Achalasia is characterized by the absence of lower esophageal sphincter relaxation and esophageal aperistalsis. Diagnosis is confirmed through high-resolution esophageal manometry. Laparoscopic myotomy is the standard treatment, but peroral endoscopic myotomy (POEM) is a safe and effective alternative, with good short-term and medium-term results. Our aim was to describe the short-term and medium-term experience with POEM at a tertiary care center.
Materials and methodsThe study was conducted within the time frame of November 2014 and February 2017. Treatment-naïve achalasia patients and previously-treated achalasia patients that were candidates for POEM were included. A protocolized 24-month follow-up was carried out.
ResultsFifty procedures were included and 31 (68%) were performed on women. Forty-one (82%) of the procedures were carried out on previously untreated patients, 7 (14%) were performed on previously treated patients, and 2 (4%) of the patients had redo-POEM. The mean age of the patients was 48.8±14.1 years. The pre-POEM Eckardt score was 9 and the integrated relaxation pressure was 24.4mmHg. Sixty-eight percent of the patients had type ii achalasia. Procedure time was 80min and myotomy length was 12.6cm. Hospital stay was 3 days and subcutaneous emphysema was the most common adverse event (30%). A total of 22/50 (44%) patients reached the 24-month follow-up, maintaining the Eckardt score and the decrease in the integrated relaxation pressure. There were no deaths. A total of 47.5% of the patients had a positive pH-study at 6 months, 15% had clinical reflux, and 35% presented with mild esophagitis. All the patients were adequately controlled with proton pump inhibitors.
ConclusionPOEM is safe and effective in the short term and medium term for the treatment of achalasia and other esophageal motor disorders in Mexican patients.
La acalasia se caracteriza por una ausencia de relajación del esfínter esofágico inferior y aperistalsis esofágica. La manometría esofágica de alta resolución) confirma el diagnóstico. La miotomía laparoscópica es el estándar de tratamiento, pero la miotomía endoscópica peroral (POEM) representa una alternativa segura, efectiva y con buenos resultados a corto y mediano plazo. Nuestro objetivo es describir la experiencia de la POEM en un centro de referencia de tercer nivel en México a corto y mediano plazo.
Material y métodosEstudio realizado entre noviembre 2014 y febrero 2017. Se incluyeron pacientes con acalasia vírgenes y postratados, candidatos a POEM. Se realizó un seguimiento hasta 24 meses de forma protocolizada.
ResultadosSe incluyeron 50 procedimientos, edad de 48.8±14.1 años, mujeres 31 (68%), vírgenes 41 (82%), postratados 7 (14%) y redo-POEM 2 (4%). El puntaje Eckardt y la presión de relajación integrada pre-POEM fueron 9 y 24.4mmHg respectivamente. La acalasia fue tipo ii en el 68%. Tiempo del procedimiento 80min y miotomía de 12.6cm. Estancia intrahospitalaria de 3 días, el enfisema subcutáneo fue el evento adverso más común (30%). Veintidós de 50 (44%) alcanzaron 24 meses, observando un mantenimiento del Eckardt y disminución en la presión de relajación integrada. No se presentó ninguna muerte. La pHmetría fue positiva en el 47.5% a los 6 meses, hubo reflujo clínico en el 15% y esofagitis leve en el 35%, que fueron adecuadamente controlados con inhibidor de bomba de protones.
ConclusiónLa POEM es una técnica segura y efectiva para el tratamiento de pacientes mexicanos con acalasia y otros trastornos motores del esófago a corto y mediano plazo.
Achalasia is a primary motor disorder of the esophagus characterized by failure of relaxation of the lower esophageal sphincter (LES), combined with esophageal aperistalsis, with no signs of a mechanical cause of obstruction in the distal esophagus.1 Its current prevalence is 0.3 to 1.63 cases per 100,000 adults per year,2 with a similar distribution in both sexes and a mean patient age at presentation of 50 years. The main symptoms are dysphagia (90%), heartburn (75%), regurgitation or vomiting (45%), non-cardiac chest pain (20%), and involuntary weight loss (10%),3 which are evaluated through the Eckardt score.4 Its etiology is unknown, but in pathophysiologic terms it is thought that, in a genetically susceptible host, an autoimmune process triggered by a subclinical viral infection (in most cases, herpes) may lead to degeneration and loss of function of ganglion cells of the myenteric plexus in the distal esophagus at the level of the LES.5
High-resolution manometry provides detailed topography of esophageal pressure, which has become the method of choice for diagnosis and classification of achalasia.6,7 Currently, there are 3 subtypes, according to the Chicago classification:8 Type I or classic achalasia: characterized by elevated integrated relaxation pressure (IRP) (>15mmHg) with 100% failed peristalsis; Type II or achalasia with esophageal compression: elevated IRP with panesophageal pressurization in more than 20% of the swallows; and Type III or spastic achalasia: elevated IRP, abnormal peristalsis, and premature (spastic) contractions in more than 20% of the swallows.
Treatment is aimed at reducing the pressure gradient through the LES. There are different types of treatment: A) pharmacologic (calcium channel blockers or nitrates), which has a poor response; B) endoscopic (mainly botulinum toxin injection and esophageal balloon dilation), which has a good, but temporary, clinical response; and C) surgical (laparoscopic Heller myotomy [LHM] combined with an anti-reflux procedure), currently considered the gold standard.9
Peroral endoscopic myotomy (POEM) was developed in 2008 by Inoue et al.,10 and has demonstrated adequate safety and efficacy up to now. We have developed the technique since 2012 in ex vivo models and then in animal models. In 2014, we finally developed a protocol that evaluates the safety and efficacy of the procedure.11 Our aim was to describe the short-term and medium-term results of that endoscopic technique in a cohort of patients with achalasia at a tertiary care center in Mexico.
Materials and methodsA quasi-experimental study (before and after) was conducted at the Department of Gastrointestinal Endoscopy of the Centro Médico Nacional Siglo XXI within the time frame of November 2014 and February 2017.
Inclusion and exclusion criteriaPatients of either sex, older than 18 years of age, with a suspected diagnosis of esophageal achalasia based on upper endoscopy, barium esophagogram, and clinical evaluation findings and confirmed through high-resolution manometry were included in the study. Patients that presented with any pathology in which the procedure would be contraindicated, such as portal hypertension, premalignant conditions in the esophagus, some type of epiphrenic diverticulum, pregnant patients, or patients that rejected the procedure were excluded.
Pre-POEM evaluationPrior to the procedure, all patients were evaluated through upper endoscopy, timed barium esophagogram, high-resolution manometry, and thoracoabdominal tomography. In addition, each patient filled out the Eckardt clinical questionnaire and a quality of life questionnaire (AE-18). In all cases, Chagas disease was ruled out through a blood test.
