We appreciate and read with great interest the Letter to the Editor sent by Phinder-Puente M.E. et al., in which they underline the utility of serum ammonia in the context of hepatic encephalopathy (HE) and consider that serum ammonia quantification could be useful in making or ruling out the diagnosis of HE. In that regard, in the study they cited, conducted by Gundling et al.,1 venous ammonia levels > 65 μmol/l had a diagnostic accuracy of just 59%. Even though specificity (Sp) for diagnosing HE was 95%, sensitivity (S) was only 41.7%. It should be pointed out that in the Discussion section of their study, Gundling et al. even stated that ammonia levels “do not reliably detect HE” and cannot be considered a useful screening test for HE. However, ammonia level determination, importantly, could be positioned as a tool for ruling out HE.
With respect to the cited work of Nicolao et al.,2 in which 42 patients with cirrhosis were analyzed, only 27 of them had HE. The primary aim of that study was to determine whether partial pressure of ammonia (ppNH3) quantification was better than arterial ammonia or venous ammonia quantification, in patients with or without HE. Those authors found that the correlation for “severity” of HE was similar between arterial ammonia (r = 0.76), venous ammonia (r = 0.72), and ppNH3 (r = 0.75). The reported S and Sp, as well as the cutoff point for diagnosing HE (the fact that only 27 patients with HE were included should be emphasized), for a ppHN3 of 6.4 mmHg × 10−5 were 85% S and 93% Sp, with an area under the curve (AUC) of 0.92; for a venous ammonia level of 73 μg/dl were 85% S and 93% Sp, with an AUC of 0.90; and for an arterial ammonia level of 101 μg/dl were 92% S and 86% Sp, with an AUC of 0.93. Importantly, 17 of those 27 patients evaluated continued to have elevated, or even higher, ammonia levels in the three variants after complete symptom resolution of HE, showing the absence of correlation between serum ammonia and the clinical picture of the syndrome.
Regarding ammonia levels and prognosis, Phinder-Puente et al. cite an article by Verma et al.3 that included 3,009 patients with acute-on-chronic liver failure (ACLF). Indeed, ammonia levels were associated with the presence of HE (OR: 1.007), but other factors had a greater association strength than serum ammonia in the multivariate analysis, such as age (OR: 1.03), systemic inflammatory response syndrome (SIRS) (OR: 1.23), sepsis (OR: 1.58), and the model for end-stage liver disease (MELD) score (OR: 1.04). Total serum protein values were a protective factor (OR: 0.73). With respect to independent predictors of progression of HE, an Asian Pacific Association for the Study of the Liver-ACLF Research Consortium (AARC) score > 9 had an OR of 1.15, whereas ammonia levels > 85 μmol/l had an OR of 1.002. Importantly, neither ammonia levels nor the other variables were utilized for diagnosing HE.
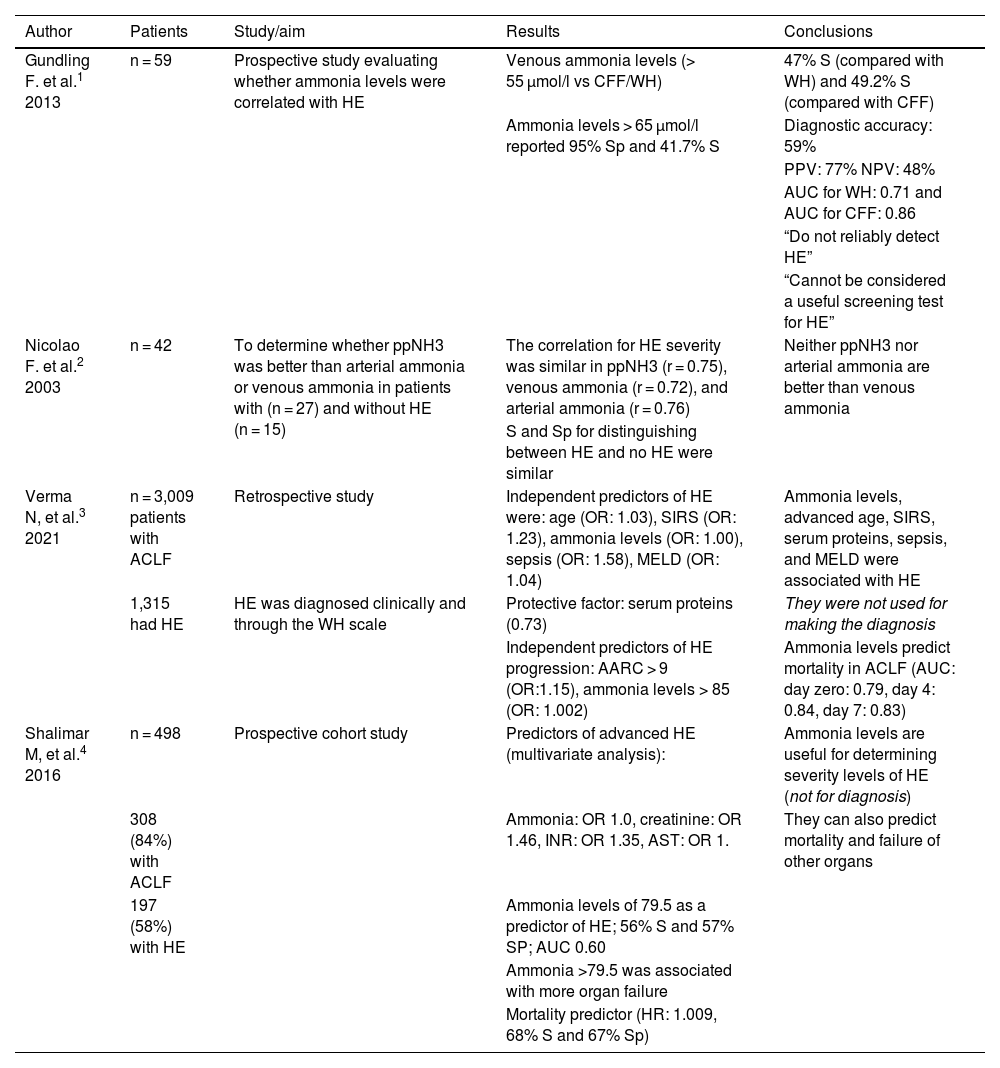
