linear relation to weight and BMI. The patients studied that underwent gastric bypass and sleeve gastrectomy procedures presented with a significant postoperative decrease in CRP, weight, and glucose values. There are many likely factors that intervene in CRP reduction after bariatric surgery and their relation is non-linear. Further studies are needed to corroborate whether the decrease in CRP as a marker of a proinflammatory state is related to a decrease in the incidence of other diseases and to a reduced risk for cardiovascular disease in these patients.
Financial disclosureNo financial support was received in relation to this article.
Conflict of interestThe authors declare that there is no conflict of interest.
Please cite this article as: Rojano-Rodríguez ME, Valenzuela-Salazar C, Cárdenas-Lailson LE, et al. Nivel de proteína C reactiva en pacientes con obesidad mórbida antes y después de cirugía bariátrica. Revista de Gastroenterología de México. 2014;79:90–95.