Patient preparation- •
Patients were admitted 24h before the procedure.
- •
Antimicrobial prophylaxis was used 24h before the procedure with 1g cefotaxime IV or 1g ciprofloxacin IV in patients allergic to penicillin or cephalosporin, both as single doses.
- •
Fasting 24h prior to the procedure. Patients with megaesophagus or severe dilation received a liquid diet for 72h and fasted 24h before the procedure.
- •
If a subsequent adverse event presented, the decision was to continue antibiotic treatment for at least 5 days, either IV or oral.
The POEM procedure was performed according to that described by Inoue et al.,10 with the following accessories: a conventional endoscope model EG590WR (diameter 9.8mm, channel 2.8mm); a hood model DH-28GR (Fujinon, Tokyo, Japan); an ERBE VIO 200D electrosurgical unit with an I-type Hybrid Knife (Tübingen, Germany) with the following parameters: injection (ERBEJET, effect 50), incision (ENDOCUT Q, effect 3, cutting duration 3, and cutting interval 3), tunnelization (SWIFT COAG, effect 3 to 70 w), myotomy (ENDOCUT Q, effect 2, cutting duration 3, cutting interval 3), hemostasis (SOFT COAG, effect 3 to 40 w); Resolution Clip hemoclips (Boston Scientific, USA) or cyanoacrylate (B-Braun, USA) were used for incision closure. An insufflator (ENDO STRATUS, Medivators; Minneapolis, Minnesota, USA) and carbon dioxide were used in all the procedures.
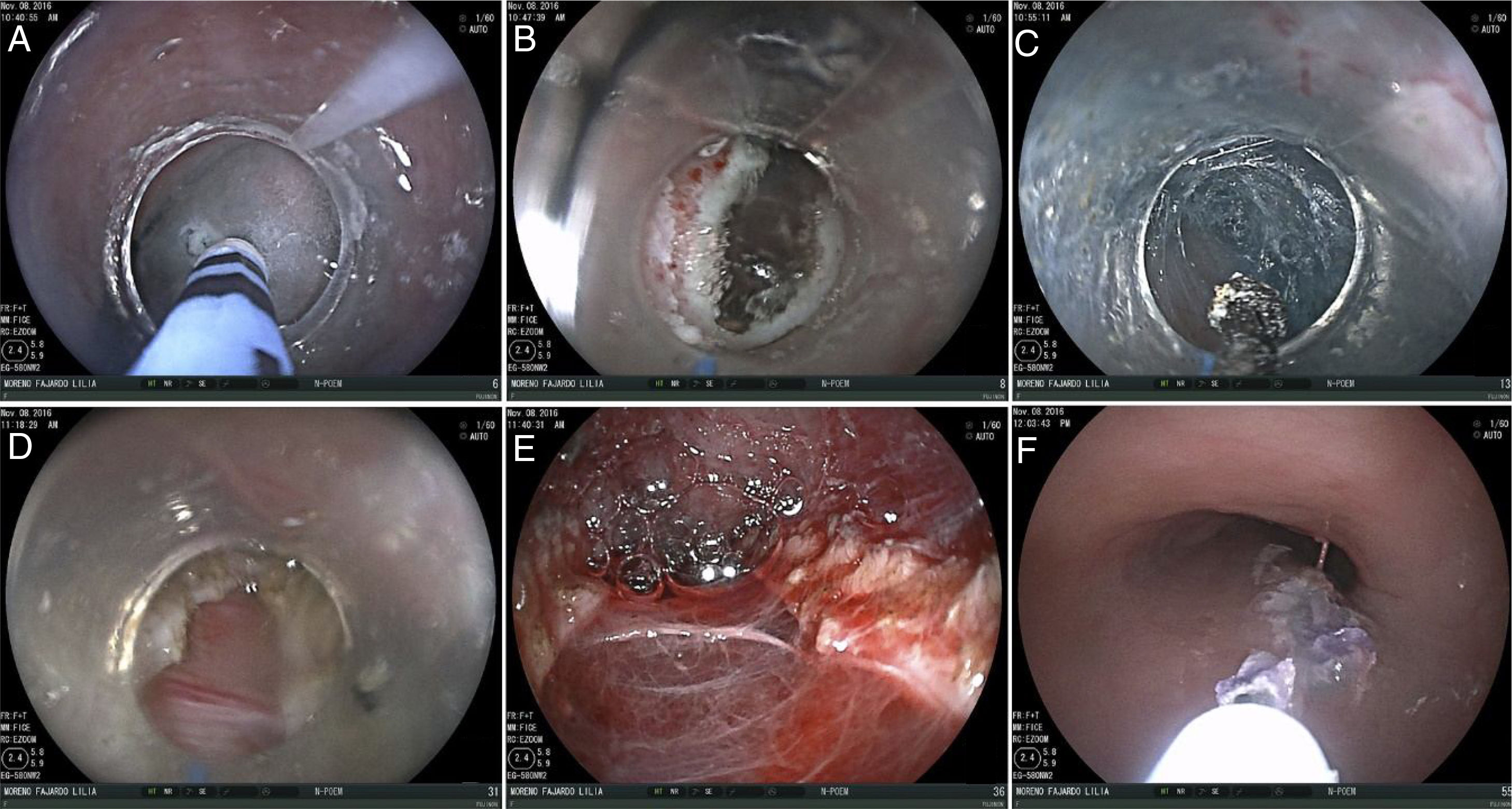
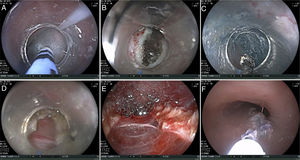
The internationally described technique we used for the POEM consisted of 5 steps (fig. 1):
- 1.
Examination and injection: Through upper diagnostic endoscopy, we located the esophagogastric junction (EGJ) and documented the distance from the incisors to the EGJ. The site for performing the anterior POEM was located (at the 2 o’clock position). A posterior POEM (6 to 8 o’clock position) was carried out on the previously-treated patients. A mixture of normal saline solution and methylene blue at 0.5% was injected with the hybrid knife at 13-15cm proximal to the EGJ in all the cases, except those with type III achalasia, in whom the injection was applied at 20cm from the incisors to perform a longer myotomy.
- 2.
Incision: A longitudinal incision, 10 to 15-mm long, was made parallel to the major axis of the esophagus and served as the entrance site to the submucosal tunnel.
- 3.
Tunnel: An injection was applied to elevate the submucosal space, which was then dissected from the entrance up to 2-3cm below the EGJ.
