Metastatic gastrointestinal lesions from the lung can appear at any part of the gastrointestinal tract and usually present at advanced stages of the disease, conferring poor prognosis. Duodenal appearance is exceptional and jejunal involvement implies a greater risk for perforation.1–3
We present herein two cases of patients with anemia due to metastasis to the small bowel as the initial presentation of lung cancer.
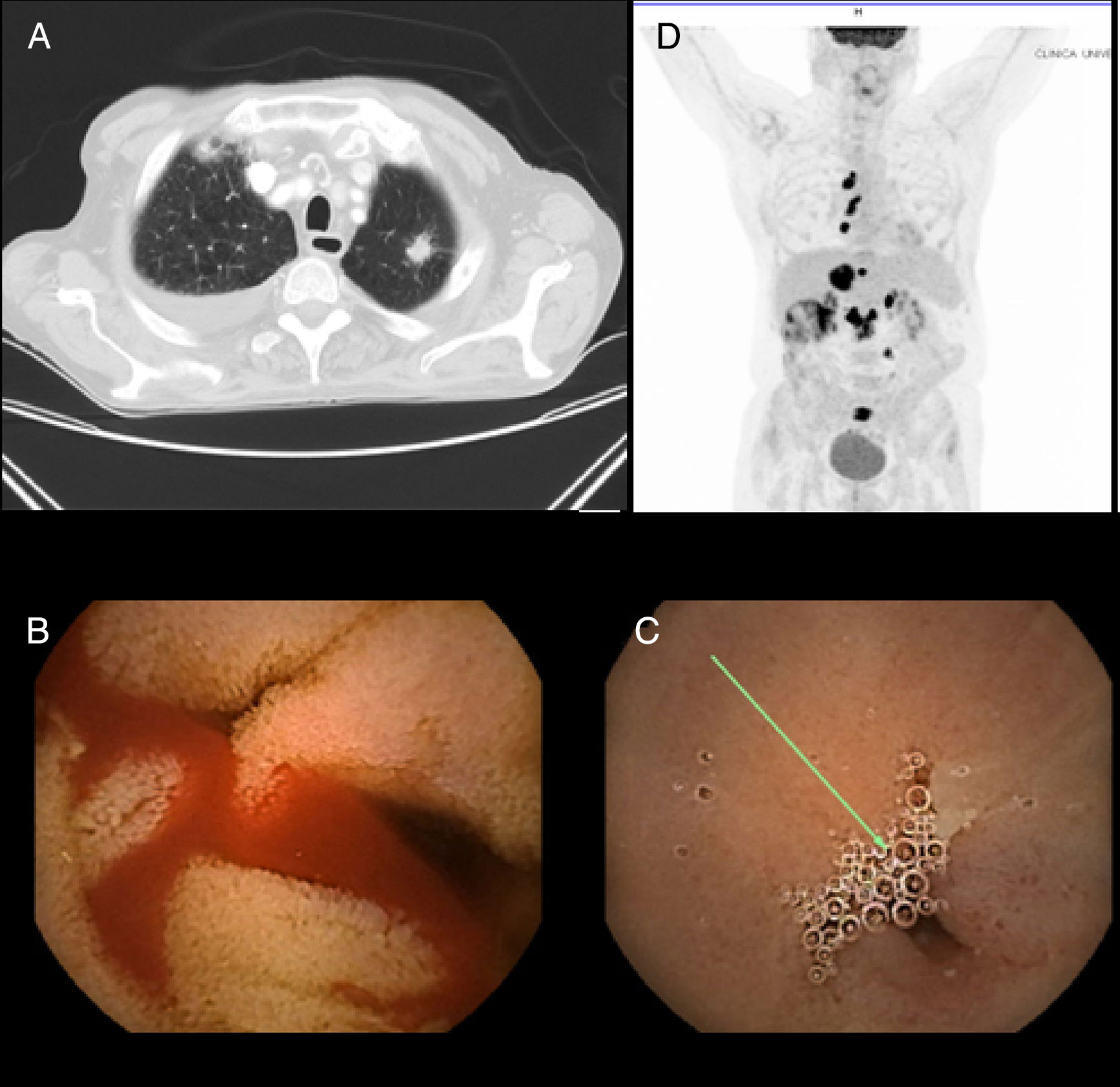
The first case corresponds to an 86-year-old man, ex-smoker, admitted to the hospital for constitutional symptoms and asymptomatic anemia. Complementary imaging studies (ultrasound and abdominal computed tomography [CT]) identified nonspecific duodenal involvement. At endoscopy, the duodenum showed signs of neoplastic infiltration. The histologic study revealed a poorly differentiated non-small cell carcinoma of pulmonary origin. Chest CT identified a 15 x 19 x 20mm spiculated nodule in the left upper lobe suggestive of a primary tumor of the lung (positive CAM 5.2 and TTF1) (fig. 1 A). Given the age of the patient, his comorbidity, and quality of life based on a previous Eastern Cooperative Oncology Group (ECOG) grade of 3-4, palliative management was decided upon and the patient died 4 months later.
