Rectal prolapse is common in the elderly, having an incidence of 1% in patients over 65years of age. The aim of this study was to evaluate the safety and feasibility of a new endoluminal procedure for attaching the previously mobilized rectum to the anterior abdominal wall using an endoscopic fixation device.
Materials and methodsThe study is a single-arm phasei experimental trial. Under general anesthesia, total rectal prolapse was surgically reproduced in five pigs. Transanal endoscopic reduction of the rectal prolapse was performed. The best site for transillumination of the abdominal wall, suitable for rectopexy, was identified. The EndoLifter was used to approximate the anterior wall of the proximal rectum to the anterior abdominal wall. Two percutaneous rectopexies were performed by puncture with the Loop FixtureII Gastropexy Kit® at the preset site of transillumination. After the percutaneous rectopexies, rectoscopy and exploratory laparotomy were performed. Finally, the animals were euthanized.
ResultsThe mean procedure time was 16min (11-21) and the mean length of the mobilized specimen was 4.32cm (range 2.9-5.65cm). A total of 10 fixations were performed with a technical success rate of 100%. There was no evidence of postoperative rectal prolapse in any of the animals. The EndoLifter facilitated the process by allowing the mucosa to be held and manipulated during the repair.
ConclusionsEndoscopic-assisted percutaneous rectopexy is a safe and feasible endoluminal procedure for fixation of the rectum to the anterior abdominal wall in experimental animals.
El prolapso rectal es común en los pacientes de edad avanzada, con una incidencia del 1% en los mayores de 65años. El objetivo de este estudio fue evaluar la seguridad y la factibilidad de un nuevo procedimiento endoluminal para la fijación a la pared abdominal anterior del recto previamente movilizado utilizando un dispositivo de fijación endoscópica.
Materiales y métodosEl estudio es un ensayo experimental fasei de brazo único. La reproducción quirúrgica del prolapso rectal fue realizada bajo anestesia general en 5 cerdos. Se llevó a cabo la reducción endoscópica transanal del prolapso rectal. Se identificó el mejor sitio para la transiluminación de la pared abdominal, adecuado para rectopexia. El EndoLifter se utilizó para aproximar la pared anterior de la parte proximal del recto a la pared abdominal anterior. Se realizaron 2 rectopexias percutáneas con el Loop FixtureII Gastropexy Kit® en el sitio preestablecido de transiluminación. Posteriormente se llevaron a cabo rectoscopia y laparotomía exploratoria. Por último, los animales fueron sacrificados.
ResultadosEl tiempo promedio del procedimiento fue de 16min (11-21) y la longitud promedio del recto movilizado fue de 4.32cm (rango 2.9-5.65cm). Se realizaron un total de 10 fijaciones, con una tasa de éxito técnico del 100%. No hubo evidencia de prolapso rectal postoperatorio en ninguno de los animales. El EndoLifter facilitó el proceso al permitir la manipulación de la mucosa durante la pexia.
ConclusionesLa rectopexia percutánea asistida por endoscopia es un procedimiento endoluminal seguro y factible para la fijación del recto a la pared abdominal anterior en animales de experimentación.
Rectal prolapse, or procidentia, is defined as a protrusion of the rectum beyond the anal verge.1 Rectal prolapse is common in the elderly, having an incidence of around 1% in patients over 65 years of age.2 Predisposing factors include lax muscles of the pelvic floor and anal canal,3 an abnormally deep pouch of Douglas,4 weakness of both the internal and external sphincters,5 and weakness of the lateral ligaments.6 The pathogenesis of complete rectal prolapse is therefore very complex and its treatment is primarily surgical.7
The aim of this study was to evaluate the safety and feasibility of a new endoluminal procedure for attaching the mobilized rectum to the anterior abdominal wall using an endoscopic fixation device in an in vivo animal model.
Materials and methodsThe protocol was approved by the institutional Gastroenterology Department Review Board. Procedures were conducted in the experimental laboratory of the School of Medicine's Complejo Hospitalario del Hospital Das Clínicas of the Universidad de Sao Paulo.