- 4.
Myotomy: It was begun 2cm under the incision, inside the submucosal tunnel as a partial myotomy (only cutting the internal circular layer of the esophagus) or a total myotomy (cutting both muscle layers [the last 20 cases]) and was continued up to the EGJ and extended 2cm below it. There were 3 methods for corroborating adequate myotomy: by measuring the location of the EGJ and 2cm below it, compared with the same measurement through the submucosal tunnel; through operator perception, feeling a decrease in resistance upon advancing the equipment to the level of the EGJ; and by performing a short retrovision in the stomach and observing the Z line or the opening of that region during moderate CO2 insufflation. Pediatric equipment is not available to us for performing the double-endoscope technique.
- 5.
Closure: Six to 8 hemoclips were used to close the incision. In the cases in which they could not be placed, or in which there was an adverse event at the entrance site, such as dehiscence due to the detachment of one of the clips, 1ml of undiluted cyanoacrylate was applied. The application was exactly at the entrance site, initially preloading it in a 3-ml syringe and then pushing it inside the tunnel with 3ml of injectable water. Obturation was observed immediately and adequate closure was corroborated through the instillation of water and the absence of “bubbles” coming from the tunnel at that site.
After the procedure, a thoracoabdominal x-ray was taken to document pneumoperitoneum or pneumomediastinum. If either was found, and did not have any clinical repercussions, no maneuver was carried out. If there was a manifest clinical repercussion, a decompression puncture was made with a 14-F catheter. Patients fasted for 24h and then a water-soluble contrast esophagogram was performed to rule out leakage into the submucosal tunnel. If there was no contraindication, liquid diet was begun, and patients were released 48-72h after the procedure. During hospital stay, patients received analgesic management with nonsteroidal anti-inflammatory drugs and antiemetics. Antibiotic therapy was initially administered IV and then completed PO for 5-7 days. The services of general surgery, cardiothoracic surgery, and intensive care were available 24/7 for attending to any complications.
Follow-upFollow-up was planned for one month after surgery, to be continued at postoperative months 3, 6, 12, 18, and 24, and then annually for 10 years. The following studies were carried out at each evaluation: upper endoscopy, high-resolution manometry, pH-study, a clinical evaluation of symptoms using the Eckardt scale, the AE-18 quality of life questionnaire, the gastroesophageal reflux disease questionnaire, and timed barium esophagogram, which was performed starting in May 2016 (n = 21).
DefinitionsClinical success: when the patient achieved an Eckardt score ≤ 3.
Manometric success: when an IRP < 15mmHg was attained post-procedure.
Minor complications: non-life-threatening complications that presented during or after the procedure. Resolved medically, endoscopically, or spontaneously, they included: mucosotomy (communication between the lumen of the gastrointestinal tract and the submucosal tunnel), minor bleeding during the procedure that did not require packed red blood cell administration, subcutaneous emphysema, pneumoperitoneum or pneumomediastinum with or without puncture during or after the procedure, dysphagia, and mild abdominal pain.
Major complications: life-threatening complications, those that required surgery, or whose resolution was difficult through any modality. They included: hemodynamic instability during the procedure, the need for blood transfusion due to bleeding during or after the procedure (even when there was adequate hemostasis), admission to the intensive care unit for surveillance, prolonged hospitalization (> 5 days), pneumonia, conversion to open surgery, an invasive postoperative procedure (chest tube placement, thoracotomy, etc.), and when the patient required hospital readmission due to signs of submucosal tunnel leakage, bleeding, or signs suggestive of mediastinitis.
Statistical analysisFor sample size, we used the mean difference method, considering the pre-procedure and post-procedure delta in the IRP value. A mean pre-procedure IRP value was set at 26 ± 5.5mmHg as the reference and a post-procedure change of at least 16 ± 3.5mmHg was regarded as significant. Considering a type I error of 5% and a type II error of 20%, a total of 40 patients were needed.
The quantitative variables with normal distribution were expressed as means, using standard deviation as the measure of dispersion. The median and interquartile range was used for the quantitative variables with skewed distribution. Normality was evaluated through the mental methods test and the Kolmogorov-Smirnov test. Qualitative and ordinal variables were expressed as proportions. Different tests were employed for the bivariate analysis: the Student's t test for the quantitative variables with normal distribution; the Wilcoxon test for the related variables (before-after); and the χ2 test for the qualitative variables or the Fisher's exact test (in the case of having an expected value < 5). The ANOVA, Kruskal-Wallis, and Pearson's χ2 or Fisher's exact test were respectively used for the same group comparisons at different post-procedure times, depending on the variable. The statistical analysis was carried out with the SPSS version 22.0 (Chicago, Illinois, USA) program. A p < 0.05 was considered statistically significant, and the corresponding confidence intervals were 95%.
ResultsGeneral characteristics of the procedure and the patientsA total of 50 procedures were performed within the time frame of November 2014 and February 2017 at the Department of Gastrointestinal Endoscopy of the Hospital de Especialidades Centro Médico Nacional Siglo XXI. Thirty-one of the patients were women (62%) and 19 were men (38%). Mean patient age was 48.8 ± 14.1 years and the time from first symptom onset to final disease diagnosis was a median of 24 months (9-140). Our cohort included: 41 treatment-naïve patients (82%), 7 previously-treated patients (14%) (all with LHM), and 2 patients (4%) that partially responded to initial POEM and were candidates for a second POEM procedure (redo-POEM).
