Ischemic colitis (IC) is the most common cause of intestinal ischemia (60-70%). Fulminant presentation occurs in less than 5% of all cases, but it is a life-threatening situation with a high mortality rate1,2. The causes of IC have been classified as systemic or local, occlusive or non-occlusive, and iatrogenic or non-iatrogenic, with post-embolization IC standing out in the latter group3. We report herein a case of arterial post-embolization fulminant IC.
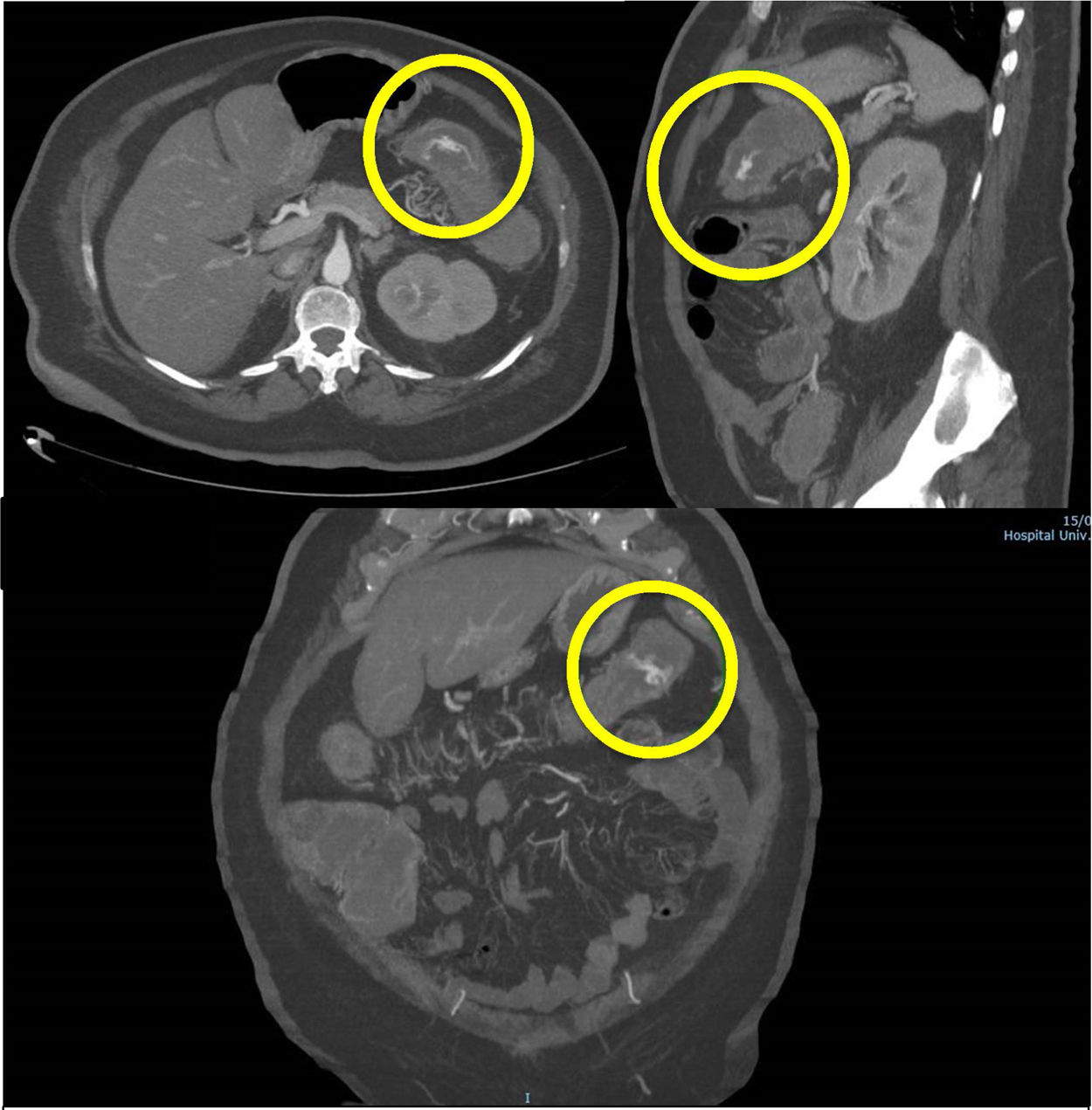
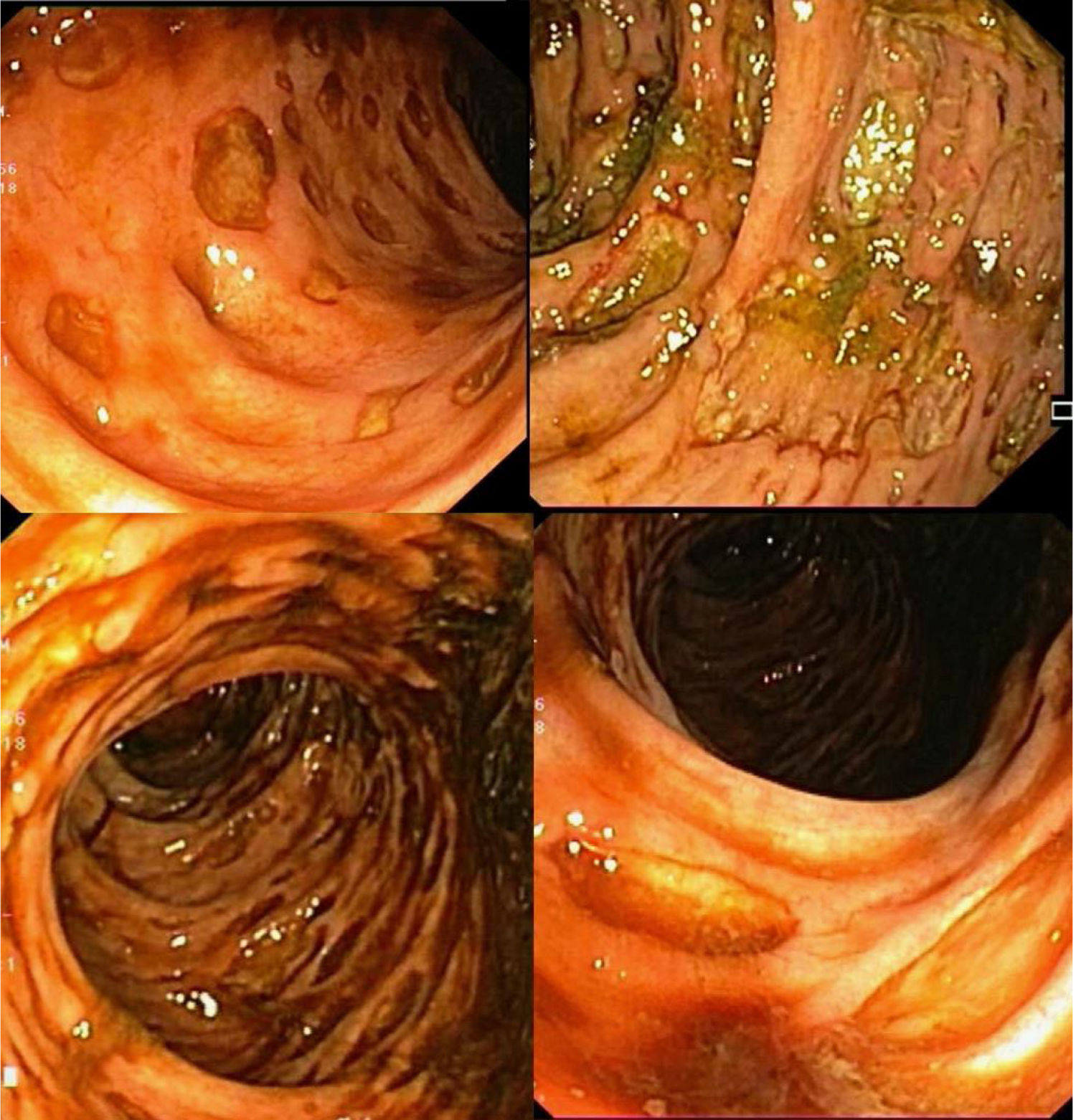
A middle-aged female patient, with a personal history of high blood pressure, type 2 diabetes mellitus, and dyslipidemia, was admitted for abdominal pain and vomiting of 2-month progression. Two days later, she developed rectal bleeding, with hemodynamic instability (Hb 6 g/dl), and acute renal failure (Cr 6 mg/dl). Abdominal CT-angiography showed active intraluminal bleeding, arising from the splenic flexure (Fig. 1). Superselective arterial embolization of the distal branch of the left colic artery was performed, utilizing microspheres, with no immediate adverse events. At 24-48 h post-embolization, after new episodes of massive rectal bleeding, urgent colonoscopy was performed, leading to a diagnosis of fulminant ischemic pancolitis (Fig. 2).
