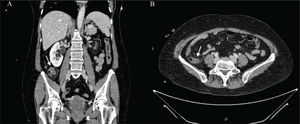
A 62-year-old woman, with an unremarkable past history, arrived at the emergency department, presenting with abdominal pain at the level of the right hemiabdomen, fever of 39.5°C, likely due to a bacterial infection, together with nausea and unaltered bowel habit. Laboratory tests reported a C-reactive protein value of 91mg/l (reference value 0–5), procalcitonin level of 6.3ng/mL (reference value 0.02–0.5), and a leukocyte count of 16,500IU/l, with 94% neutrophils. Given the clinical and laboratory data, abdominal computed tomography (CT) scanning was ordered that identified a diverticular formation in the terminal ileum, with inflammatory changes, suggestive of diverticulitis (Fig. 1A and B). Blood cultures obtained upon the patient’s arrival revealed the growth of Eggerthella lenta. She was hospitalized and intravenous antibiotic therapy was started with amoxicillin/clavulanic acid, resulting in good progression. The patient was discharged, with outpatient follow-up. Once the acute episode was resolved, colonoscopy with ileoscopy was ordered, confirming the presence of said diverticula at the level of the terminal ileum (Fig. 2).
With the exception of Meckel’s diverticulum, the presence of diverticula in the ileum is a rare entity. Its incidence in the general population varies from 0.3 to 2.3%, according to the most recent case series1. Its pathogenesis is attributed to herniation of the mucosa and submucosa, through the intestinal muscle layer, due to local increases in intraluminal pressure and smooth muscle anomalies. The majority of cases (60%) tend to be asymptomatic. When symptoms are present (40%), only a small portion of those cases (10%) develop severe complications. The main complication is diverticulitis, but bleeding and intestinal obstruction can also manifest2. The delayed diagnosis of diverticulitis can result in intestinal perforation. Endoscopic access to the ileum and its visualization through conventional imaging techniques are difficult, making the diagnosis of diverticula at that site challenging, and they are often detected intraoperatively2,3. There is no clear consensus on their therapeutic management. Even though intestinal resection with primary anastomosis appears to be the treatment of choice, conservative medical management with antibiotic therapy should be considered in mild cases3,4.
Ethical considerationsThe authors declare that the manuscript contains no personal information that can identify the patient, who signed a statement of informed consent for the performance of the studies. The corresponding author is in possession of said document. No experiments were conducted on animals or humans. The correct protocol was followed at all times, with the agreement of the patient and her family.
Financial disclosureNo financial support was received in relation to this article.
Conflict of interestThe authors declare that they have no conflict of interest.
Please cite this article as: García-Márquez J, García-Verdejo FJ, Caballero-Mateos AM. Diverticulitis aguda en íleon terminal: un caso raro a tener en cuenta. Rev Gastroenterol Méx. 2022;87:118–119.