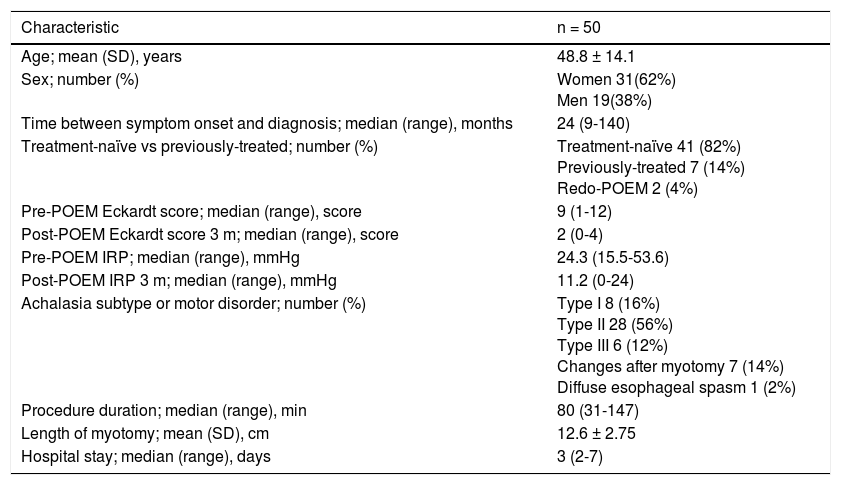
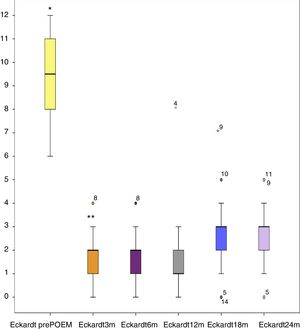
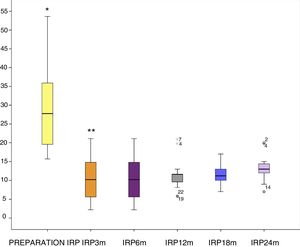
The median pre-procedure Eckardt symptom score values were 9 (1-12) and the post-procedure values were 2 (0-4). The pre-POEM IRP values had a median of 24.3mmHg (15.5-53.6) and at 3 months after the procedure, the median was 11.2mmHg (0-24). Eight patients had type I achalasia (16%), 28 had type II (56%) (the most frequent in our cohort), and 6 patients had type III (12%). In relation to motor disorders, 7 patients had changes due to previous myotomy (14%) and one patient had signs of distal esophageal spasm (DES) (2%). Median procedure duration was 80min (31-147) and mean myotomy length was 12.6 ± 2.75cm. Median hospital stay was 3 days (2-7) (Table 1).
Procedure and patient characteristics.
| Characteristic | n = 50 |
|---|---|
| Age; mean (SD), years | 48.8 ± 14.1 |
| Sex; number (%) | Women 31(62%) Men 19(38%) |
| Time between symptom onset and diagnosis; median (range), months | 24 (9-140) |
| Treatment-naïve vs previously-treated; number (%) | Treatment-naïve 41 (82%) Previously-treated 7 (14%) Redo-POEM 2 (4%) |
| Pre-POEM Eckardt score; median (range), score | 9 (1-12) |
| Post-POEM Eckardt score 3 m; median (range), score | 2 (0-4) |
| Pre-POEM IRP; median (range), mmHg | 24.3 (15.5-53.6) |
| Post-POEM IRP 3 m; median (range), mmHg | 11.2 (0-24) |
| Achalasia subtype or motor disorder; number (%) | Type I 8 (16%) Type II 28 (56%) Type III 6 (12%) Changes after myotomy 7 (14%) Diffuse esophageal spasm 1 (2%) |
| Procedure duration; median (range), min | 80 (31-147) |
| Length of myotomy; mean (SD), cm | 12.6 ± 2.75 |
| Hospital stay; median (range), days | 3 (2-7) |
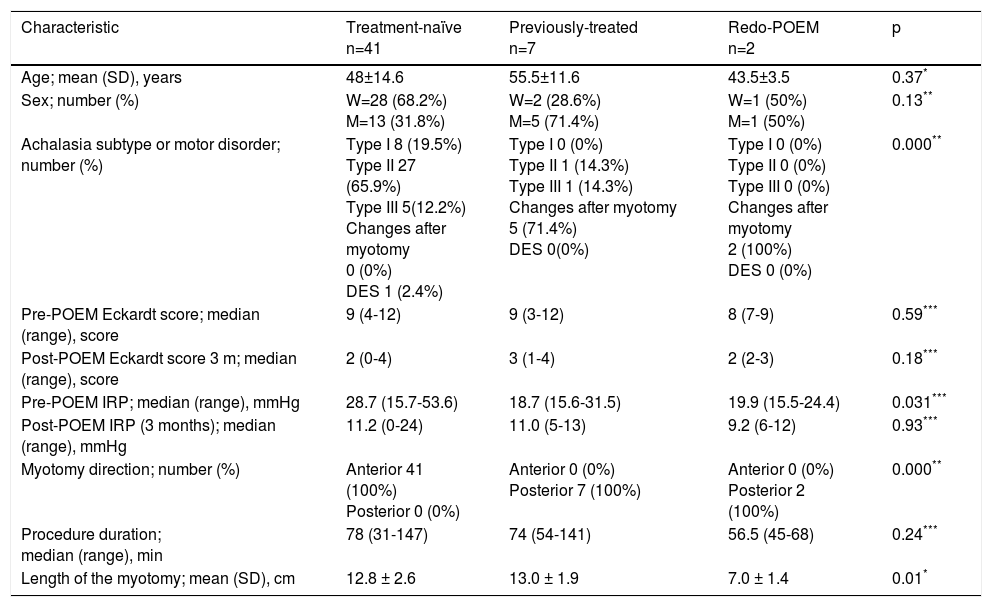
After comparing the different types of patients included in the study, there were no statistically significant differences in relation to age, sex, the pre-POEM Eckardt scores, and the post-POEM Eckardt scores at 3 months, procedure duration, and post-POEM IRP values at 3 months. However, there were statistically significant differences among groups with respect to achalasia subtype or motor disorder; most of the treatment-naïve patients were type II (27 = 65.9%), followed by type I (8 = 19.5%), and finally type III (5 = 12.2%), as well as the case of DES (1 = 2.4%) included in the late group. The previously-treated cases were statistically different from those in the treatment-naïve group. The former had a total of only 7 cases. The previously-treated group had no type I cases, there was one (14.3%) type II case, one (14.3%) type III, and 5 cases could not be correctly classified through the Chicago classification and were catalogued as changes due to previous myotomy. The redo-POEM group consisted of only 2 cases (100%) and they had undergone a previous failed POEM. Other statistically significant differences between those two groups were the pre-POEM IRP levels. The treatment-naïve patients had a higher IRP value with a median of 28.7mmHg (15.7-53.6), compared with 18.7mmHg of the previously-treated patients and 19.9mmHg of the redo-POEM group. Thus, only the comparison between the naïve-treatment patients versus the previously-treated patients was statistically significant (p=0.007), but the treatment-naïve group versus the redo-POEM group was not, nor was the previously-treated group versus the redo-POEM group (p = NS). There was a statistically significant difference in relation to the direction of the myotomy. Obviously, it was anterior in all the treatment-naïve patients (41 = 100%) and posterior in the previously-treated patients (7 = 100%) and redo-POEM patients (2 = 100%). Finally, myotomy length was longer in the treatment-naïve patients and the previously-treated patients, with 12.8 ± 2.6cm and 13.0 ± 1.9cm, respectively, compared with 7.0 ± 1.4cm in the redo-POEM patients, demonstrating statistical differences between the redo-POEM group and the other 2 groups (treatment-naïve group vs redo-POEM group [p = 0.008] and previously-treated group vs redo-POEM group [p = 0.016]) (Table 2).
