Twenty percent of patients with portal hypertension develop gastric varices. The risk for bleeding varies from 5 to 10%, and some authors have reported up to 16%.1 Gastric variceal bleeding has greater severity and a higher mortality rate than esophageal variceal bleeding.2
Endoscopic intravariceal cyanoacrylate (CYA) injection is first-line treatment for acute bleeding, as well as for secondary prophylaxis.3 Hemostasis is achieved in 90% of the cases and the risk for rebleeding is 15 to 30%. The most dreaded complication is CYA pulmonary embolism that manifests clinically in approximately 5% of cases.4,5
Endoscopic ultrasound-guided CYA injection has the advantage of direct visualization. It corroborates variceal obliteration through Doppler ultrasound and enables CYA injection to be directed at the perforating or feeding veins.6
The technique of coil injection under echo-endoscopic guidance, followed by CYA injection (B-CYA plus Lipiodol or O-CYA, alone), was developed in the last decade. The aim of the combined treatment was to inject a smaller amount of CYA, thus reducing the risk for embolization.7
A 51-year-old man presented with gastric variceal bleeding (IGV 1) with hemodynamic decompensation refractory to endoscopic and hemodynamic therapy.
The patient was diagnosed with idiopathic cavernous transformation of the portal vein. The usual causes of portal thrombosis were ruled out.8 Multiple episodes of gastric variceal bleeding were treated endoscopically with B-CYA injection (1ml each session, 4 sessions) plus Lipiodol, achieving control of the acute bleeding, but not eradicating the varices.