Likewise, the work by Shalimar et al.4 was a prospective cohort study (n = 498) that included 308 subjects with ACLF (84%) and 197 (58%) with HE. The authors determined predictors of HE in a multivariate analysis: ammonia (OR: 1.0), serum creatinine (OR: 1.46), international normalized ratio (INR) (OR: 1.35), and aspartate aminotransferase (AST) (OR: 1). Ammonia levels > 79.5 µmol/l predicted HE with 56% S, 57% Sp, and an AUC of 0.60. Ammonia > 79.5 µmol/l was associated with more organ failure and was a predictor of mortality (HR: 1.009, 68% S and 67% Sp). Given the above, we agree that ammonia levels can be a good prognostic marker, and even predict mortality, but is should be noted that the cutoff point is not altogether standardized.3,4Table 1 summarizes the main comments on the findings of studies referred to by the authors.
Main characteristics of the studies referred to on ammonia and hepatic encephalopathy.
| Author | Patients | Study/aim | Results | Conclusions |
|---|---|---|---|---|
| Gundling F. et al.1 2013 | n = 59 | Prospective study evaluating whether ammonia levels were correlated with HE | Venous ammonia levels (> 55 µmol/l vs CFF/WH) | 47% S (compared with WH) and 49.2% S (compared with CFF) |
| Ammonia levels > 65 µmol/l reported 95% Sp and 41.7% S | Diagnostic accuracy: 59% | |||
| PPV: 77% NPV: 48% | ||||
| AUC for WH: 0.71 and AUC for CFF: 0.86 | ||||
| “Do not reliably detect HE” | ||||
| “Cannot be considered a useful screening test for HE” | ||||
| Nicolao F. et al.2 2003 | n = 42 | To determine whether ppNH3 was better than arterial ammonia or venous ammonia in patients with (n = 27) and without HE (n = 15) | The correlation for HE severity was similar in ppNH3 (r = 0.75), venous ammonia (r = 0.72), and arterial ammonia (r = 0.76) | Neither ppNH3 nor arterial ammonia are better than venous ammonia |
| S and Sp for distinguishing between HE and no HE were similar | ||||
| Verma N, et al.3 2021 | n = 3,009 patients with ACLF | Retrospective study | Independent predictors of HE were: age (OR: 1.03), SIRS (OR: 1.23), ammonia levels (OR: 1.00), sepsis (OR: 1.58), MELD (OR: 1.04) | Ammonia levels, advanced age, SIRS, serum proteins, sepsis, and MELD were associated with HE |
| 1,315 had HE | HE was diagnosed clinically and through the WH scale | Protective factor: serum proteins (0.73) | They were not used for making the diagnosis | |
| Independent predictors of HE progression: AARC > 9 (OR:1.15), ammonia levels > 85 (OR: 1.002) | Ammonia levels predict mortality in ACLF (AUC: day zero: 0.79, day 4: 0.84, day 7: 0.83) | |||
| Shalimar M, et al.4 2016 | n = 498 | Prospective cohort study | Predictors of advanced HE (multivariate analysis): | Ammonia levels are useful for determining severity levels of HE (not for diagnosis) |
| 308 (84%) with ACLF | Ammonia: OR 1.0, creatinine: OR 1.46, INR: OR 1.35, AST: OR 1. | They can also predict mortality and failure of other organs | ||
| 197 (58%) with HE | Ammonia levels of 79.5 as a predictor of HE; 56% S and 57% SP; AUC 0.60 | |||
| Ammonia >79.5 was associated with more organ failure | ||||
| Mortality predictor (HR: 1.009, 68% S and 67% Sp) |
AARC: Asian Pacific Association for the Study of the Liver Acute-on-Chronic Liver Failure Research Consortium model; ACLF: acute-on-chronic liver failure; AUC: area under the curve; HE: hepatic encephalopathy; Sp: specificity; CFF: critical flicker frequency; HR: hazard risk; INR: international normalized ratio; MELD: model for end-stage liver disease; OR: odds ratio; ppNH3: partial pressure of ammonia; S: sensitivity; SIRS: systemic inflammatory response syndrome; NPV: negative predictive value; PPV: positive predictive value: WH: West Haven scale.