Differences between treatment-naïve patients and previously-treated patients.
| Characteristic | Treatment-naïve n=41 | Previously-treated n=7 | Redo-POEM n=2 | p |
|---|---|---|---|---|
| Age; mean (SD), years | 48±14.6 | 55.5±11.6 | 43.5±3.5 | 0.37* |
| Sex; number (%) | W=28 (68.2%) M=13 (31.8%) | W=2 (28.6%) M=5 (71.4%) | W=1 (50%) M=1 (50%) | 0.13** |
| Achalasia subtype or motor disorder; number (%) | Type I 8 (19.5%) Type II 27 (65.9%) Type III 5(12.2%) Changes after myotomy 0 (0%) DES 1 (2.4%) | Type I 0 (0%) Type II 1 (14.3%) Type III 1 (14.3%) Changes after myotomy 5 (71.4%) DES 0(0%) | Type I 0 (0%) Type II 0 (0%) Type III 0 (0%) Changes after myotomy 2 (100%) DES 0 (0%) | 0.000** |
| Pre-POEM Eckardt score; median (range), score | 9 (4-12) | 9 (3-12) | 8 (7-9) | 0.59*** |
| Post-POEM Eckardt score 3 m; median (range), score | 2 (0-4) | 3 (1-4) | 2 (2-3) | 0.18*** |
| Pre-POEM IRP; median (range), mmHg | 28.7 (15.7-53.6) | 18.7 (15.6-31.5) | 19.9 (15.5-24.4) | 0.031*** |
| Post-POEM IRP (3 months); median (range), mmHg | 11.2 (0-24) | 11.0 (5-13) | 9.2 (6-12) | 0.93*** |
| Myotomy direction; number (%) | Anterior 41 (100%) Posterior 0 (0%) | Anterior 0 (0%) Posterior 7 (100%) | Anterior 0 (0%) Posterior 2 (100%) | 0.000** |
| Procedure duration; median (range), min | 78 (31-147) | 74 (54-141) | 56.5 (45-68) | 0.24*** |
| Length of the myotomy; mean (SD), cm | 12.8 ± 2.6 | 13.0 ± 1.9 | 7.0 ± 1.4 | 0.01* |
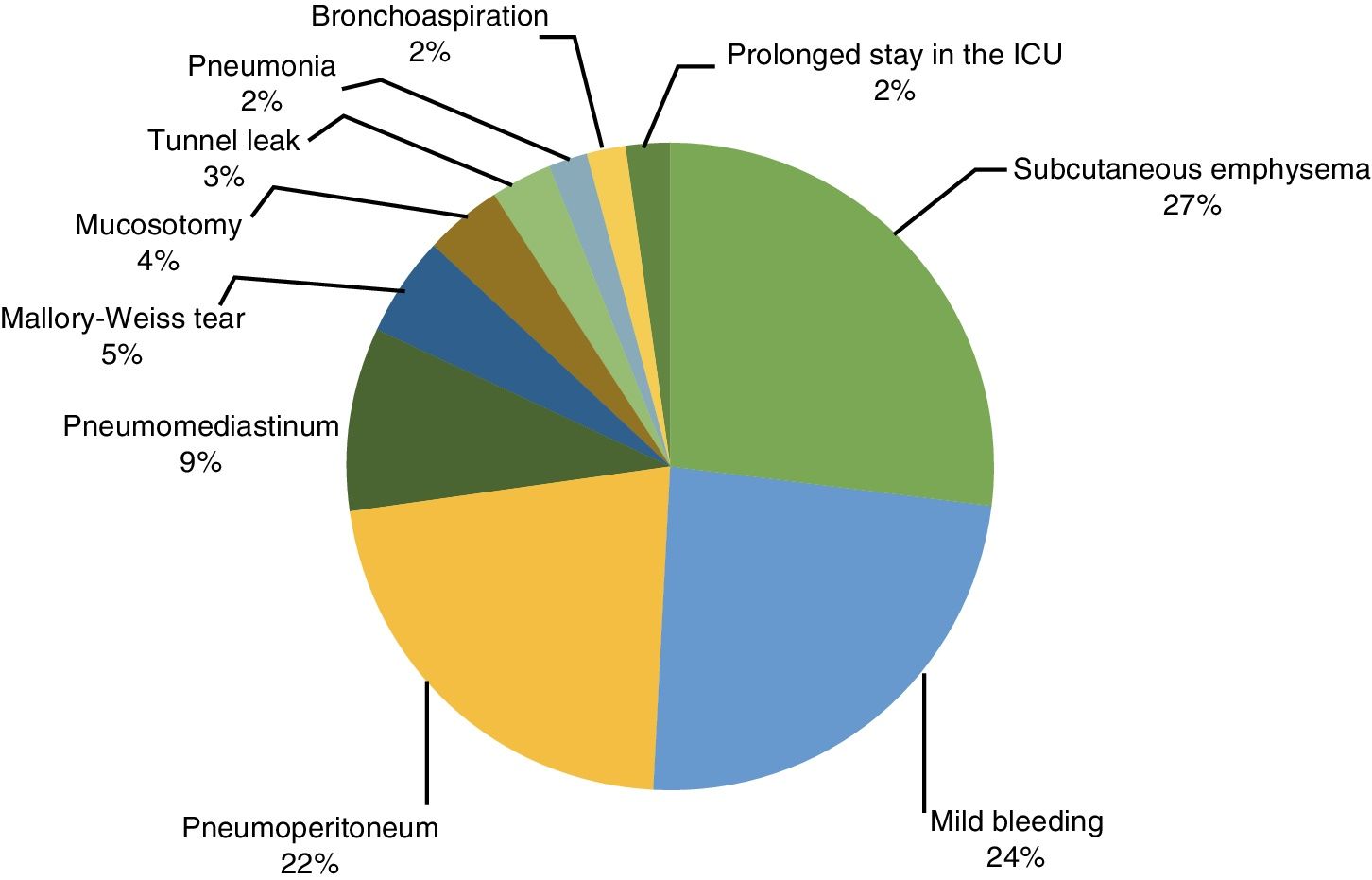
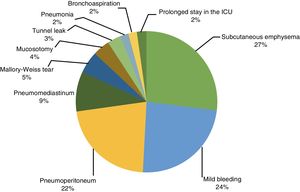
Several adverse events presented after the procedure: subcutaneous emphysema was the most frequent, presenting in 15/50 (27%) of the patients immediately after the procedure, followed by intraoperative bleeding in 13/50 (24%), with endoscopic control in all the cases. Pneumoperitoneum presented in 12/50 (22%) and pneumomediastinum in 5/50 (10%). Large-caliber needle puncture for decompression was necessary in only 5 of those patients, and it was performed post-procedure in all of them. Mucosotomy presented in 3 cases, requiring endoscopic treatment with cyanoacrylate. In one of the patients, it was evidenced through an upper gastrointestinal x-ray with water-soluble contrast medium and in another, it presented 48h after the procedure as a Mallory-Weiss tear. One patient presented with pneumonia, most likely due to aspiration during intubation, and it was medically resolved. One patient was admitted to the intensive care unit for 72h due to suspected pulmonary thromboembolism, which was then ruled out. Finally, one patient presented with cardiac arrhythmia during the study and was hospitalized and evaluated by the cardiology service. POEM completion was not contraindicated. There were no deaths associated with the procedure (fig. 2).