During the fourth episode of bleeding, the patient was referred to our hospital. In accordance with the surgical expertise at our center, derivation through a mesocaval shunt was performed for treating prehepatic portal hypertension. Shunt thrombosis occurred one week after the intervention. The patient presented with variceal rebleeding, for which splenic artery embolization with coils was performed through angiography to decrease splenic circulation and the fundal variceal pressure (fig. 1).
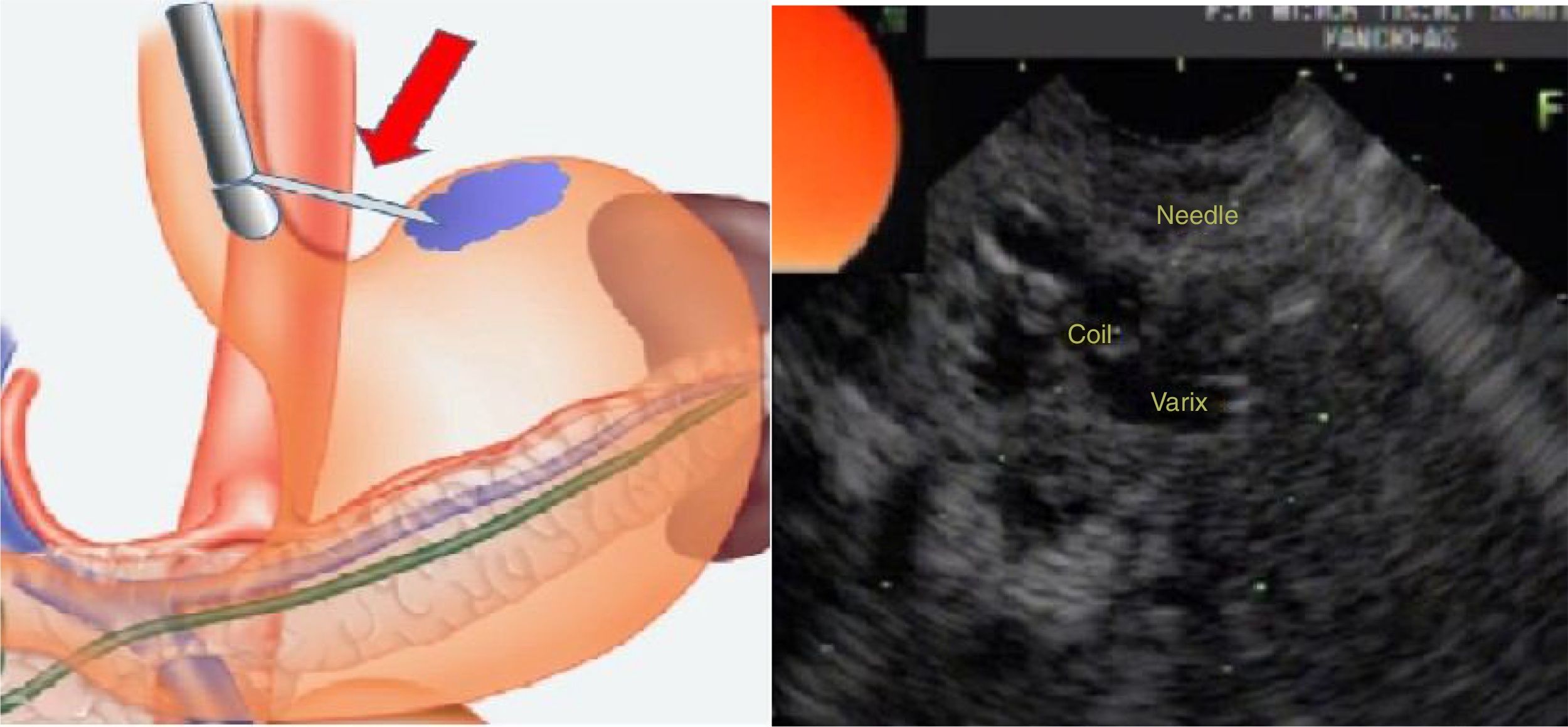
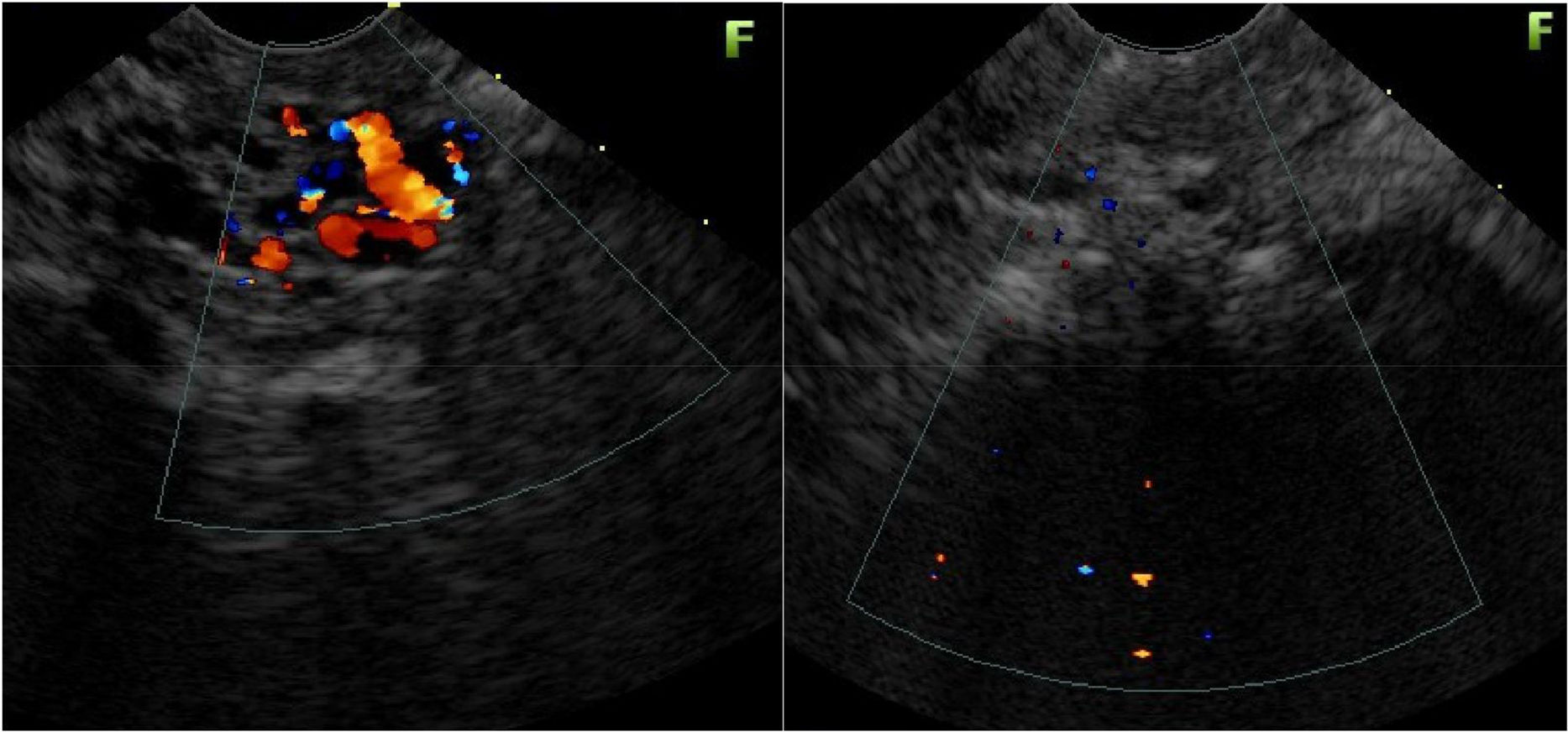
Endoscopic ultrasound therapy was carried out because of IGV-1 persistence and a new rebleeding episode. The largest IGV-1 (15mm in diameter) was chosen, using a linear or sector echoendoscope (Fujinon EG530 OUT, New Jersey, USA). The distal esophageal wall was punctured with a 19-gauge echoendoscopic needle (EchoTip Ultra, Cook Medical, Bloomington, Indiana, USA) until reaching the interior of the selected varix (fig. 2). The coil (MicroNester®, 10 mm-7cm, Cook Medical, Bloomington, Indiana, USA) was introduced, pushing the needle stylet under endosonographic vision. A mixture of B-CYA (1ml) and Lipiodol (1ml) was then injected. Doppler ultrasound was used to confirm the absence of blood flow at the interior of the treated varix after injection.
No complications were reported and the Doppler echoendoscopic control at 4 months showed gastric varix obliteration.