The study is a single-arm phase I experimental trial. Five healthy domestic female Yorkshire pigs were used. The animals had a mean pre-procedure weight of 35kg (32 to 40kg range) and had undergone no previous surgery. They were kept fasting 24h before the intervention and received 1,250ml of a 20% mannitol solution the day before the procedure for rectal and colon cleansing.
In the lithotomy position with legs spread apart, all the animals underwent tracheal intubation and mechanical ventilation. They were kept under general anesthesia with a ketamine® base (intravenous 5mg/kg) and thiopental® (intravenous10-30mg/kg), followed by isoflurane® inhalation.
Mobilization of the rectum and surgical reproduction of total rectal prolapseMobilization of the rectum to the pelvic floor via the open approach was completed through sharp dissection and a bipolar electrosurgical device. The avascular presacral plane was carefully dissected and the descending colon was laterally mobilized.
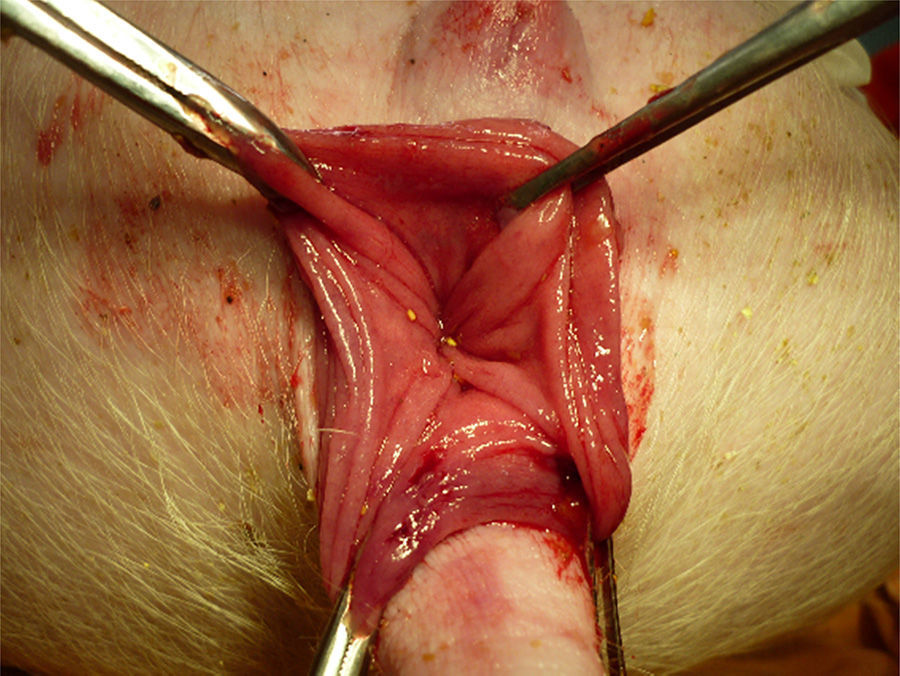
Pneumatic dilation of the anus was performed with a 30mm diameter dilator (fig. 1). Finally, an anoscope was inserted into the anus, and the mucosa of the mobilized rectum was pushed outwards with the Allis retractor (fig. 2).
Rectopexy techniqueAll examinations were performed by a single endoscopist with advanced skills. Rectopexies were carried out by an experienced colorectal surgeon.
After total rectal prolapse was surgically reproduced, the following steps were followed:
- 1.
Preparation of the abdominal wall with povidone-iodine and saline solution.
- 2.
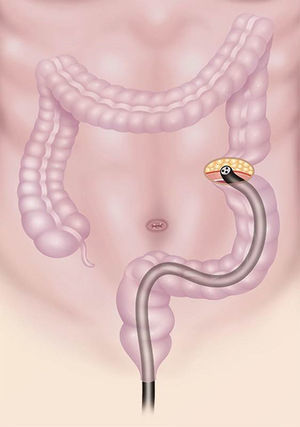
Transanal introduction of the endoscope (Pentax EG–290) and reduction of the rectal prolapse.
- 3.