Likewise, in the current Mexican guidelines,5 we stated that the information is controversial, given that some studies describe ammonia levels as useful, with respect to severity and prognosis, whereas others report no differences in those aspects. It is worth noting that those studies tend to have similar limitations, especially the fact that they include few patients. Other limitations, as mentioned above, are the fact that the cutoff points showing association, particularly with prognosis, are not completely standardized, and severity and prognosis in HE are multifactorial and do not depend only on serum ammonia levels. Kundra et al.6 evaluated patients with acute liver failure and with cirrhosis, measuring ammonia levels to correlate them with HE severity. There was adequate correlation only in the patients with acute liver failure (r = 0.91, p < 0.05); correlation in the patients with cirrhosis (r = 0.30, p < 0.05) was not good.
On the other hand, it is important to point out that ammonia is not the only cause of HE in critically ill patients with cirrhosis. In a prospective study on 100 patients with cirrhosis, 59% were admitted to the intensive care unit with grade 3 HE, 46% of the patients had positive cultures, 22% had signs of SIRS with negative cultures, and HE severity was not correlated with ammonia levels.7
In their letter, Phinder-Puente et al. state that the guidelines of the European Association for the Study of the Liver (EASL) recommend the routine use of ammonia level quantification. They make that suggestion because if levels are normal, the HE diagnosis should be questioned and a differential diagnosis, such as delirium, for example, should be contemplated instead. Those guidelines also state that there are patients without HE and without liver disease that can have elevated ammonia levels. Thus, we believe that the negative predictive value (NPV) of ammonia should be considered, i.e., that it is a valuable datum in the context of ruling out HE, but not as a specific diagnostic tool. The EASL recommendation does not provide a cutoff point or ammonia level for determining normality or abnormality, and importantly, it is a “level 4” recommendation, which means information is lacking and the statement can change as a result of future research.8
In their 2014 guidelines, the American Association for the Study of Liver Disease (AASLD), together with the EASL, stated that elevated blood levels of ammonia alone do not add any diagnostic, prognostic, or staging value for HE in patients with cirrhosis. However, if levels are determined in a patient suffering from HE, and the values are normal, the diagnosis should be questioned, and other causes of altered mental state should be investigated.9
The consensus of the International Society for Hepatic Encephalopathy and Nitrogen Metabolism (ISHEN) states that there can be elevated ammonia levels in the clinical absence of HE and that values can be normal in up to 60% of patients with cirrhosis that arrive at the emergency room presenting with an altered mental state. A significant explanation for that is the association of infections and inflammation in the pathophysiology of HE. Nevertheless, low levels of ammonia in a patient with cirrhosis and HE could motivate the investigation of diagnostic alternatives. It should be taken into account that external factors, such as valproic acid, can elevate ammonia levels. The ISHEN consensus recommends that if the decision is made to draw a sample for measuring ammonia levels, the patient should be fasting, and venous blood should be drawn, placed in a tube with a stabilizer, immediately refrigerated on ice, sent to the laboratory, and analyzed at once, preferably within 30-60 minutes.10
Lastly, the diagnostic algorithm proposed by Phinder-Puente et al. suggests carrying out serum ammonia level quantification in patients that cannot undergo neurologic examination. That could certainly be done to rule out HE due to the elevated NPV, but the fact that there are patients with HE whose ammonia levels are normal must be underlined. Therefore, HE cannot be completely ruled out, and in that context, the patient should continue to be managed empirically, adding tests, such as tomography, resonance, cultures, complete biochemical profile, etc., to make the correct differential diagnosis.
Conflict of interestThe authors declare that they have no conflict of interest.
Please cite this article as: Velarde-Ruiz Velasco JA, Aldana-Ledesma JM, Higuera-de-la-Tijera F. Respuesta a Phinder-Puente M.E. et al. Visión actual sobre el diagnóstico y cuidados integrales en encefalopatía hepática. Rev Gastroenterol Mex. 2023;88:457–459.