Amoebiasis is caused by the protozoan, Entamoeba histolytica (E. histolytica). This parasite has 2 life stages: as a cyst, which is the infectious form, and as a trophozoite, which is the form that causes invasive disease. Approximately 500 million persons are annually infected worldwide,1 and frequently in poor countries, due to socioeconomic conditions and sanitation levels. The majority of cases are asymptomatic, but the disease can manifest as amoebic dysentery, amoebic liver abscess, and can sometimes affect the lungs, heart,2 and brain.3 Amoebiasis is situated between the third and fifth cause of death from parasitic disease at the world level.4E. histolytica trophozoites invade the colonic mucosa, causing inflammation. In some cases the amoebas break through the mucosal barrier 5 and travel through the portal circulation to the liver, where they cause abscesses. Amoebic liver abscess (ALA) is the most frequent extraintestinal manifestation of amoebiasis.6 It is estimated that from 2 to 5% of intestinal amoebiasis cases progress to liver abscess. Mexico has the characteristics of an endemic country, with a mean ALA rate of 3.66 per 100,000 inhabitants. An epidemiologic map of the country shows that few States are affected by ALA; in some the incidence rate is lower than the national mean. For example, in the federal entity of Mexico City, it is 0.69 and the rates in the following states are: Sinaloa, 11.37; Nayarit, 10.11; Colima, 9.5; and Chiapas, 11.1. Sonora has the highest rate,7 with 13.4. Hernández et al.8 and Valenzuela et al.9 explain this by showing that there are differences in the presence of alleles in the major histocompatibility complex (HLA-DRB1 and HLA-DQB1) among the inhabitants of different regions of the country, conferring resistance to the development of amoebic liver abscess, as occurs in Mexico City. The population of Sonora does not have those alleles and so they have a greater susceptibility to the disease. ALA presents more frequently in men10,11 between the ages of 30 and 50 years, with a ratio of 10:1. There are important case series reported in Mexico: In the Centro Médico Nacional Siglo XXI of the Instituto Mexicano del Seguro Social, Cuarón and Gordon12 conducted a multicenter study between 1963 and 1969 based on tomographic findings, gathering information on a total of 4,286 ALAs in 2,500 patients. Eighty-three percent of the cases had a single ALA and the remaining 17% presented with more than one lesion. Between 1968 and 1972, at the Instituto Mexicano del Seguro Social, 3,000 cases of hepatic amoebiasis were reported by Barroso,13 with 1,200 patients with ALA. The case series from the Hospital Juárez by Pérez-García and Zamora-Godínez14 in 1994 included studies on platelets and lymphocytes as outcome indicators of ALA. Another important series on ALA (1,128 patients) was conducted by Cerecero and Gaxiola15 in 1980 at the Hospital General de México, the same hospital center where a study was carried out in 1996 on ultrasound-guided evacuating puncture that included 160 patients.16 The number of cases of ALA since 2002 is unknown. A report of 48 cases, between 2005 and 2007, was conducted in the State of Sonora.7 ALA continues to be a health problem linked to poverty. One study found cases from 1.7 to 2.1% in patients hospitalized in general hospitals for very low-income persons, whereas in the registers of hospitalized patients in private hospitals, only 0.8% cases of ALA were found. Liver abscesses are usually treated with drugs, such as metronidazole, with a success rate of 90%.17 The contributions of Sigler et al.18 guided many surgeons in Mexico in the successful treatment of ALA. In recent years, percutaneous liver puncture19,20 has been considered the criterion standard of surgical treatment, more than 150 years after its implementation by the Mexican physician, Miguel. F. Jiménez, in 1856.