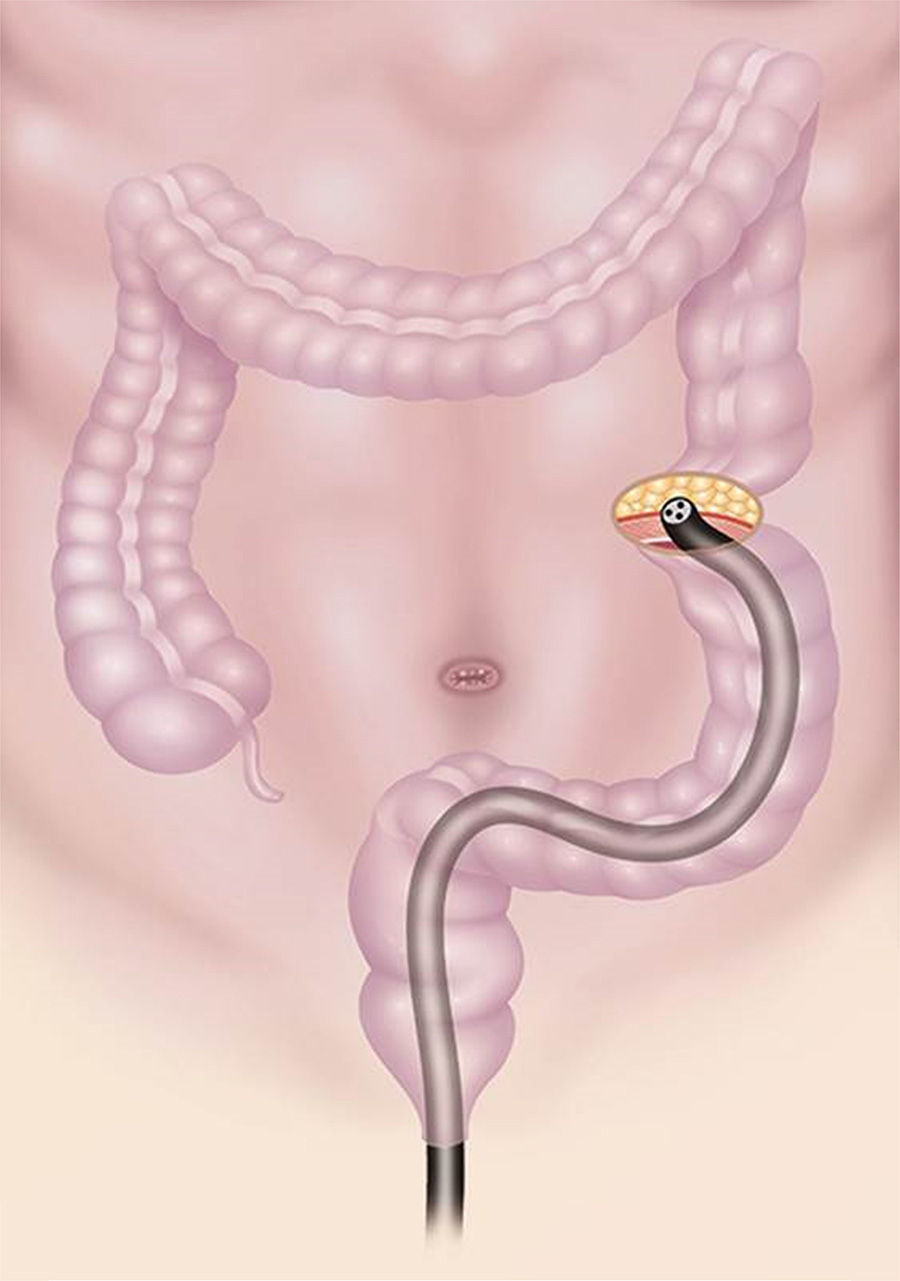
Identification of the best site for transillumination of the abdominal wall, suitable for rectopexy (fig. 3).
- 4.
