Introduction
Inflammatory bowel disease (IBD) represents a wide spectrum of disease both macroscopically and microscopically, with classic Ulcerative Colitis (UC) and classic Crohn's disease (CD) at either end. However, there are cases located in the middle of the spectrum that constitute IC. Since Ashley Price in 1978 introduced the term "Indeterminate Colitis" (IC) to describe cases in which colonic resection had been conducted for chronic IBD where macroscopic and microscopic features were not sufficient to allow a definite diagnosis of either the classic type of Ulcerative Colitis (UC) or Crohn's disease (CD), others have reported this condition.[1-8] In recent years, the controversial and complex issue involving IBD classification has spurred medical debate and at the World Congress of Gastroenterology in Montreal in 2005 a working party decided that the IC diagnosis should be made only after colectomy, and the term "inflammatory bowel disease unclassified" should be used in all other cases where definitive features of CD and UC are absent.9,10
Macroscopically, the affected colon and rectum in IC demonstrates an extensive colitis, severe continuous disease throughout the colon often with relative rectal sparing, and intermittent ulceration. The mucosa between these ulcers may appear normal, and fissures may also be seen macroscopically.11-13 Microscopically IC shows myocitolisis, telangiectasia and some fissuring.
The histological diagnosis of the colectomy specimen is imperative for subsequent management. If UC is present, then ileal pouch anal anastomosis (IPAA) is performed, whilst in CD this is usually contraindicated due to the increased risk of complications.
Epidemiological data from some series have reported that IC is diagnosed in between 9% and 20% of colectomy specimens, although some studies report only 5%.14 Among the IC cases diagnosed, most patients will eventually be reclassified as either UC or CD.7,15,16 and of those, more than 80% will behave like UC while only between 1% and 15% of IC patients are ultimately diagnosed as CD.17-19
Since there are no Latin-American studies that can establish IC epidemiological data, our aim was to determine the frequency of IC in Mexican patients from a tertiary care-center hospital and to describe its frequency and clinical features.
Patients and Methods
We carried out a retrospective database analysis of all patients diagnosed with IBD who underwent total colectomy between 1990 and 2006. We analyzed demographic data as well as clinical, laboratory, endoscopic and histopathological variables relating to the 86 patients who underwent total colectomy.
For the demographic data, age, gender, race and age at diagnosis were considered. The following clinical features were included: a family history of IBD, autoimmune concomitant diseases, smoking, extra-intestinal manifestations, extent, course of disease, response to treatment and indication for surgery. The histopathological findings before and after colectomy were considered to compare the initial diagnosis with the final outcome.
The diagnosis of IBD was based on well-established clinical, endoscopic and histopathological diagnostic criteria before the total colectomy. The Truelove and Witts activity index was used for evaluating disease severity in the UC patients.
The final diagnosis of UC was based on clinical, laboratory, full endoscopic and histological findings. In relation to CD, diagnosis was based on clinical, ileoscopic, radiological (small bowel series) or histological findings.
After colectomy, the pathological specimen was analyzed and a diagnosis was established. All the specimens were analyzed by two pathologists and after agreement they made a final diagnosis. In order to determine the final IC diagnosis, certain histopathological criteria were required which included macroscopic colitis and/or microscopic abnormalities including severe ulceration, with non-specific transmural inflammation, foci of myocytolysis, presence of islands of surviving mucosa with inflammation, and a regular glandular pattern and mucin preservation, or fissures that did not share characteristics with the ones seen in CD, and absence of granulomas.
Patients with IC were diagnosed according to the pathological features observed in the colectomy specimen that failed to meet diagnostic criteria for either CD or UC. 20-24
Descriptive statistics were expressed as mean and standard deviation (SD). Data were analyzed by non-parametric and parametric tests. A p value < 0.05 was considered statistically significant. All statistical analyses were performed with SSPS Version 14.0.