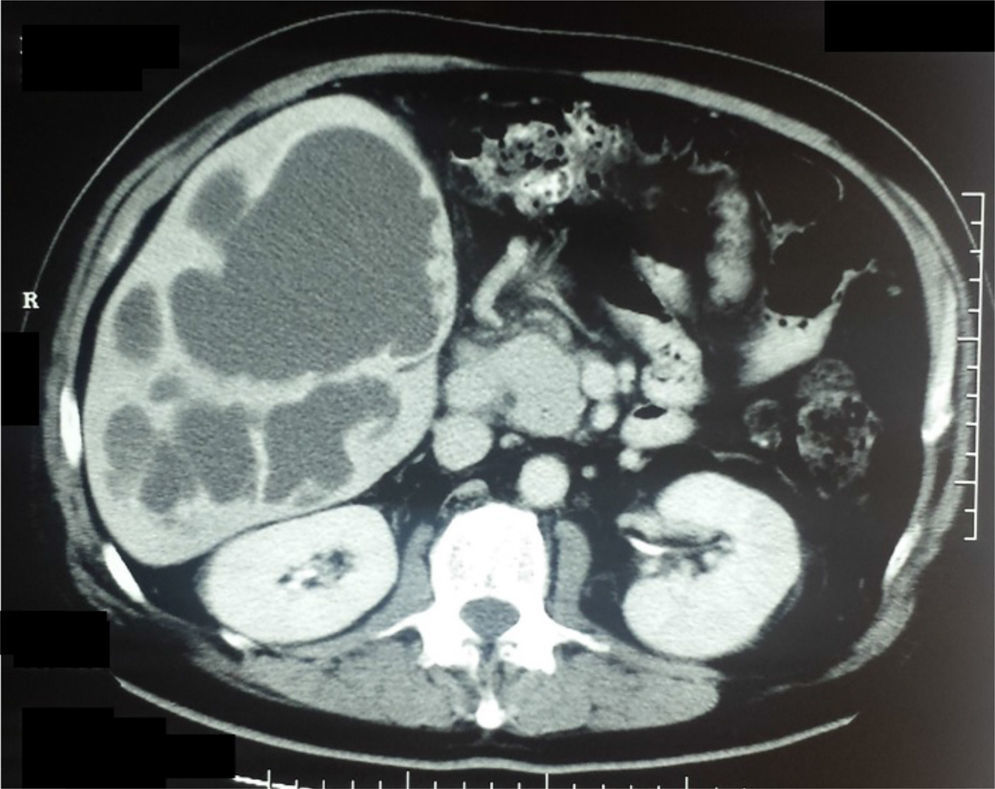
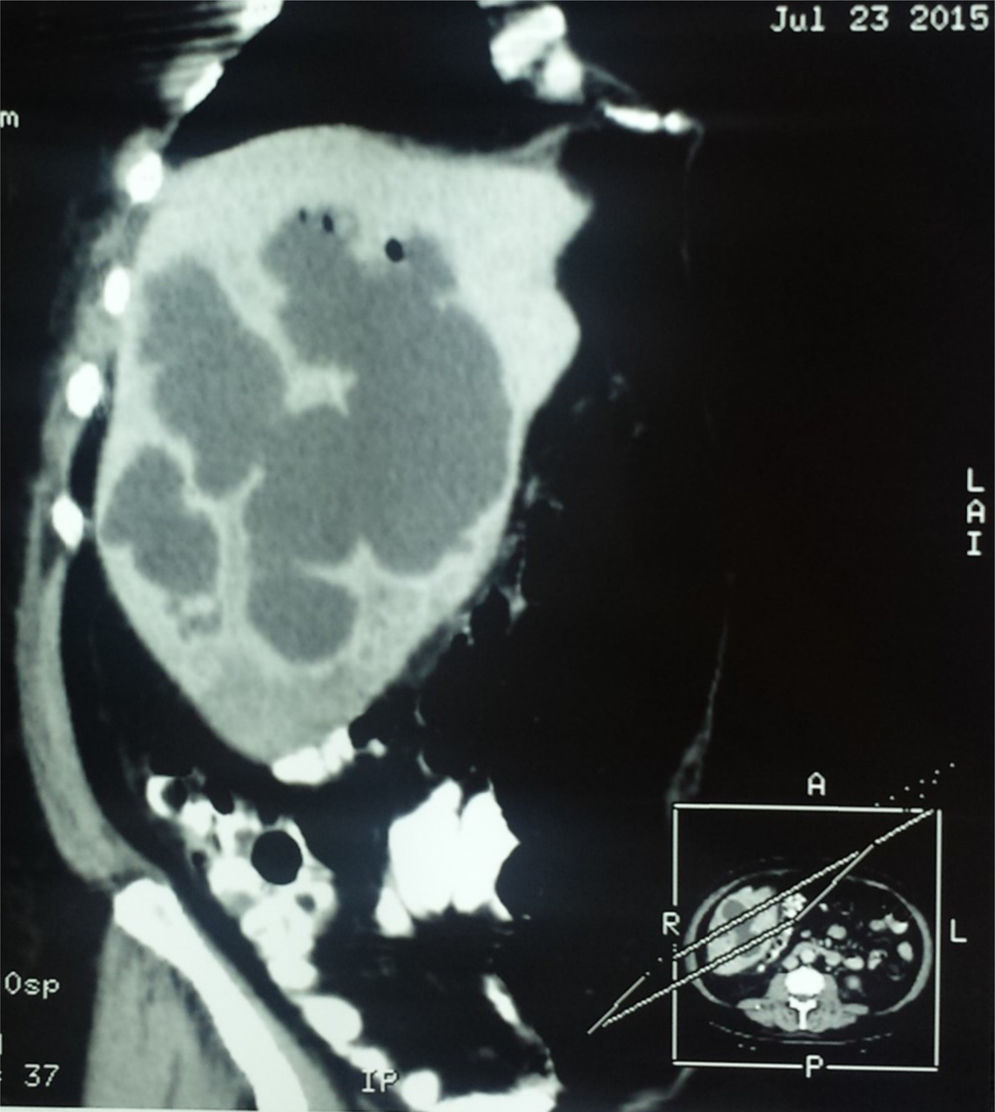
Clinical caseA 57-year-old man from San Luis de la Paz, Guanajuato, with a low socioeconomic level, had a 2-week progression of diarrhea with mucus and blood accompanied by straining and tenesmus, along with 10 days of fever and moderate-to-intense abdominal pain located at the right upper quadrant and irradiating to the right shoulder. Physical examination revealed: temperature of 39° C; heart rate of 100 beats/min; respiratory rate of 20 breaths/min; and blood pressure of 95/60mmHg. Peristalsis was present, there was pain in the right hypochondrium upon palpation, hepatomegaly of 4cm below the costal margin, and positive fist percussion in the hepatic area with no signs of peritoneal irritation. The patient was hospitalized with the clinical diagnosis of amoebic liver abscess. Abdominal ultrasound showed multiple cystic formations in the liver that were confirmed through contrast-enhanced abdominal tomography scan and scintigram (figs. 1 and 2). Blood cytometry reported leukocytes of 12,000 103/μl, with 78% neutrophilia, and a positive serologic latex agglutination test. Metronidazole was administered at a dose of 750mg 3 times/day for 10 days. The patient was released on the 12th day of hospitalization with no symptoms.