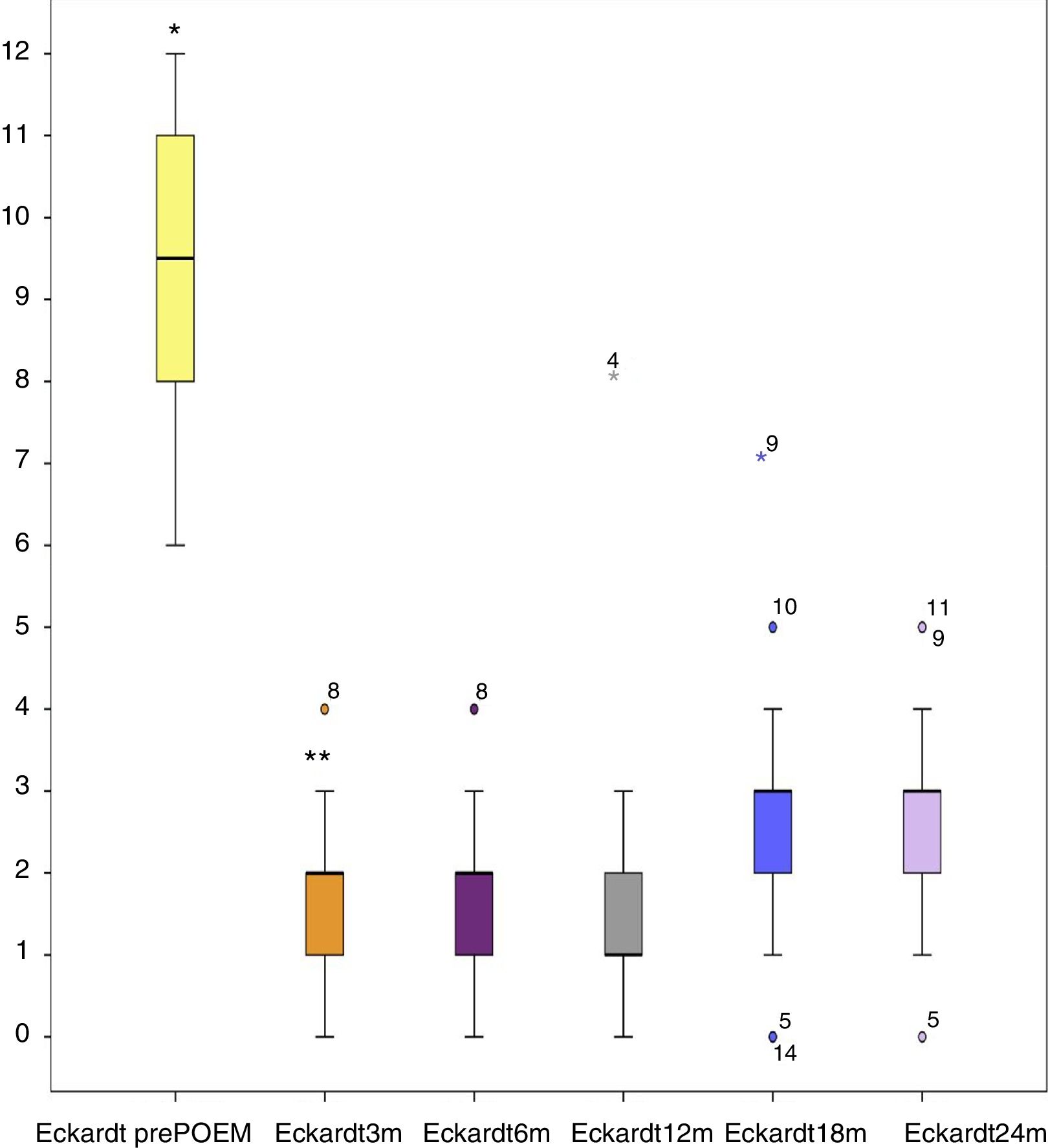
Short-term and medium-term follow-upThe median Eckardt score prior to the procedure was 9 and it decreased to a median of 2 after the procedure, resulting in clinical success at 3 months in all patients except 2. The median remained unchanged at post-POEM follow-up months 6, 12, 18, and 24. At 24 months only 22/50 (44%) patients continued in follow-up and were exclusively treatment-naïve patients, given that at the time of this writing, all of the previously-treated patients and redo-POEM patients had fewer than 18 months of follow-up. However, no differences in clinical response were found between the 3 treatment groups, and the Eckardt scores of the patient cohort remained unchanged at the short term and at the medium term. Statistically significant differences were observed only between the pre-procedure scores and the scores obtained after the procedure, with the exception of the post-procedure Eckardt scores at 24 months (fig. 3).
