Mesenteric cysts are very rare intra-abdominal tumors with a minimum of clinical symptoms, making their preoperative diagnosis difficult. Diagnosis is generally made through abdominal ultrasound or computed tomography studies. The differential diagnosis should be made with other abdominal or retroperitoneal tumors. Treatment is surgical, with complete resection of the cyst through laparotomy or laparoscopy.
Given that this type of lesion is not often contemplated preoperatively and that its symptomatology can be very ambiguous, we present herein the case of a giant mesenteric cyst whose diagnosis was suspected in the preoperative period, but had previously been confused with another pathology.
A 65-year-old housewife with an obstetric history of gravida 1, para 0, abortus 1, cesarean section 0, had a ruptured ectopic pregnancy at 30 years of age for which she underwent an exploratory laparotomy with profuse intraoperative blood loss and several transfusions in the postoperative period. Her current illness had a 2-year progression and began with gradual, nonpainful abdominal growth that eventually became incapacitating. It caused dyspnea in the dorsal decubitus position, the patient was unable to get up on her own, and it limited her walking due to respiratory difficulty.
She was examined and managed by a general practitioner, who after numerous failed treatments with diuretics for apparent progressive ascites, referred her for control and management of cirrhosis due to post-transfusional hepatitis.
At her referral consultation, the patient presented with dyspnea after slight physical exertion, no cachexia or jaundice, and with an important increase and tension in abdominal volume, but no signs of chronic hepatopathy.
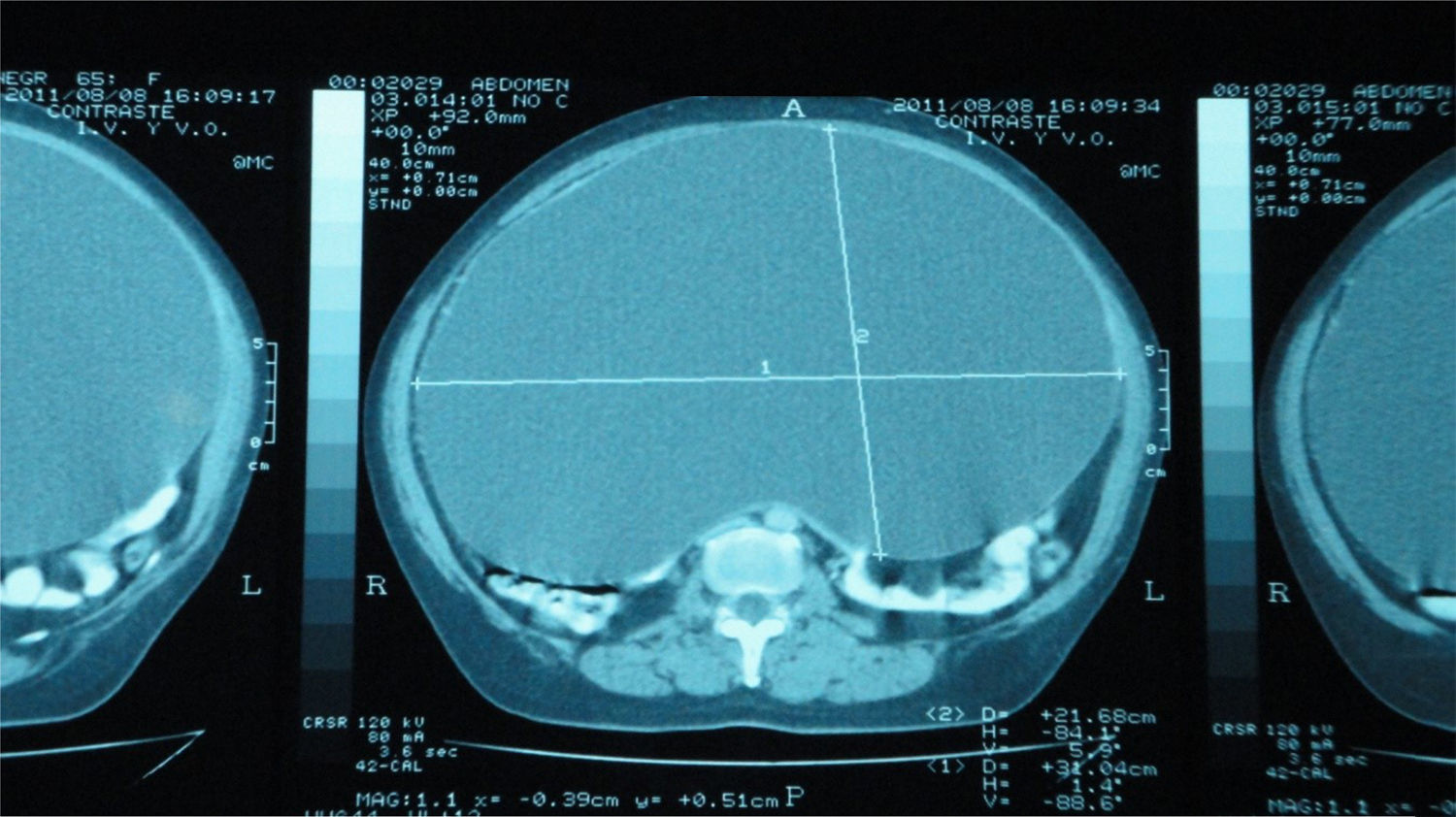
Complete blood count, blood chemistry, and liver function tests were ordered, all of which were normal. There were no indications of liver failure or thrombocytopenia due to hypersplenism. Ultrasound study was ruled out because the possibility of an intra-abdominal tumor was contemplated, and non-contrast and contrast-enhanced abdominal computed tomography scans were carried out instead. They revealed a liver with normal consistency and morphology, but that was importantly displaced toward the upper abdomen by a large, fluid-containing, thin-walled intra-abdominal mass that moved all the intra-abdominal viscera from their usual positions and took up the entire abdominal cavity. The preoperative diagnostic suspicion was a giant mesenteric cyst (figs. 1 and 2).
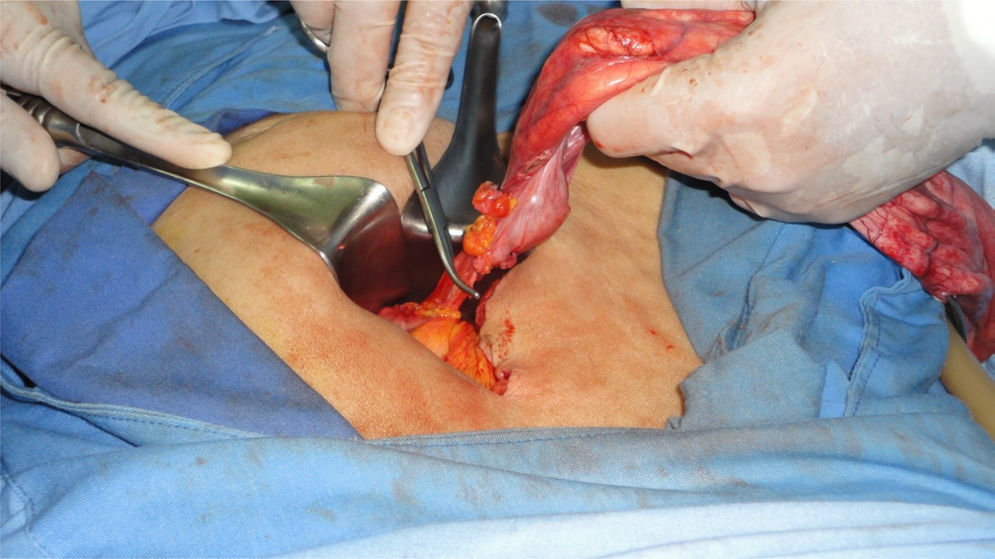
Having ruled out chronic hepatopathy, and given that the patient had normal coagulation tests, open laparotomy was performed. It revealed a giant mesenteric cyst that was not attached to any viscera and was only being nourished through its pedicle, which arose from the mesentery of the rectosigmoid colon. The patient had no alterations during the immediate postoperative period and was released from the hospital on the second day after surgery, tolerating oral diet well.