Results
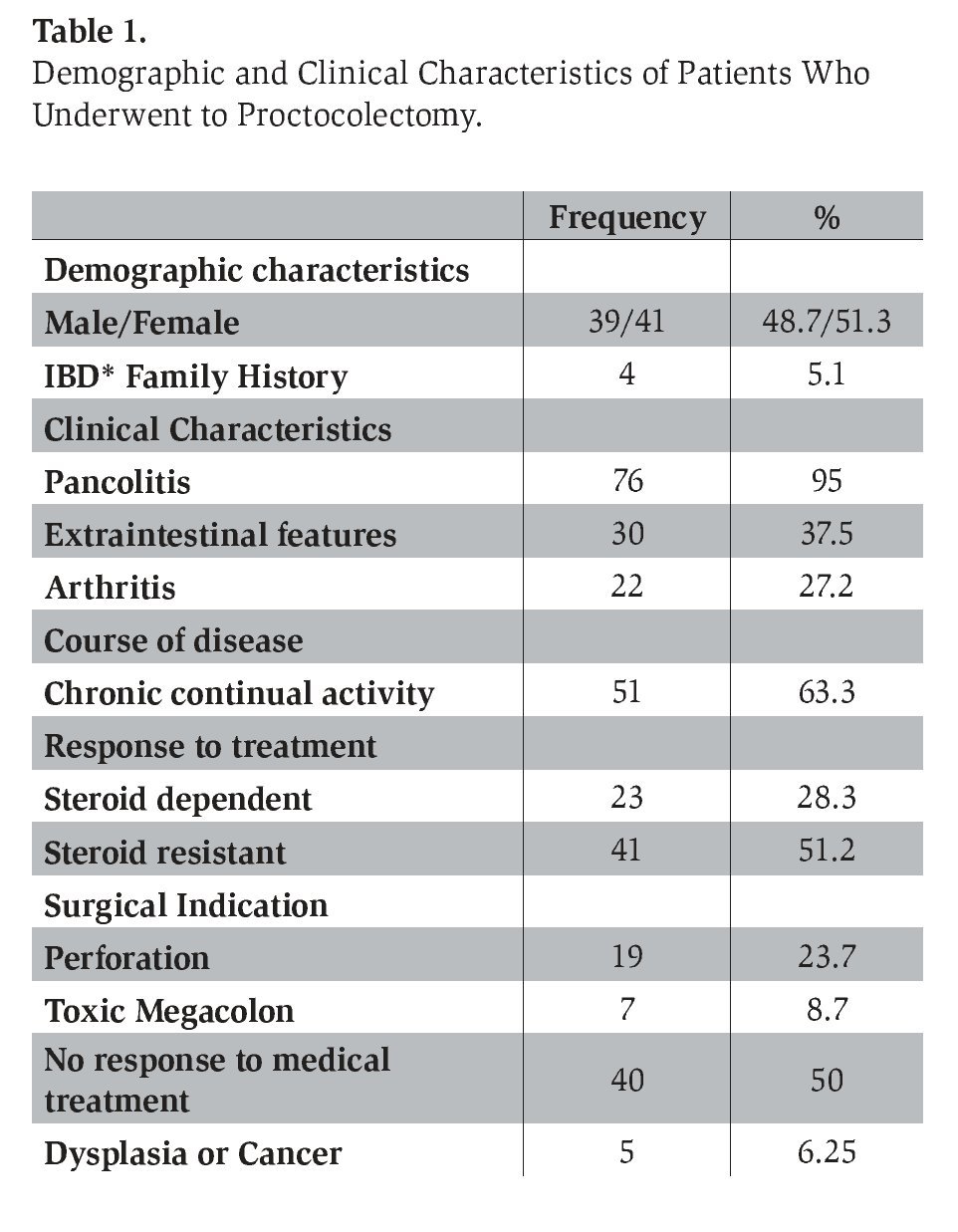
Of the 86 IBD patients who underwent total colectomy, 80 had all the data and criteria necessary for the analysis. Six patients were excluded because the clinical records were incomplete, or because some of them had the surgery at another medical center. In total, we analyzed 80 patients (39 male, 41 female), with a mean age of 44.8+13 years, all of whom had a mestizo or racially mixed Mexican ethnic background. No statistical difference was found between the subgroup of patients with IBD in terms of gender. Preoperatively all of these patients had been clinically diagnosed with UC. Following total colectomy, among the specimens analyzed by the pathologists who gave the final diagnosis, we found that among the 80 specimens, 71 (88.7%) were confirmed to be UC, 2 were CD (2.5%) and 7 (8.7%) were IC. Those patients diagnosed with IC were significantly younger than the other patients, with a mean age at diagnosis of 27+4.8 years old.