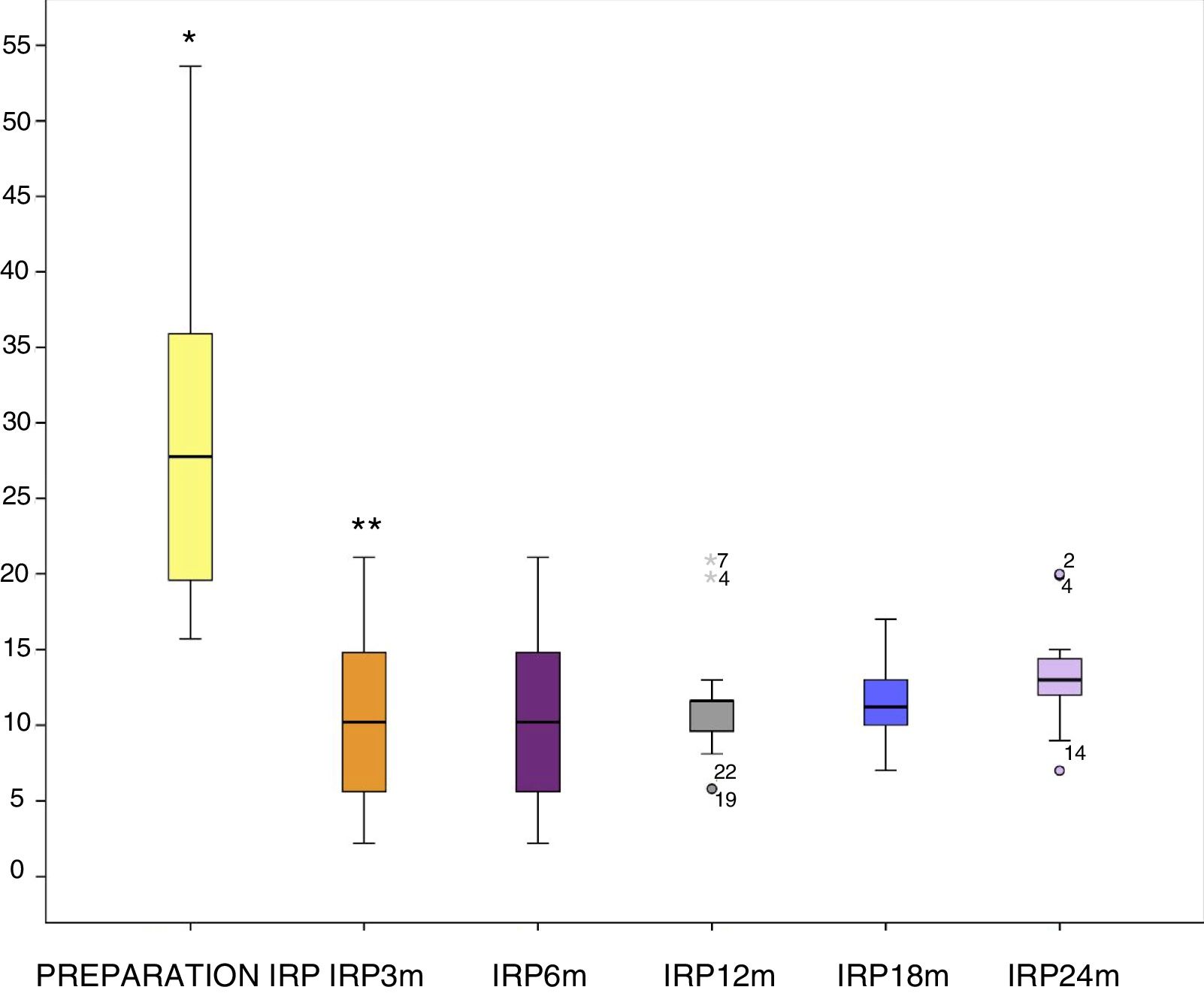
The IRP decreased from a pre-procedure median of 24.3mmHg (15.5-53.6) to 11.2mmHg (0-24) at 3 months after the procedure. The decrease in the IRP remained unchanged up to month 24 of the follow-up, where a slight increase in the median to 13.5mmHg was observed. Prior to that value, no statistically significant differences between post-procedure IRP values were found. At present, all the evaluated patients have been treatment-naïve patients, given that no previously-treated patients or redo-POEM patients has yet reached follow-up month 24 (fig. 4).
Post-procedure gastroesophageal refluxAll the patients were treated with a standard dose of a proton pump inhibitor (PPI) for 30 days, after which the patients had no medical treatment and were evaluated at 3, 6, 12, 18, and 24 months after the procedure. At post-procedure month 3, 35/50 (70%) patients presented with a positive pH-study (> 14.73), 8/50 (16%) had clinical reflux, and 15/50 (30%) had esophagitis (grades A and B in 80% of the cases). We then decided to begin a double dose of PPI for 4 weeks, and at the evaluation at 6 months, of the 43/50 (86%) patients that reached that point of the follow-up, 65% did not present with esophagitis, but 35% did; 12.5% of those patients had grade A esophagitis, 20% had grade B, and 2.5% had grade C, according to the Los Angeles classification. The pH-study was positive in 47.5% of the patients and 15% had clinical reflux. The decision was made to give those patients a standard PPI dose for an indefinite period of time, and at the evaluation at month 24, only 5% of the patients still had a positive endoscopy (grade A or B Los Angeles classification erosive esophagitis), 10% had clinically evident gastroesophageal reflux (heartburn), and 10% had a positive pH-study. Thus, there was no correlation between the instrumented pH measurement and the clinical method for evaluating that parameter, but it could be medically controlled in all cases through PPI dose readjustments.
Discussion and conclusionsThe POEM procedure was introduced in 2008 and has been widely described since 2010. Numerous studies, including a meta-analysis, have evaluated the efficacy and safety of that procedure worldwide, motivating our group to learn the novel endoscopic-surgical technique.12–14 According to modern surgical technique learning models, before performing a procedure on humans, the technique must be mastered. We established that at least 26 procedures need to be carried out on an animal model to reduce potential complications and improve the efficacy of the procedure, before moving on to a patient with achalasia.15
Our results were similar to those of different international prospective cohort studies that showed clinical efficacy greater than 90% and manometric efficacy (IRP < 15mmHg) > 85%.16–18 In our study, we found that 20/22 (91%) of the cases at month 24 of the post-treatment follow-up continued to have clinical improvement and that 19/22 (86%) continued with manometric improvement. Those results concurred with outcomes obtained in populations different from ours, in which clinical success was greater than 95% after the procedure. It was maintained during the first 12 months and then decreased to 80-85% after 24 post-treatment months.19 Initial improvement in IRP levels has also been observed, with an over 50% decrease from the baseline level, but with the passage of time, it appears that those levels gradually rise, albeit not significantly (< 10%).20
Achalasia is an uncommon disease in the Mexican population and presents more frequently in women. The mean presentation age is similar to that of the 50 years of age reported by other authors, but one of the most important problems we face
in Mexico is diagnostic delay. It has a median of 24 months from first symptom onset to the final diagnosis. That is consequential, because many Mexican patients presenting with subtle signs of the disease, especially young patients, are commonly treated as cases of GERD and do not respond to medical treatment. Some are referred to surgery and are incidentally diagnosed through preoperative manometry. All those factors delay disease diagnosis and coincide with the related data from reviews conducted by other authors.1,2,5
As in other studies, most of our patients had no previous endoscopic or surgical treatment and the most frequent achalasia subtype was type II. However, in terms of treatment response, we found no statistical significance between them. In fact, at month 3 of the post-procedure evaluation, the 2 patients that did not respond to initial peroral myotomy and underwent a second procedure, belonged to the group of patients with type II achalasia. However, because that subtype group was the most common, there was no statistically significant difference in relation to the other subtypes. That differs slightly from other studies whose authors have preliminarily reported that patients with type II achalasia have greater treatment response, compared with the other types. Nevertheless, that response appears to be only during short-term evaluations (12-18 months) and has been shown to not necessarily be true in evaluations conducted after longer periods of time. Most likely all cases of esophageal achalasia will decrease, regardless of subtype, the cause of which is not yet known. In other words, it could be related to a problem involving pathophysiology (a gradual increase in baseline and residual pressure of the LES due to an immunologic phenomenon that has not been eliminated) or to a problem of cicatrization at the level of the LES, due to treatment that could cause an increase or alteration in the levels of sphincter pressure measurement.1,2,4,16,17,20
The procedure characteristics were similar to those reported in the literature in terms of time and the aspects of each step of the technique. We had a median total surgery duration of 80min (30-147), the differences of which we attributed to the learning curve. We documented the change in performance velocity after the first 20 cases, in which the median was higher (90min), compared with the more recent cases (30) (median of 65min) (p < 0.05). We realized that the practice and standardization we carried out in animal models were necessary, but not sufficient for complete mastery of the technique. Results were heterogeneous when compared with other works. Different studies maintained a similar median procedure time (80min), but when the learning curve was evaluated, it differed greatly (20 cases vs 86). When each group was evaluated, those that did not have an animal model to learn on had a longer curve than those that did, explaining the heterogeneity in mastering the technique, in which safety and time are among the most important parameters.2,3,17,19,20 Along with learning the technique, our group has also implemented new alternatives, such as closure with cyanoacrylate at the level of the entrance site, initially or when adverse events present. That option was utilized on two of our patients that had entrance site dehiscence that could not be resolved in the conventional manner with hemoclips, significantly increasing the safety of the procedure.21