The book Bibliografía mexicana del absceso hepático by Dr. Raoul Fournier,21 published in 1956, contains an annotation by the physician and historian, Francisco Fernández del Castillo,22 relating the arrival in 1608 of the Archbishop of Mexico and future Viceroy of New Spain, Fray García Guerra, who died 6 months after being promoted to viceroy in 1611 (probably from an amoebic liver abscess). According to the chronicle in the words of Mateo Alemán, “He was suffering from a lack of animus, distress, and a bit of too much heat.” To get away from the hectic pace of the capital he sought refuge in Tacubaya, where he was treated by several physicians. Nevertheless, the fever, pain in the liver, and the fact that “that abscess having spontaneously corrupted itself from the inside” made it necessary one Sunday at four in the afternoon -the bull-fighting hour- to open His Grace, who survived only two weeks’. In the autopsy “they found, by the concave part of the tip of the liver, where it touches the ribs, half an egg's worth of putrid matter.”
One hundred seventy-eight years later, in 1790, the Royal Tribunal of the Protomedicato (Medical Board)23 called the physicians to an academic contest on “Inflammatory obstructions of the liver”. One of the awarded participants was Don Joaquín Pío Eguía y Muro, “professor of Vespers of Medicine at that Royal University, physician at the San Andrés General Hospital, and Proto-Attorney of the Tribunal of the Protomedicato”. Eguía speaks of “an epidemic of malignant bilious fevers” that in 1783 “made it impossible to explain the normal anatomy of the liver to the students of anatomic practice, because all the cadavers provided (seven) presented with this bloody entrail”.
