¿ The Case for Recommending Surgery for Polypoid Lesions of the Gallbladder ≥ 8 mm
Pros
The natural history of polypoid lesions of the gallbladder (PLG) is not completely understood, because most available studies are necessarily retrospective. Although most polyps are benign and asymptomatic, some early gallbladder carcinomas will become evident as symptomatic polypoid lesions. Traditionally, the characteristics of the polyp associated with an increased risk of malignancy include diameter greater than 10 mm, patient age greater than 50 years, presence of concomitant gallstones, solitary lesions, sessile polyp, presence of symptoms and rapid change in size on serial ultrasonography (US), however, there are no definitive criteria identified.1 The advances in resolution and the broader use of modern imaging methods have enabled the detection of smaller PLG. However, despite new technology like endoscopic ultrasonography, it remains difficult and often impossible to differentiate neoplastic from nonneoplastic PLG solely by depending on imaging studies, especially when polyps are smaller than 10 mm.2 Moreover, US is highly operator-dependent and may over or underestimate polyp diameter, making size assessments difficult to compare between examinations particularly when performed with low-end equipment or by non-radiologists.
Some studies have shed light on the clinical importance of small polyps. Kubota et al. reported that 12% of gallbladder cancers and 75% of the adenomas removed had a diameter of less than 10 mm.3 Ishikawa et al. conducted a study on 97 patients with surgically resected PLG in an attempt to determine both the shape and diameter of the polypoid lesions associated with malignancy. Foci of carcinoma were noted in 9 (13%) of the 67 pedunculated lesions and in 10 (33%) of the 30 sessile lesions. Sessile polyps harboring carcinoma averaged 14 ± 4 mm (8 - 20 mm) in maximum diameter Cancer invasion extended beyond the muscular layer in 2 of the polyps that were )10 mm in diameter.4
Recent observations have challenged the classic criterion of using a cut-off value of 10 mm to recommend cholecystectomy in asymptomatic PLGs. Zielinski et al. reviewed retrospectively 130 patients who had PLGs found on US and subsequently underwent cholecystectomy. While obviously a selected population of patients was analyzed in this study, they all underwent cholecystectomy. This study did identify several risk factors that increased the likelihood for malignancy: a history of primary sclerosing cholangitis (PSC), evidence on imaging of either local invasion or increased vascularity, and a maximum diameter of ≥6 mm based on the pre-operative US. Furthermore, 7.4% of PLGs ≤ 10 mm were neoplastic. The positive predictive value (PPV) and negative predictive value (NPV) for diagnosing neoplastic changes on US based on a cut-off value of ≥ 10 mm were 28.5% and 93.1%, respectively, with a false negative rate of 5.0%. Using a cut-off of ≥ 6 mm changed the positive predictive and negative predictive values to 18.5% and 100%, respectively, but now with a false negative rate of 0%.5 Park et al. followed 1558 patients with PLG, 71% for more than one year, and found 33(2.1%) with neoplastic polyps. While PLG ≥ 10 mm had 24.2 times greater risk of malignancy than PLG < 10 mm, 15 of 33 neoplastic polyps (46%) were < 10 mm. When the size cut-off point was set at 10 mm, sensitivity and specificity of predicting neoplastic polyps were 54.5% and 94.1% respectively, but when it was decreased to 8 mm, the sensitivity increased to 63.6% while the specificity decreased to 85.9%. The number of neoplastic polyps that would have been overlooked when the size criterion was set at 8 and 10 mm were 12 (36%) and 15 (46%) of 33.6
These observations show that a substantial and clinically relevant number of small PLG are neoplastic, have a very real risk of malignancy and thus require a careful and potentially costly long-term follow-up. Indeed, evidence based recommendations for surveillance are undefined in terms of frequency and type of imaging. Setting a cut-off value of 3 10 mm cannot exclude neoplastic polyps completely and risks missing some early cancers. Decreasing the threshold to recommend surgery for PLG to 3 8 mm should be considered seriously given the current very low morbidity of laparoscopic cholecystectomy, the high lethality of gallbladder cancer, the lack of diagnostic accuracy of current imaging techniques, and the costs of surveillance imaging.