Due to persistent hemodynamic instability and massive rectal bleeding, with no response to conservative treatment, urgent surgical intervention was decided upon and total colectomy with ileostomy was carried out.
The histopathologic evaluation of the surgical specimen confirmed the diagnosis of gangrenous IC.
Fulminant forms of IC, resulting in gangrenous necrosis with perforation, peritonitis, and death, do not exceed 5%. Only clinical suspicion confirmed by endoscopic findings enables early diagnosis and salvage therapy (colectomy in most cases)2,4.
Multiple factors predispose to the development of IC. The most common causes are non-occlusive (atherosclerosis, hypoperfusion states, etc.), whereas the occlusive forms are more atypical. Those secondary to embolization are now exceptional1.
Adverse events of arterial embolization are infrequent because most procedures are currently performed utilizing superselective catheterization5,6. In a large study on 134 patients, intestinal ischemia was below 6%7.
The risk of symptomatic intestinal ischemia depends on the clinical-anatomic setting of the patient and the technical aspects of the interventional radiology procedure. Procedure-related aspects that minimize said adverse event include the adequate selection of the embolization agents and avoidance of extensive embolization4,8. The few cases of intestinal ischemia reported after superselective embolization have been due to the fact that the compensatory collateral circulation pathways were not respected, as likely occurred in the present report.
Nevertheless, choosing a suitable embolic agent is important. Available options include microcoils, gelfoam, polyvinyl alcohol (PVA), and microspheres, and outcomes vary, depending on the material chosen and its utilization. Gelfoam is used as a temporary embolic agent and is relatively safe, but it is not conducive to complete embolization and the rate of recurrent bleedings is higher than that of other embolic agents. Particles achieve rapid and complete embolization of the target artery, regardless of artery type and diameter. However, the complication rate is higher than that of other agents, owing to the high risk of non-target embolization. Microspheres present a greater risk for ischemia, compared with PVA particles, due to the more distal vascular occlusion that appears to be related to their compressibility capacity. Microcoils can be clearly seen in lateral fluoroscopic imaging and are easily and accurately positioned. Although we used gelfoam fragments and particles safely and successfully, those agents have their disadvantages. For example, they are not sufficiently radiopaque, thus the final resting position cannot be easily controlled, which makes manipulating the quantity of the agents more difficult. We performed embolization with gelfoam fragments and particles. Because it is a procedure that is not as tightly controlled as embolization with microcoils, it is more likely to trigger bowel infarction6,7.
Although uncommon, fulminant IC is a life-threatening condition with a high mortality rate2, if an urgent therapeutic approach is not performed4–7,9. To minimize its risk, superselective embolization should be used whenever possible7, keeping in mind that adverse events related to the clinical-anatomic setting of the patient can still occur.
Ethical considerationsInformed consent was not required for the present type of study. Consent for publication was obtained, regarding all personal data included in the case.
FundingThis study was not supported by any funding.
Conflict of interestThe authors declare that they have no conflict of interest.
Please cite this article as: Valdés-Delgado T, Jiménez-García VA, Galván-Fernández MD. Embolización arterial para control de sangrado gastrointestinal bajo. ¿Tratamiento o complicación? Revista de Gastroenterología de México. 2022;87:119–122.