In the entire group, family history of IBD was found only in 4 patients (5.1%). We found that smoking was present in 21 (26.2%) patients. In relation to clinical characteristics, pancolitis was found in 76 (95%) of these patients. Extraintestinal manifestations (EMs) were present in 30 (37.5%) patients and displayed a wide range of different features. Arthritis was the most frequent EM occurring in 22 (27.2%) patients, followed by sacroiliitis in 3 (3.75%) patients, primary sclerosing cholangitis, pyoderma gangrenosum and erythema nodosum in 2 patients (2.5%), and uveitis as well as ankylosing spondylitis in 2 patients (2.5%). Thromboembolic events were found in only 5 (6.2%) patients. With regard to the clinical course of disease prior to the surgical treatment, we found 51 (63.7%) with chronic continual activity, 20 (25%) with severe intermittent activity and 7 (8.7%) with mild intermittent activity but who underwent surgery because dysplasia or cancer was found. With regard to medical treatment before colectomy, 23(28.75%) were steroid-dependent and 41 (51.2%) steroid-resistant, (most were receiving standard steroid dosage regimens), 9 (11.2%) were azathioprine resistant and one (1.2%) was intolerant to immune modulator agents. Forty-one patients were on treatment with immunomodulators at the time of surgery; none of the patients received treatment with cyclosporine.
Analysis of surgical indications found that non-response to medical treatment was the most frequent indication for surgery in 40 (50%) patients, followed by perforation in 19 (23.7%) patients, toxic megacolon in 7 (8.7%) patients, dysplasia or cancer in 5 (6.25%) patients, uncontrollable bleeding in 3 (3.75%) patients, and 4 (5%) patients had other surgical indications (Table 1).
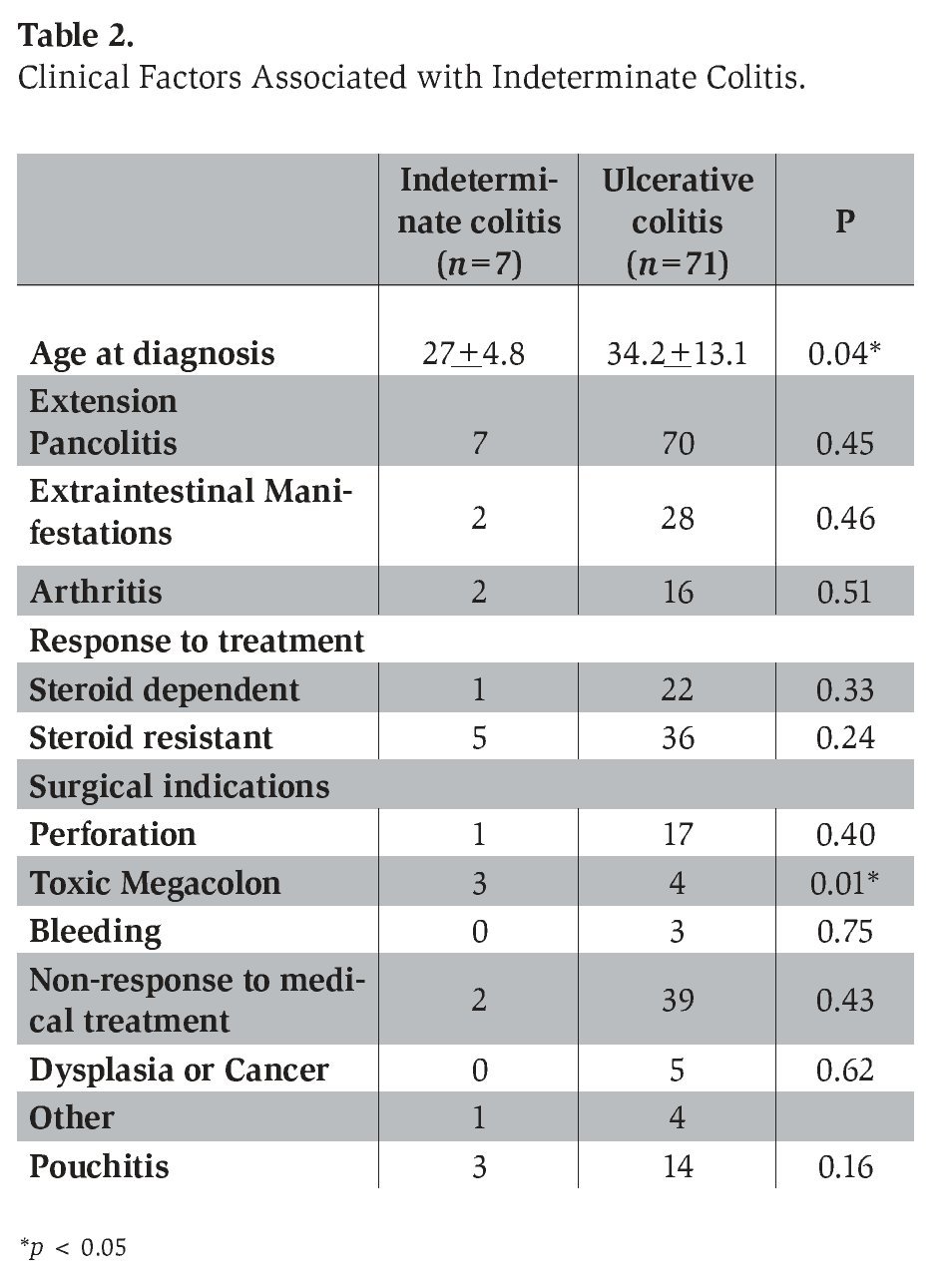
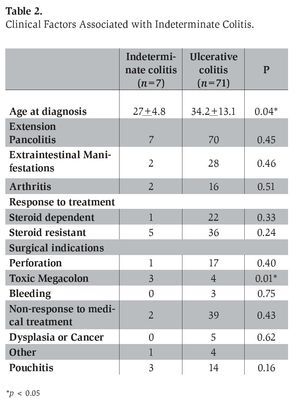
During the subgroup analysis of the IC and UC patients, several demographic and clinical characteristics were analyzed. Among the 80 patients, 78 had an initial diagnosis of UC, while 2 were diagnosed with CD. Seven patients were reclassified as having IC after total colectomy; all of them had an initial diagnosis of UC (3 male, 4 female). The mean age 27.0+ 4.8 years at diagnosis for patients with IC was significantly lower compared to 34.2+13.2 years for patients with UC (Table 2). All 7 patients with IC had pancolitis, 5 (71%) had a chronic continual activity and 2 (28.5%) had severe intermittent activity. With regard to the response to medical