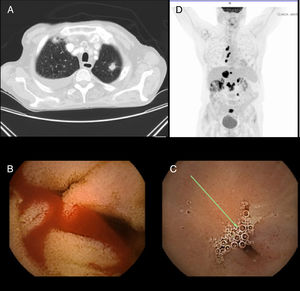
A) CT image in which a spiculated nodule in the left upper lobe suggestive of a primary lung tumor is identified. B) Capsule endoscopy image with angiodysplastic lesions in the jejunum with active bleeding. C) Capsule endoscopy image with jejunal stricture. D) PET image showing uptake in the mediastinal and peritoneal lymph nodes suggestive of dissemination.
The second case was a 68-year-old man, ex-smoker, who presented with severe iron deficiency anemia. Capsule endoscopy revealed angiodysplastic lesions in the jejunum with active bleeding, along with possible jejunal stricture (fig. 1B and C). CT confirmed jejunal neoplasia with lymph node involvement and liver metastases. Further study included a chest CT scan and positron emission tomography (PET) scan, confirming the presence of disseminated disease with a primary tumor of the lung (stage IV). Immunohistochemical analysis of the biopsies identified the adenocarcinoma subtype (positive CAM 5.2; negative CDX-2 and keratin 20; positive TTF1 and keratin 7) (fig. 1D). Given the patient's good general condition, chemotherapy was begun (carboplatin [CBDCA]+Alimta+atezolizumab) with good response (survival at 5 months from diagnosis).
Lung cancer is the first cause of death by cancer in the Spanish environment and 50% of the cases develop metastasis. The most frequent subtype is non-small cell carcinoma (85%).1,4–8
The gastrointestinal tract is an atypical location of metastatic lung cancer (0.5-1.3%), even though autopsy studies determine that its involvement is underdiagnosed (4.7-14%), especially when associated with the large cell subtype.1,3,5,6,8
The majority of patients are asymptomatic or present with the nonspecific symptoms of anemia, perforation, malabsorption, obstruction, or even appendicitis.3,5 Gastric or jejunal involvement can begin as a perforation and degenerate into secondary peritonitis, whereas tumors that grow rapidly usually begin as obstruction.3,5 Perforation is also related to the use of chemotherapy (especially bevacizumab) due to the tumor response secondary to treatment that produces cellular necrosis and thinning of the wall, favoring that complication.1
There is diagnostic suspicion of lung cancer in patients that begin with digestive symptoms or anemia, but those symptoms can also be the onset of the disease, given that they have been reported as the first manifestation in some case series. Gastrointestinal metastases condition a worse general outcome because they are related to a more advanced phase of disease when diagnosed.