Dr. Antonio Ramos-De la Medina
Departamento de Cirugía
Hospital Regional de Alta Especialidad de Veracruz. Veracruz, México.
ramos.antonio@inbox.com
¿ Selective Cholecystectomy for Gallbladder Polyps: The Case for Observing Polyps Less Than 1 cm
Cons
Gallbladder cancer is a malignancy associated with an extraordinarily poor survival when advanced.7 It is also known that some polypoid lesions of the gallbladder may be early cancers, or are adenomas that may degenerate into frank malignancies. This has led some to advocate resection of all incidentally discovered gallbladder polyps, no matter how small. Given that many patients get imaging for the slightest of abdominal disturbances, many more gallbladder lesions less than 1 cm are being discovered than ever before. One must be judicious about treating all incidentally discovered small lesions because unnecessary surgery can still cause complications.
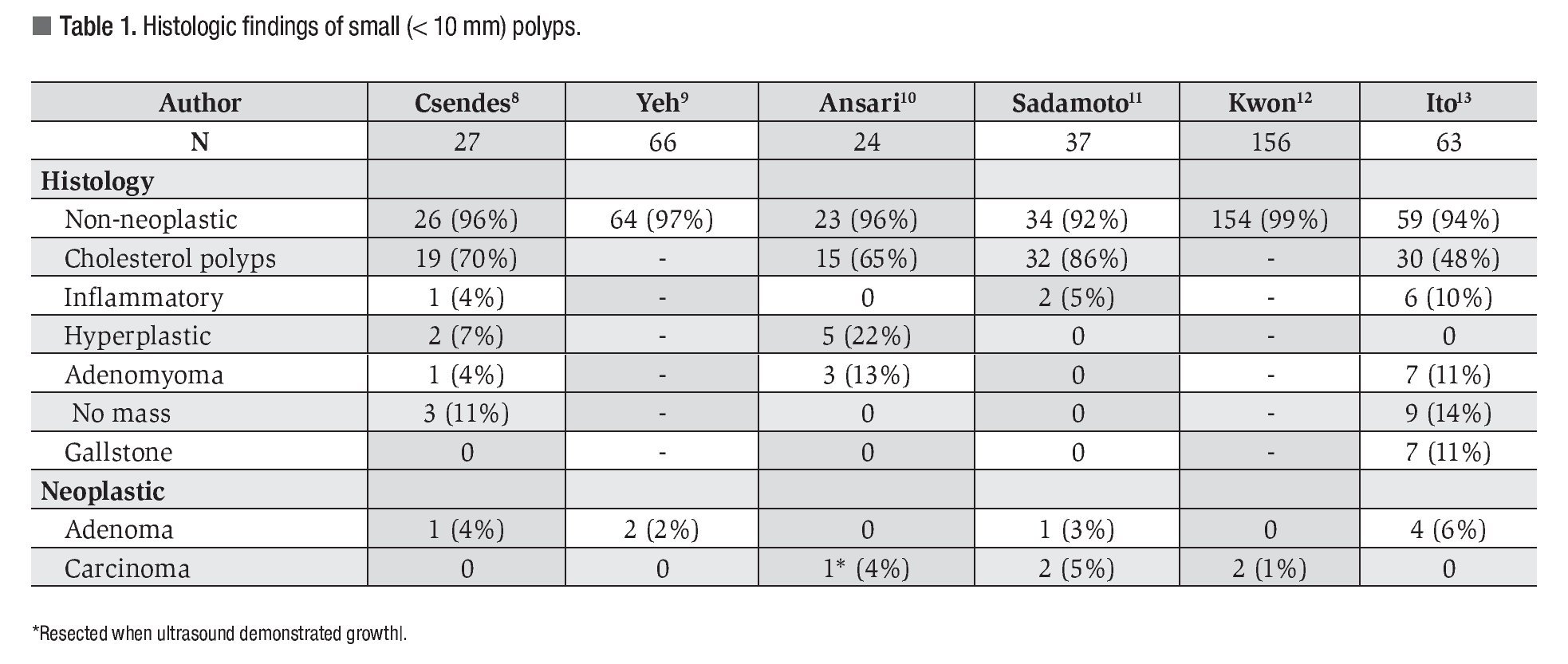
There are many types of benign small lesions of the gallbladder. They include cholesterosis, submucosal abscesses, gallbladder diverticuli, small inspisated stones, inflammatory polyps, and adenomyomata. Benign lesions of the gallbladder are much more common than the 2000 gallbladder cancers seen in this country every year, or the 3000 or so adenomatous polyps. Table 1 summarizes the recent literature examining small (< 1 cm) solid lesions of the gallbladder.8-13 Overall, 96% of small lesions turn out to be non-neoplastic. Only 1% turn out to be cancer and 2% to be adenomas. Thus, surgery for small mucosal lesions in the gallbladder is much more likely to remove a benign lesion than a malignant one.