treatment, 5 (71.4%) were steroid resistant, 1 (14.2%) was steroid dependent, and 1 (14.2%) was immunomodulator resistant. Only 2 (28.5%) of the IC patients had arthritis as an extra-intestinal manifestation. When examining indications for the total colectomy in the IC subgroup, we found that 3 (42.8%) were diagnosed with toxic megacolon, 2 (28.5%) were unresponsive to medical treatment and 1 (14.2%) had a colonic perforation. None of the IC patients had dysplasia or cancer as a surgical indication. Of all the clinical variables analyzed, we found no significant association with any of the variables and IC except for the presence of toxic megacolon as a surgical indication (p=0.01; OR 12.72, CI 95% 1.56-27.75) and the younger age of onset (p=0.04; CI 95% -2.8 -17.3).
The morphological macroscopic features observed in IC patients were the presence of extensive ulceration and the disease affecting >50% of the mucosal surface of the entire colon. The microscopic findings seen in IC patients were extensive ulceration with sharp transition to normal adjacent mucosa, transmural lymphoid inflammation, absence of well-defined epitheloid granulomas and multiple squat V-shaped ulcers.
The morbility of all patients who underwent colectomy was 55%, most of the patients had abdominal sepsis and the mortality was 0%.
Discussion
In the present study, IC was found in 7/80 patients (8.7%) Mexican patients with IBD who underwent total colectomy between 1990 and 2006. In spite of the fact that the UC and IC prevalence is higher in Caucasian populations (between 5% and 20% of colon specimens).14,15,23 we found an IC frequency comparable to that reported in other populations.
In some retrospective studies.15 IC accounted for 5-6% of all initial diagnoses, but the prevalence of IC diagnosed preoperatively may increase or decrease after surgery and evaluation of the colon specimen. Price.7 reclassified 15 cases of IC after reviewing pre-colectomy biopsies. If reclassification of IC is supported by evidence derived from clinical symptoms, and pathological examination of endoscopic pre-colectomy and post-colectomy biopsies, IC may be a provisional diagnosis. In our study we found that among 80 patients with an initial diagnosis of UC, 7 had their diagnosis reclassified to IC. This substantiates the observation that despite a clinical diagnosis of UC supported by pre-colectomy biopsies, the final diagnosis may change after subsequent examination of colectomy specimens and with patient follow up.