The first mention of the existence of amoebas24 corresponds to Rösel von Rosenhof of Nuremberg, who in 1755 described what he called “the little Proteus”, alluding to the changing form of the cells. The name later given to amoebas comes from the Greek,
, amoibé, which means change.One hundred years later, one of Mexican medicine's contributions to surgical treatment of the liver abscess was made by the physician, Miguel F. Jiménez. In 1856, he began the puncture and cannulation of the liver abscess as an effective therapeutic procedure, thus reducing the mortality of this disease, whose causal agent would be known almost 20 years later.25
In chapter V of the Crónicas de la Medicina Mexicana,26 the following is written: “Dr. Jiménez made the fortunate decision to write down and publish his observations, research, and clinical lessons. His most well-known works are those on liver abscess. He described very complete clinical symptoms, according to the different locations of the abscess. He also described the complications and the method to cure the hepatic lesion through evacuating punctures”. The eminent Mexican physician, Miguel F. Jiménez, died on April 2, 1875.
One of the most paradoxical facts in the history of amoebiasis,27 a disease characteristic of countries with warm climates, is that it was first discovered in St. Petersburg (a city with temperatures below 7° C, three quarters of the year) by Dr. Fedor Aleksandrovich Lesh. In 1875, he attended to a patient from the Arkhangelsk district, close to the Arctic Circle. The patient had diarrhea, general malaise, and rectal discomfort. Upon examining the patient's stools, Lesh found numerous microscopic formations that he believed to be amoebas, due to their form and mobility. In his words, their microscopic appearance indicated that “they cannot be confused with anything, not even for a moment, that are not amoebic cells”. Microscopically, he described the presence of refractile nucleoli, or intranuclear bodies (rediscovered one hundred years later). In addition, in an experiment on 4 dogs, he infected them with the contaminated fecal matter from the patient with diarrhea and one became sick. This confirmed that the amoebas were capable of producing intense irritation that progressed to ulceration of the large intestine.
William Osler described the first case of amoebic liver abscess studied in the United States at the end of the nineteenth century. He found abundant amoebas in a 19-year-old physician who was a former resident of Panama, where he had suffered various episodes of dysentery ending in fever, general malaise, and pain in the area of the liver. The patient died April 5, 1890 and the article on his cause of death appeared in the Johns Hopkins Hospital bulletin the following month. After Osler's description, his disciples reported 15 cases of invasive amoebiasis at a hospital in Baltimore.
One year later, William Councilman published the monograph on the pathology of amoebiasis in which the terms “amoebic dysentery” and “amoebic liver abscess” were introduced. In addition to the description of the lesions produced by the parasite, he suggested that the human intestine could contain different species of amoeba, some pathogenic and some not.
The differentiation between Entamoeba coli (E. coli) and E. histolytica was begun in 1893 by two German physicians, Quincke (who introduced the lumbar puncture technique) and Roos, who discovered the cystic form of the amoeba. Fritz Schaudinn (the discoverer of Treponema pallidum) finally differentiated E. coli from E. histolytica. Schaudinn died at 35 years of age (another paradox) from complications of amoebiasis, resulting from self-experimentation with the pathogen. In 1909, Huber demonstrated that amoebas propagate from one host to another in the form of cysts.
In 1913, Walker and Sellards conducted one of the most important experiments of medical parasitology and knowledge of amoebiasis. With the help of Phillipino volunteers that were inmates in the Bilibid prison, they showed that E. coli was not capable of producing dysentery. Twenty prisoners were fed E. coli organisms, 17 became infected, and none of them became ill. E. histolytica was given to 20 other volunteers, 18 became infected, and only 4 of the 18 had dysentery. The experiment showed that the same organism could be a pathogen in some individuals and not cause disease in others. It also led to the conclusion that an asymptomatic carrier could transmit a pathogenic parasite to other individuals. The conditions under which Walker and Sellards carried out the experiments were striking. The following is their description of what is known today as informed consent: “The nature of the experiment, and the possibility of developing dysentery as a result of it, were carefully explained to each of the men in their native dialect and each one signed his agreement to the conditions of the experiment. No promises of immunity from prison discipline, commuted sentences, or financial reward were granted in exchange for volunteering”.
In 1925, the French parasitologist, Émile Brumpt, based on epidemiologic considerations, emphasized that the amoeba of cosmopolitan distribution was a non-pathogenic parasite that he named Entamoeba dispar (E. dispar), whereas the parasite located in certain tropical countries in which dysentery and liver abscess were frequent, was another amoeba, which he named Entamoeba dysenteriae, establishing the basis for the existence of 2 different species of amoeba, one that was a pathogen and the other that was not.