The risk of anesthesia, infection, and bile duct injury are the same for a cholecystectomy for benign disease as for malignant or premalignant disease. In the age of laparoscopic cholecystectomy, gallbladder polyps are more likely to be resected. Yeh et al. reported on 123 patients with gallbladder polyps who underwent laparoscopic cholecystectomy.9 No lesion less than 1.5 cm was found to be cancer. Only 2 of 66 lesions less than 1.0 cm (2.1%) were found to be adenomas.
Many follow-up studies have demonstrated that small polypoid lesions of the gallbladder are unlikely to be cancer and do not progress to cancer during follow-up. Csendes et al. reported on 111 patients with polypoid lesions less than 10 mm. Twenty-seven underwent cholecystectomy, and none had cancer.8 The others were followed for a mean time of 71 months, and none developed cancer. Moriguchi et al. reported on a series of 109 asymptomatic gallbladder polyps followed for 6 years by ultrasound. Of these, 88 percent did not change in size. No cases of cancer were found.14 Ansari S reported on a series of 57 patients with polypoid lesions of the gallbladder. In this group, 50 had lesions less than 10 mm in size10 Of these, 24 underwent cholecystectomy, and one was found to have cancer. Twenty-six patients have undergone long-term follow-up with no further case of cancer discovered. Of note, the single patient with discovery of cancer underwent cholecystectomy because follow-up with ultrasound demonstrated growth within 6 months.
In our own series from Memorial Sloan-Kettering Cancer Center of 63 polyps less than 1 cm, only 4 were found to be adenomas.13 None were found to be cancer. Of 143 patients with asymptomatic gall-bladder polyps followed for a median of 17 months (1 to 81 months), growth was observed in only 6%. No development of cancer has been found.
Some investigators have argued the use of clinical criteria, in addition to small size, for selection of patients for follow-up. Kwon et al., in their report on 158 small polyps, suggested a clinical scoring system12 In this series, only 2 of the 158 small polyps (1.3%) were found to be cancerous. These investigators proposed a scoring system using 1) age > 60 years, 2) sessile morphology, and 3) size > 10 mm as predictive for cancer. None of their 115 patients with 0 criteria had cancer.12
Other investigators have recommended scoring systems based on imaging criteria. Since small polypoid lesions of the gallbladder are often not seen on computed tomography or magnetic resonance imaging, such proposed scoring systems are usually based on ultrasound or endoscopic ultrasound (EUS). Sadamoto et al. suggested one such scoring system in their paper examining the utility of EUS for assessing gallbladder polyps.11 They proposed a system for predicting neoplastic lesion utilizing 1) size, 2) homogeneity, and 3) echogenicity. Larger polyps, with heterogeneous echogenicity, and which are hypo-echoic are worrisome for cancer.11
Furthermore, small gallbladder cancers have a low likelihood of metastases.15,16 This is the reason that the long-term cure rate for T1 gallbladder cancer by simple cholecystectomy is above 95%, and as high as 100% in some series. Thus, a short observation period to detect further lesion growth as a characteristic indicative of cancer is unlikely to miss the window of opportunity for curative resection.
Thus, we should be judicious in surgical treatment for small, asymptomatic gallbladder lesions. Observation is the best course. Growth would be a good indication for therapy. Most incidentally discovered lesions are benign and do not need treatment. The few lesions that turn out to be neoplastic are unlikely to progress to unresec-table or incurable under close observation. This measured approach will prevent unnecessary morbidity while providing the best care possible for the patients. Unnecessary surgery, no matter how safe, is unnecessary.