Among those diagnosed with IC, nearly 66% to 80% of patients will be eventually reclassified as either UC or CD.7,15,16 and of these, more than 80% will behave clinically like UC especially if there were no features that could have suggested CD before surgery. In major series only between 1% and 15% of IC patients are ultimately diagnosed as CD.17,19 While 2 patients in our series were reclassified as having CD following colectomy, we do not have sufficient follow-up information of our IC patients to assess the ultimate clinical behavior of their IBD.
Validation of the reclassification to IC taken from colectomy results is possible when follow up of this subgroup is conducted, especially in pediatric groups, and clinical outcome is evaluated. Carvalho et al.24 reported in a retrospective analysis that 25 of their patients with an initial diagnosis of IC were reclassified to either CD (n=16) or UC (n=9) after a median follow-up of 1.9 years. Other studies also show two thirds of cases of IC diagnosed at colectomy and were eventually reclassified as UC or CD, and of these more than 80% will behave as UC. It seems clinically important to distinguish IC as a separate entity because the higher incidence of some complications and different natural history of disease may require therapeutic decisions different from the ones made for UC or CD. If we consider that IC really is a provisional diagnosis, our 7 cases of IC may be reclassified in time. But at the moment, we have to maintain the present diagnosis and try to identify unique clinical features that vary from the other two classic presentations of IBD. Thus we will be able to gain further information about this disease's clinical behavior.
Because of the design of this study, it was not our goal to follow up our cases though it would be interesting to look into the outcome and changes that have developed since surgery and, if necessary, reclassify any cases. A future complementary paper describing the longer-term clinical outcome of our patients is needed in order to establish a final diagnosis
Price emphasized the difficulty to differentiate between UC and CD when the colectomy was performed as an emergency procedure, where macroscopic and microscopic features of both CD and UC remain blurred with few distinguishing features, and where the pathological assessment difficulties are mainly due to the severity of the inflammation.7,8 This may be due to the fact that the pathological features of UC and CD are often seen to overlap in the acute phase of disease.
Most of our procedures were performed under emergency circumstances and though there might be a chance this affected histological interpretation, generally the histopathological features fit the criteria mentioned above, so the pathologists could come out with an ultimate diagnosis.
In some studies comparing IC and UC patients, those undergoing IPAAs showed a low rate of complications in UC, compared with a higher complication and pouch failure rates in IC.21,25-29 The frequency of severe pouch complications overall in IC appears to be 20%, intermediate between UC (8-10%) and CD (30-40%).30 The failure rate in IC has been reported as higher than in UC (19% vs. 8%).
To our knowledge, this is the first Latin-American study of IC based on histopathological characteristics of colectomy specimens examined by consensus criteria.9,10 Since IBD is not a very frequent disease in developing countries, the presence of IC may be underestimated, in contrast to European medical centers where IBD is more common and there is a greater diagnostic awareness of the condition. In our series there was a significant association between toxic megacolon as well as young age at diagnosis and IC which might provide clinical clues to improve it being detected in patients in Latin America.
In summary, as established by consensus criteria, colon specimens are the ultimate medical guideline for the histological classification of IBD. The prevalence of IC diagnosed preoperatively may increase or decrease after surgery and evaluation of the colectomy specimen. The diagnosis of IC made from a colon specimen in an individual patient may remain as the clinical diagnosis indefinitely, or it may change to UC or CD with further clinical evidence during follow up. The ultimate clinical diagnosis of IC patients may be based on follow-up investigations and clinical events that enable them to be reclassified into UC or CD.
In conclusion, the prevalence of IC was 8.7% in our series of patients undergoing colectomy for IBD. The clinical features associated with this condition were earlier age at diagnosis and toxic megacolon.
Correspondence author: Prof. Jesús K.
Yamamoto-Furusho M.D., Ph.D. Head of IBD Clinic, Department of Gastroenterology, Instituto Nacional de Ciencias Médicas y Nutrición Salvador Zubirán. Vasco de Quiroga 15 colonia Sección XVI, Tlalpan, CP 14000, México.
Telephone: (52) 55 55733418 ext. 2705-15. Fax: (52)5556550942.
E mail: kazuofurusho@hotmail.com