The EndoLifter was used to retract and approximate the anterior wall of the proximal rectum to the anterior abdominal wall.8
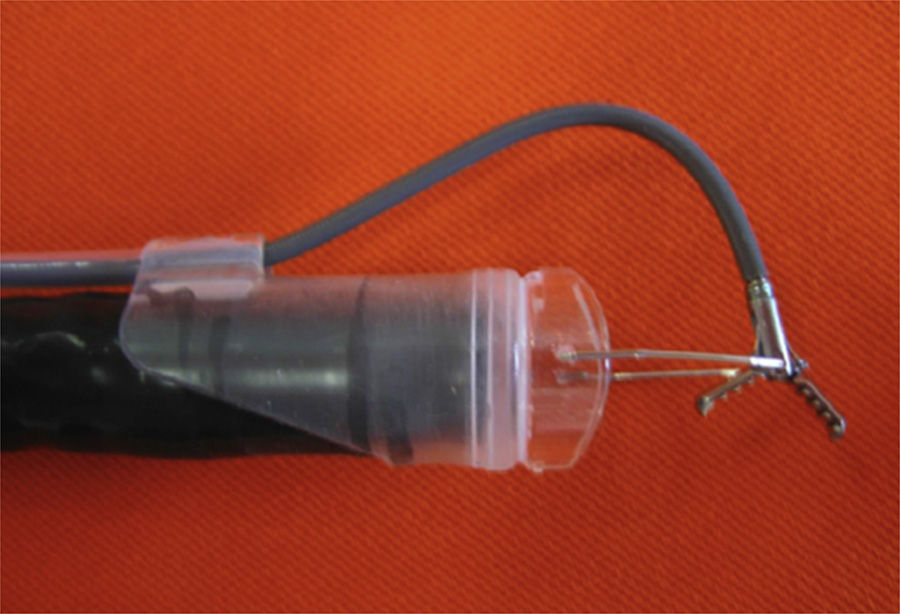
The device consists of a retractable grasping forceps attached to a transparent cap by a hinge that allows simultaneous grasping, retracting, and lifting of the mucosa (fig. 4). The transparent cap measures 13.85mm in diameter and could be attached to the tip of the 9.8-mm endoscope. Upon approximating the anterior rectal wall, the retractable forceps were first extended and the specific site where the fixation would be performed was then grasped. The forceps were then