Regarding perforation as a form of presentation, in 2004 Garwood carried out a review of 98 patients that presented with intestinal perforation secondary to metastatic lung cancer, identifying the jejunum as the first location (53%), followed by the ileum (28%). Perforation was associated with the histologic subtype of pulmonary adenocarcinoma (23.7%), followed by squamous cell carcinoma (22.7%), large cell carcinoma (20.6%), and small cell carcinoma (19.6%). Mean survival in that subgroup of patients was 66 days, 50% of the patients did not survive more than 30 days, and 1-year survival was less than 3%.9,10
The majority of authors describe the small bowel as the main location of gastrointestinal involvement in 2.6-10.7% of the cases.2,3,5–9 The case series by Antler et al. is the exception. They describe the esophagus as the most affected organ (chiefly as a result of contiguity).6
Few cases of duodenal involvement are reported (15 cases published from 1999 to the present) and presentation is varied.
In 2011, Yamada et al. conducted a systematic bibliographic search of the cases of duodenal involvement published between 1999 and 2007, including the terms «lung cancer» and «duodenal metastasis». Nine cases were identified and only 2 of them presented with asymptomatic anemia.2
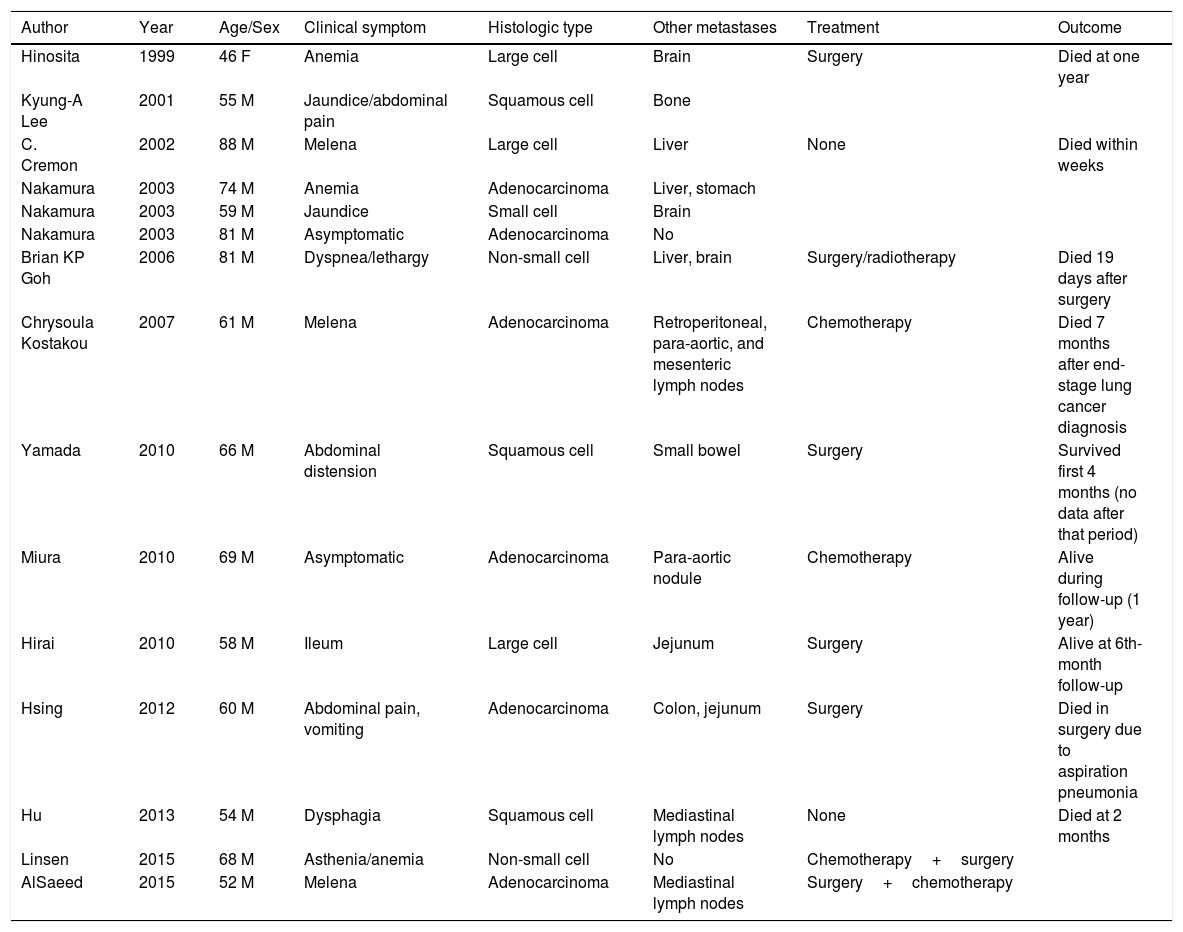
We completed the search up to the present date on Medline through PubMed with the same search criteria (Table 1) and identified a total of 15 cases.