Yuman Fong, MD
Murray F. Brennan Chair in Surgery Memorial Sloan-Kettering Cancer Center 1275 York Avenue, C887
New York, New York 10065
212-639-2016 fongy@mskcc.org
¿ Gallbladder Polyps: What Size Should Stimulate Cholecystectomy?
The balance
Doctors Fong and Ramos-De la Medina have each offered cogent arguments in support of their individual contention that polyps of > 1 cm and > 0.8 cm, respectively, should be treated by cholecystectomy. So... who is correct? Or, are they both correct? Most all biliary surgeons agree that gall-bladder polyps > 1 cm should initiate cholecystectomy, even in the asymptomatic patient (and especially so if the patient is > 60 years old, they are symptomatic, or if the polyp is sessile). So then why quibble about the difference between 8 and 10 mm, i.e. a 2 mm difference? The answer lies in the dismal outlook for most any patient with a gallbladder carcinoma extending through the submucosa to involve the muscle of the gallbladder wall as well described by both Drs. Fong and Ramos-De la Medina.
Actually, both authors are correct and, in my opinion, the factors deciding the decision making include the risk of cholecystectomy, costs (to individual vs. to society), quality-adjusted life years (QALY), the cost of future surveillance imaging, possibility of emotional turmoil, and ultimately possibly the financial feasibility in the country in which the patient lives.
Risk of cholecystectomy: In an otherwise healthy patient, serious morbidity after laparoscopic cholecystectomy is exceedingly small (< 1%); likewise, the convalescence is exceedingly short (days). In contrast, in patients with serious co-morbidity (cardiac, pulmonary) or those in whom a minimally invasive approach is unlikely (less and less common currently), then cholecystectomy for polyps < 1 cm probably should be evaluated as per Dr. Fong's approach.
Costs: Financial considerations must be acknowledged. In countries where the budget for health care is limited, elective cholecystectomy for an 8 mm or 9 mm gallbladder polyp is probably ludicrous; the amount of money expended for such a low-yield, prophylactic cholecystectomy would be better used elsewhere. For the financially privileged, if they can afford it - so be it. This argument may very well differ between countries and possibly within social strata within countries!
QALYs: Clearly, this concept is a value judgment and also may vary with society and the national health care budgets. How much is life worth? -A VALUE JUDGMENT that may vary with social strata, personal finances, and personal opinion-provided you can afford to pay for the service (not everyone drives a Mercedes - unless you can afford it personally).
Surveillance imaging: As with the financial considerations to the health care budget, the cost of surveillance may weigh into the equation. Routine? Yearly or biennial in a 40-year-old patient will be expensive. Moreover, the appropriate algorithm for surveillance is not defined.
Emotional turmoil: In some people, the extreme worry about the potential risk of a "malignancy" may outweigh the risks/costs of a safe laparoscopic cholecystectomy. There are cancer-o-phobes, we have all met them—prophylactic cholecystectomy is indicated or they will drive you, their family, and/or themselves literally crazy!
Predisposition to gallbladder cancer: The country of origin should weigh into the decision making. Chile, Japan, and Northern India have an inordinately greater incidence of gallbladder cancer that occurs at an earlier age, even in the absence of gallstones. Similarly, in patients with sclerosing cholangitis, the risk of gallbladder cancer is increased markedly. In these patients, cholecystectomy is warranted.
In summary: "prophylactic" cholecystectomy for the 8 mm to 10 mm asymptomatic gallbladder polyp requires consideration of the risk of operative cholecystectomy, national vs. personal costs, the subjective worth of QALYS (provided the patient can afford it!), estimated cost of long-term surveillance, possibility of emotional turmoil/worry of cancer, and other environmental (demographic) and predisposing factors. All these considerations need to be weighed in the decision-making process of the art of surgery; indeed, sometimes the best surgical practice is nonoperative.
Michael G. Sarr, MD
James C. Masson Professor of Surgery Mayo Clinic, Rochester, MN USA