partially retracted to lift up the mucosa of the anterior rectal wall, approximating it to the anterior abdominal wall.
- 5.
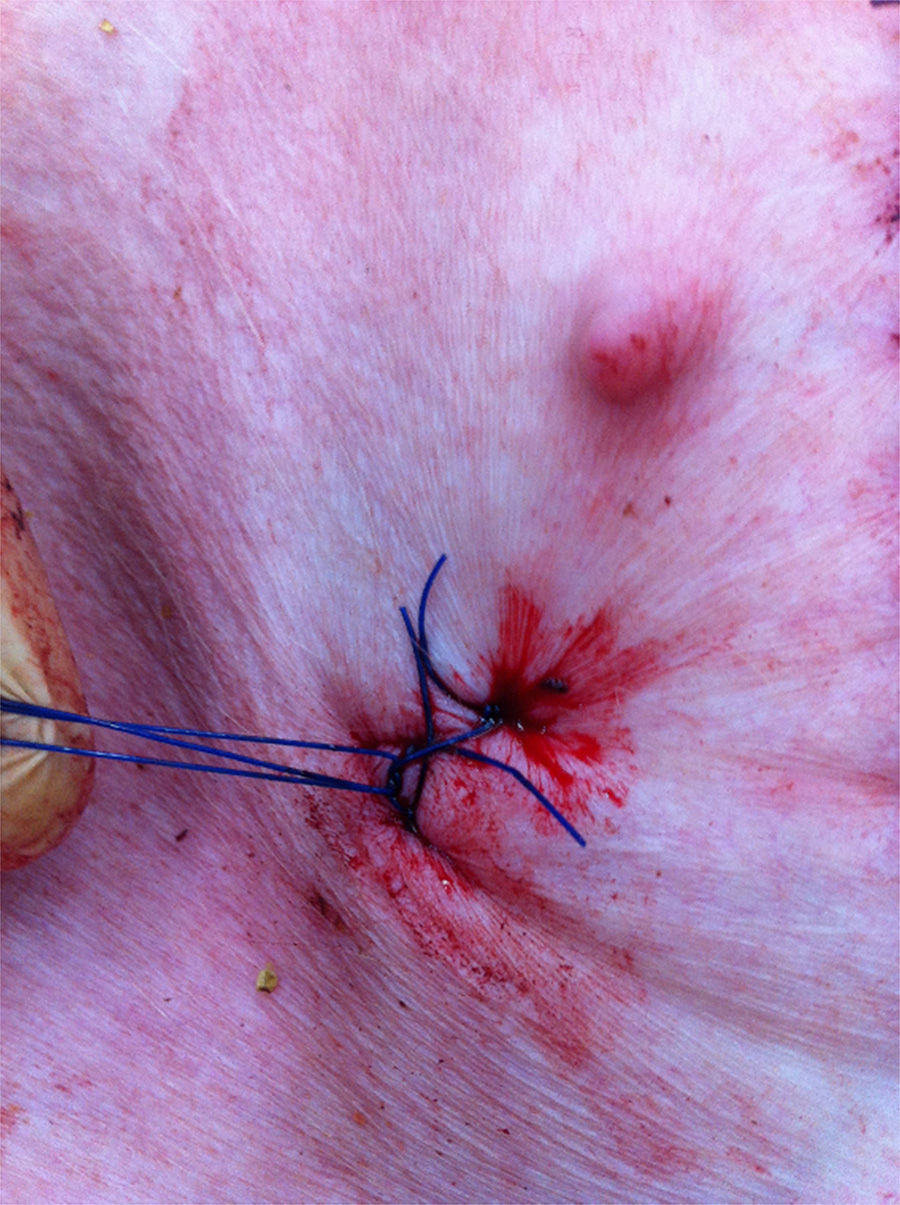
Two percutaneous rectopexies were performed by puncture with the Loop Fixture II Gastropexy Kit® at the preset transillumination site (fig. 5). Briefly described, this device has 2 needles, one that has a suture inserted through it just before the tip of the needle, and the other with a suture-holding loop.
- 6.
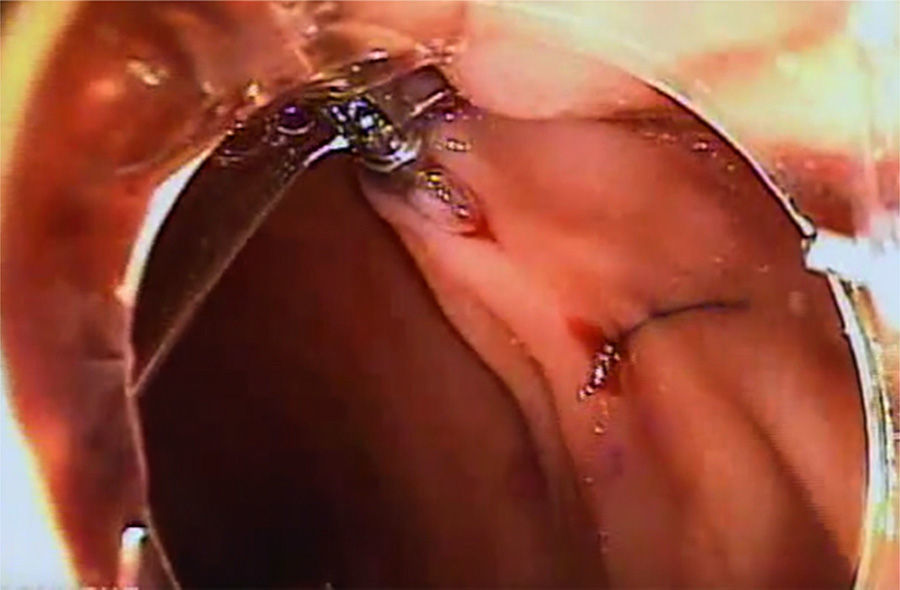
Under endoscopic observation, the suture-holding needle was pushed downwards to form a loop for holding the suture.