Cases of metastatic duodenal involvement due to a primary tumor of the lung.
| Author | Year | Age/Sex | Clinical symptom | Histologic type | Other metastases | Treatment | Outcome |
|---|---|---|---|---|---|---|---|
| Hinosita | 1999 | 46 F | Anemia | Large cell | Brain | Surgery | Died at one year |
| Kyung-A Lee | 2001 | 55 M | Jaundice/abdominal pain | Squamous cell | Bone | ||
| C. Cremon | 2002 | 88 M | Melena | Large cell | Liver | None | Died within weeks |
| Nakamura | 2003 | 74 M | Anemia | Adenocarcinoma | Liver, stomach | ||
| Nakamura | 2003 | 59 M | Jaundice | Small cell | Brain | ||
| Nakamura | 2003 | 81 M | Asymptomatic | Adenocarcinoma | No | ||
| Brian KP Goh | 2006 | 81 M | Dyspnea/lethargy | Non-small cell | Liver, brain | Surgery/radiotherapy | Died 19 days after surgery |
| Chrysoula Kostakou | 2007 | 61 M | Melena | Adenocarcinoma | Retroperitoneal, para-aortic, and mesenteric lymph nodes | Chemotherapy | Died 7 months after end-stage lung cancer diagnosis |
| Yamada | 2010 | 66 M | Abdominal distension | Squamous cell | Small bowel | Surgery | Survived first 4 months (no data after that period) |
| Miura | 2010 | 69 M | Asymptomatic | Adenocarcinoma | Para-aortic nodule | Chemotherapy | Alive during follow-up (1 year) |
| Hirai | 2010 | 58 M | Ileum | Large cell | Jejunum | Surgery | Alive at 6th-month follow-up |
| Hsing | 2012 | 60 M | Abdominal pain, vomiting | Adenocarcinoma | Colon, jejunum | Surgery | Died in surgery due to aspiration pneumonia |
| Hu | 2013 | 54 M | Dysphagia | Squamous cell | Mediastinal lymph nodes | None | Died at 2 months |
| Linsen | 2015 | 68 M | Asthenia/anemia | Non-small cell | No | Chemotherapy+surgery | |
| AlSaeed | 2015 | 52 M | Melena | Adenocarcinoma | Mediastinal lymph nodes | Surgery+chemotherapy |
Of the 15 articles, only the case reported by Linsen et al. presented with the initial symptom of anemia with no visible bleeding, as the first such patient described.4 The majority of the patients (93.3%) were men, with a mean age of 59 years. Adenocarcinoma was the most frequently associated type of primary tumor of the lung (40%).
Data on the treatment received was available in 11 patients and only 5 were candidates for surgery. Mean survival was < 50% at 3 months, but there were cases of prolonged survival.1,3,5,7
Management depends on the basal state of the patient, the control of the primary disease focus, and the number of metastatic lesions. Resection, with or without chemotherapy, can be performed in well-localized lesions.
Larger studies of patients are needed to establish adequate management in terms of treatment, the prevention of complications, and indicators of medium-term and long-term survival.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of dataThe authors declare that they have followed the protocols of their work center on the publication of patient data.
Right to privacy and informed consentThe authors declare that no patient data appear in this article.
Financial disclosureNo financial support was received in relation to this study/article.
Conflict of interestThe authors declare that there is no conflict of interest.
Please cite this article as: Saldaña-Dueñas C, Rullán-Iriarte M, Macías-Mendizábal E. Anemia como presentación inicial del cáncer de pulmón con afectación intestinal metastásica. Revista de Gastroenterología de México. 2019;84:259–262.