However, regarding myotomy, we observed a difference between the groups, because 2 patients that had already been treated through endoscopy required a short myotomy (mean of 7cm), compared with the other two treatment groups, in which myotomy was larger than 10cm. On average, it was extended to more than 15cm in patients with type III achalasia. The differences found with respect to the direction of the myotomy had to do with the fact that the approach had previously been anterior in the 2 patients with redo-POEM and in the patients that had undergone surgery. Therefore, the posterior approach was performed in those patients. Only the treatment-naïve patients had the anterior approach, as is documented in other centers.22–25 We also observed logical differences in those patients with a pre-procedure IRP included in our study. The previously-treated patients and the 2 redo-POEM patients had a lower IRP, compared with the treatment-naïve patients. Nevertheless, those IRP values did not signify greater clinical improvement, compared with the medical treatment-naïve patients, nor were there any differences between the patients with the anterior approach or those with the posterior approach, such as a greater tendency to present with GERD that has been documented in some studies.17–20
The Eckardt score and IRP evaluations for the follow-up are the 2 criteria that have classically been used to assess achalasia patients. However, the use of the esophagogram, especially the timed one, is excellent for evaluating patients previously-treated for achalasia.26 We decided to use the timed esophagogram, given that it appears to have a greater prognostic value for the preliminary evaluation of previously-treated patients. All our patients, including the previously-treated patients and the patients with redo-POEM, had a delay in emptying at 5min greater than 50%, but there was an average 20% improvement in the post-POEM evaluation in the majority of the patients, which was related to the clinical and manometric improvement in those patients. However, its value in cases of very dilated esophagus, or megaesophagus, appears to be low, especially when the barium column is evaluated (as in our case) and not the quantification of the volume emptied at 5min, where it could have more benefit in those types of patients.
The gastroesophageal reflux data we found has also been previously reported in different studies,27 in which it was demonstrated that although there was no clinical, endoscopic, or pH-study correlation, as in our analysis, the majority of previously-treated patients had high abnormal exposure to acid at the esophageal level. Even though we do not know the significance of that problem in the medium term or the long term, especially because most of the patients only presented with mild-to-moderate endoscopic lesion (grades A and B esophagitis), it could have the same consequence if not treated correctly, especially when the EGJ has been altered, as in the case of POEM. Therefore, at 6 months after the POEM, our patients were treated with a PPI dose for an indefinite period of time, which resulted in adequate disease control in practically all the cases. Only 5% of the patients had abnormal acid exposure and 10% of patients had positive endoscopy and clinical reflux at 24 months after treatment. We did not consider weight gain (a mean of 5.4 ± 0.73kg at post-procedure month 6), which is a factor that could have a negative effect on the reflux evaluation of those patients.
Finally, both the IRP and the Eckardt score remained a “success” during the follow-up period, but at the measurement at 24 months, there was a tendency for their levels to increase. This could be very important, given that a longer follow-up period would probably show clinical and manometric data consistent with disease recurrence and they could be related to the pathophysiology of achalasia (keeping in mind that our treatment only improved emptying, with no action on pathophysiology). They could also explain the cases of disease recurrence that are attributed to poor surgical or endoscopic technique (whether for lack of myotomy or poor patient characterization before the procedure) and not to the actual effect of the pathophysiology of the disease, which could result in recurrence, regardless of the treatments currently offered. Therefore, longer term measurement of those variables could reflect the true role of POEM in the treatment of patients with achalasia.
Even though ours were short-term and medium-term results and the patient cohort was relatively small (considering the low disease prevalence and the inclusion of only one patient with distal esophageal spasm), we believe that our study results demonstrate that POEM is a true alternative and procedure of choice in patients with achalasia and other esophageal motor disorders.
In conclusion, with the proper training, hospital infrastructure, and instrumentation, POEM represents an advance in therapeutic-surgical endoscopy, with high short-term and medium-term success rates in the Mexican population for treating patients with achalasia and other motor disorders of the esophagus. Its adverse events are minor and easily controlled. Secondary gastroesophageal reflux, if present, can be medically controlled with satisfactory results. However, longer-term studies are needed to determine the true role of POEM in treating achalasia.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of dataThe authors declare that no patient data appear in this article.
Right to privacy and informed consentThe authors declare that no patient data appear in this article.
Financial disclosureNo financial support was received in relation to this study.
Conflict of interestThe authors declare that there is no conflict of interest.
Please cite this article as: Hernández-Mondragón OV, Solórzano-Pineda OM, González-Martínez MA, Blancas-Valencia JM, Caballero-Luengas C. Miotomía endoscópica peroral para el tratamiento de acalasia y otros trastornos motores del esófago. Resultados a corto y mediano plazo en un centro de referencia en México. Revista de Gastroenterología de México. 2019;84:1–10.