- 7.
The suture was advanced downwards so that its distal end passed through the suture-holding loop.
- 8.
After endoscopic confirmation that the distal end of the suture had passed through the suture-holding loop, the loop was once again placed in the puncture needle (fig. 6).
- 9.
The Loop Fixture II (fig. 7) was pulled out and the suture-holding needle pushed downwards to form a loop for releasing the free suture. The free suture was knotted against the abdominal wall to hold the anterior rectal wall to the parietal peritoneum.
- 10.
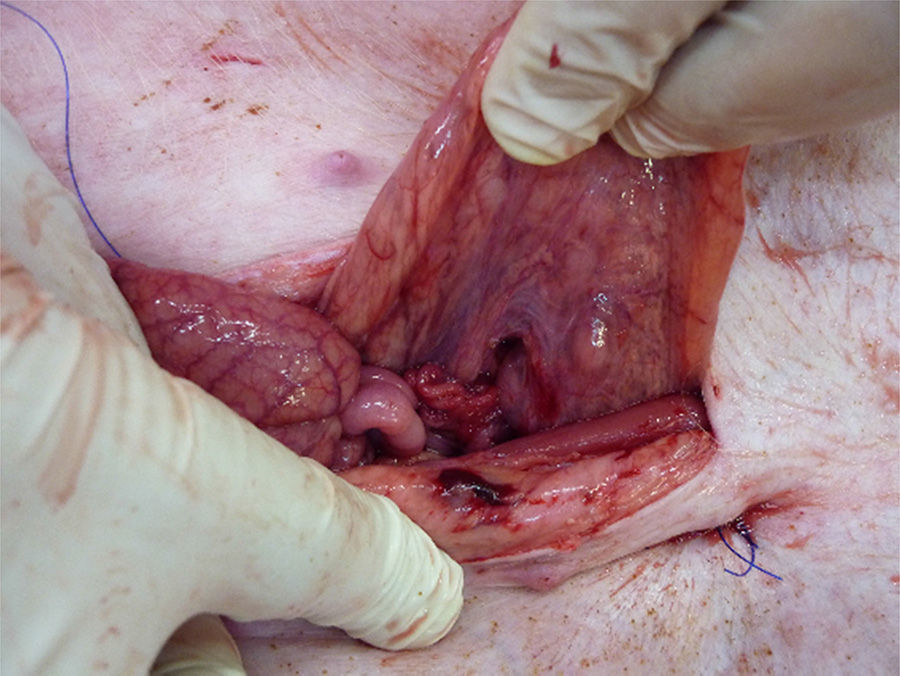
After the percutaneous rectopexies, rectoscopy and exploratory laparotomy were performed (fig. 8).
- 11.
Finally, the animals were euthanized.
The mean procedure time was 16min (11-21), and the mean length of the mobilized specimen was 4.32cm (2.9-5.65cm range).
A total of 10 fixations were performed with a technical success rate of 100%.
The procedures were carried out with no clinically important complications, such as perforations or massive bleeding, except for minor rectal bleeding in one animal. There was no postoperative evidence of rectal prolapse in any of the animals. The rectum remained firmly fixed to the anterior abdominal wall, with no protrusion or prolapse.
The EndoLifter facilitated the process by enabling the mucosa to be held and manipulated during the fixation, thus aiding in exposing the best puncture site.
The Valsalva maneuver was performed to confirm the absence of rectal prolapse recurrence, which did not present in any of the animals.
DiscussionWe demonstrated the feasibility and safety of the endoluminal fixation of the anterior rectal wall to the anterior abdominal wall, proposing a less invasive method for treating rectal prolapse by eliminating the need for general anesthesia, avoiding bowel resection and abdominal incisions, thus offering the possibility of a shorter hospital stay and a faster recovery.