The life cycle of E. histolytica was described in 1928 by the English zoologist, Clifford Dobell.27
With respect to the initial treatment of amoebiasis, long before the arrival of the Europeans to the western edges of the Atlantic Ocean, ipecacuanha was used by the indigenous tribes to treat dysentery. At the beginning of the nineteenth century, Pelletier isolated emetine from the root of the ipecacuanha. However, it was Rogers, in 1912, who demonstrated its usefulness against the symptoms of amoebiasis. In the following years, a synthetic form of emetine was achieved that combined anti-amoebic effectiveness, with fewer adverse effects than those from the infusion prepared with the root of the plant. In 1955, Nakamura isolated azomycin (2-nitromidazole) from Streptomyces, and it demonstrated antimicrobial activity against Trichomonas vaginalis. Thus began the synthesis of drugs derived from nitroimidazoles. At the end of the 1950s, Cosar and Julou28 synthesized metronidazole, and in 1961,29 they reported their experiences in the management of trichomoniasis and amoebiasis. The work of Powell et al.30 in 1966 and Powell31 in 1971 confirmed the usefulness of metronidazole, modifying the treatment of amoebiasis and amoebic liver abscess worldwide. The year 1980 brought about the modification of the epidemiology of amoebiasis.
During the second half of the twentieth century, thanks to the insistence and perseverance of the distinguished Mexican physician, Bernardo Sepulveda, the Centro de Estudios sobre Amibiasis was founded in 1968, and included a myriad of Mexican medical scientists from the Universidad Nacional Autónoma de México, the Instituto Mexicano del Seguro Social, and the Secretaría de Salud, as well as from international agencies. It is impossible to mention them all, but the work of the following contributors must be highlighted: that of Sepulveda, himself;32,33 the experimental research of Pérez-Tamayo;34 the contributions of Escandón35 on the management of asymptomatic carriers; the research of Muñoz, described by Conde and De La Mora,36 on diagnostic methods; the work and experiences contained in the book by Martínez-Palomo;37–39 the contributions on epidemiology from Tanimoto40 and his indefatigable experiments on animals; and the vast number of historic information masterfully related by Gaxiola.41 Over the years, the efforts of the Centro de Estudios sobre Amibiasis resulted in: a) broad knowledge about the structure and physiology of E. histolytica, based on the axenic culture of the amoeba by Diamond and Harlow in 1961 and 1978 (culturing it without the presence of bacteria), enabling many aspects of the amoeba to be studied; b) knowledge of the mechanism of initial penetration into the tissues, carried out in animal models, as well as agglutination and its mechanism of action, cytotoxicity, phagocytosis, cytolysis, and the discovery of ionic channel forming-proteins, beta-N-glucuronidase, and chemotaxis inhibitors; c) knowledge of human immunology against amoebiasis; and d) the isolation and characterization of E. histolytica antigens, along with the equally important recognition by the World Health Organization (WHO) of amoebiasis as a worldwide health problem. Once again, we emphasize that this came about thanks to the unwavering dedication of Dr. Sepúlveda (from 1968 to 1984). To these contributions, we must add those of Stoopen in diagnostic imagining, made over a period of 20 years.42–45 In 1993, Clark and Diamond46 realized that amoebas isolated from sickened individuals were different from those in healthy individuals, due to their agglutination capacity with certain lectins that had specific isoenzyme patterns, antigenic differences, and differences in DNA, based on biochemical, immunologic, and genetic evidence. This fact enabled the scientific community to adopt E. dispar as a species that was distinct from, but morphologically identical to, E. histolytica, which was accepted by the WHO in 1997. In 2003, the prestigious New England Journal of Medicine dedicated a review article to amoebiasis,47 signifying that it continues to be a current theme. The technology of the present century has enabled the gene sequencing48 of an internationally recognized strain, E. histolytica HM1: IMSS (of Mexican origin), thus opening new fields for the study of this parasite. Nevertheless, amoebiasis continues to be a public health problem in many parts of the world, and even more so with the migration of large populations that is presently occurring in Europe. Perhaps the twenty-first century will provide the key to controlling poverty, which among many other concerns, is linked to amoebiasis.
Financial disclosureNo financial support was received in relation to this article.
Conflict of interestThe authors declare that there is no conflict of interest.
Please cite this article as: Arellano-Aguilar G, Marín-Santillán E, Castilla-Barajas JA, Bribiesca-Juárez MC, Domínguez-Carrillo LG. Breve historia del absceso hepático amebiano, con un caso ilustrativo. Revista de Gastroenterología de México. 2017;82:344–348.