The histopathology study corresponded to: mesenteric (mesothelial) cyst.
Mesenteric cysts are very rare intra-abdominal cystic tumors with a prevalence from 1:100,000 to 1:250,000 of hospitalizations in adults and 1:20,000 in the pediatric population.1–4The origin of mesenteric cysts is not very clear and the following have been considered: lymphatic duct obstruction, lymphatic duct injury, lymph node degeneration, ectopic lymphatic tissue proliferation, and failure of the mesenteric sheets to fuse together. Congenital diseases, diverticula, pelvic cavity surgery, and inflammatory pelvic disease have also been described as possible etiologies.5
These cysts are generally asymptomatic, slow-growing, and benign. They are more frequent in women than in men and can be detected at any age, but their greatest incidence is in patients between 40 and 70 years of age.6
Size varies, with a mean up to 10cm in diameter. They do not cause specific symptomatology, and when symptoms do appear they are related to the gastrointestinal tract. Acute symptoms resulting from torsion, rupture, or bowel obstruction are extremely rare.7,8
Some uncommon cases have presented with complications, such as infection, hemorrhage, volvulus, perforation, ileus, and acute abdomen.9,10
As with all intra-abdominal tumors, diagnosis is easy to make through ultrasound or tomography, but the precise, preoperative diagnosis of mesenteric cyst is difficult because it is a rare entity with no specific symptoms.
Complete surgical resection is the treatment of choice and can be performed through laparotomy or laparoscopy.4–9In the majority of cases, the pedicle of the cyst is situated in the mesentery of the small bowel, involving that organ and often making bowel resection necessary, requiring end-to-end anastomosis after en bloc resection of the cyst. In other cases, the pedicle is located in the mesentery of the descending colon or the rectum.8
Our patient was referred to us with an erroneous diagnosis after numerous diuretic treatments, confusing the giant cyst with untreatable tension ascites secondary to a supposed cirrhosis from post-transfusion hepatitis.
The present case is interesting because the cyst was diagnosed in the preoperative period through abdominal tomography, which is extremely rare, and because of its very large size.
Resection through laparoscopy can be attempted in smaller tumors, but given the size of our patient's cyst, laparotomy was preferred. First the cyst was punctured and gradual decompression was carried out, so as not to cause hemodynamic alterations. Eleven liters of a clear, citrine fluid (fig. 3) were drained. Once the cyst was emptied, its vascular pedicle was located in the mesentery of the rectosigmoid colon and was clamped and cut (figs. 4 and 5).
The patient had a very satisfactory postoperative period and was released 48h later. There has been no recurrence or complication inherent to the pathology or surgery at the follow-up at 48 months.
The histopathology report was a mesothelial mesenteric cyst, corresponding to type 2 of the current classification, which considers 6 variants based on histopathologic characteristics: 1) cysts of lymphatic origin (simple lymphatic cysts and lymphangiomas), 2) cysts of mesothelial origin (simple mesothelial cyst, benign cystic mesothelioma, and malignant cystic mesothelioma), 3) cysts of enteric origin (enteric cysts and enteric duplication cysts), 4) cysts of urogenital origin, 5) mature cystic teratoma (dermoid cysts), and 6) pseudocysts (infectious and traumatic cysts).1 Malignancy presents in only 3% of the cases.4
In conclusion, mesenteric cyst is a rare, slow-growing entity, with no clinical pathognomonic signs. Its diagnosis is not considered in the preoperative period and it is generally diagnosed as an imaging study finding. All of these cysts should be resected through laparotomy or laparoscopy.
Financial disclosureNo financial support was received in relation to this article.
Conflict of interestThe authors declare that there is no conflict of interest.
Please cite this article as: Vallejo-Soto M, Orozco-Simental S. Quiste mesentérico gigante simulador de ascitis intratable. Revista de Gastroenterología de México. 2017;82:348–351.