Rectal prolapse occurs most commonly in elderly patients. They are more susceptible to perioperative complications, particularly those related to anesthesia and those of cardiovascular, respiratory, and infectious etiology.9
Even though laparoscopic surgery has emerged as an effective therapeutic approach for rectal prolapse, postoperative morbidity and mortality in the elderly remains a concern.10,11 A recent retrospective French study evaluated the safety of laparoscopic ventral rectopexy in the elderly. A total of 4,303 patients from a national database were included. Patients over 70 years of age were compared with patients younger than 70. Elderly patients had more minor complications (urinary, wound complications) and a longer hospital stay, but there were no differences in the major complication and mortality rates between the two groups.12 However, others have reported significant cardiac morbidity in elderly patients that underwent laparoscopic rectopexy.13,14
Surgical innovation has not stopped at this frontier and has progressed even further in relation to minimally invasive access routes such as single-port surgery, natural orifice transluminal endoscopic surgery, robotic-assisted surgery, and endoluminal surgery.
More than 100 different techniques for the surgical correction of rectal prolapse have been described,15 and approaches can be perineal or abdominal. Due to their lower morbidity, perineal approaches are more frequently performed than abdominal operations in elderly patients. Rectopexy techniques are varied and include the use of sutures, staples, or meshes that are eventually combined with sigmoid resection. None of these operations can be regarded as ideal for every patient. Abdominal approaches have a lower recurrence rate, but they are significantly associated with higher rates of infection and complications, compared with transperineal approaches.16 This makes abdominal approaches preferable in medically fit patients. The transperineal approaches are usually reserved for those patients that cannot tolerate the abdominal procedure. Even though these operations are performed frequently, a comparison and evaluation of the different methods is difficult. In the PROSPER study, a randomized comparison of surgical treatments for rectal prolapse was carried out. Patients were randomized between abdominal and perineal surgery (1), and suture vs resection rectopexy for those undergoing an abdominal procedure (2), or the Altemeier procedure vs the Delorme procedure for those having a perineal procedure (3). Primary outcome measures were prolapse recurrence, incontinence, bowel function, and quality of life scores measured up to 3 years. No significant differences were seen in any of the randomized comparisons, although substantial improvements from the quality of life baseline were observed following all the procedures.17
The use of the anterior abdominal wall is not, in fact, a new approach and has been documented in the medical literature at least as early as 1930.18 Advances in therapeutic endoscopic techniques have facilitated the improvement of previous approaches. Although the feasibility of endoscopic rectopexy for total rectal prolapse in humans has not been studied, previous reports of percutaneous full-thickness fixation of the colonic wall aided by colonoscopy, with no signs of perforation, infection or fistulas, suggest the possible clinical application of this technique. Ventral endoscopic colopexy for sigmoid volvulus treatment has proven to be an effective therapeutic procedure with low morbidity. Additionally, percutaneous gastropexy aided by endoscopic transillumination is a standard approach for patients with advanced esophageal neoplasia.19 Nevertheless, the feasibility of endoscopic rectopexy for total rectal prolapse in humans should be prospectively studied.
Endoscopic-assisted percutaneous rectopexy with the aid of the EndoLifter8 is a safe and feasible endoluminal procedure for fixation of the rectum to the anterior abdominal wall in experimental animals. Important potential advantages of this minimally invasive technique should be tested in humans and the functional improvement and recurrence rates should be measured to further demonstrate its clinical application.
Ethical responsibilitiesProtection of persons and animalsThe authors declare that the procedures followed conformed to the ethical standards of the responsible committee on human experimentation and were in accordance with the World Medical Association and the Declaration of Helsinki.
Data confidentialityThe authors declare that no patient data appear in this article.
Right to privacy and informed consentThe authors declare that no patient data appear in this article.
Financial disclosureNo financial support was received in relation to this article.
Conflict of interestThe authors declare that there is no conflict of interest.
The authors wish to thank the personnel of the Experimental Surgery Unit of the Incor-HC of the Universidad de Sao Paulo for their unconditional support in the realization of this study.
Please cite this article as: Bustamante-Lopez L, Sulbaran M, Sakai C, de Moura EG, Bustamante-Perez L, Nahas CS, et al. Una técnica novedosa para corrección de prolapso rectal completo: rectopexia percutánea asistida por endoscopia con ayuda del EndoLifter. Revista de Gastroenterología de México. 2016;81:202–207.