The treatment of choice for gastric variceal bleeding is endoscopic injection of CYA inside the varices. Doppler echoendoscopic monitoring ensures complete obliteration of the varices, reducing the possibilities of rebleed.9 Echoendoscopic-guided placement of stainless steel coils during the same session reduces the risk for systemic CYA embolization. The most widely-used coil in fundal varices is a spiraled coil with synthetic fibers adhered to the surface, which induce thrombosis, preventing CYA dispersion. The size of the coil employed is dependent on the size of the varix, and the most commonly used sizes are from 10 to 20mm in diameter. One or more coils can be introduced in each procedure.
Puncture is carried out through the distal esophagus to reduce the risk for bleeding because the thicker muscle layer of the esophageal wall collapses the puncture path.
The combination of coil and glue increases hemostasis, obliterates the fundal varices, and reduces the risk for embolization.9 In a randomized study on 32 patients, presented at the 2017 Digestive Disease Week, Chaves et al. concluded that the combined technique reduced the amount of cyanoacrylate needed to eradicate the lesions.10
Bhat et al.9 conducted a retrospective analysis of 152 patients with gastroesophageal varices type 2 (GEV-2) and IGV-1 with active bleeding (5% of the cases), secondary prophylaxis (69%), and primary prophylaxis (26%), with 99% technical success. The mean number of coils used was 1.4 (range: 1-4 coils) and the mean volume of O-CYA injected was 2ml (range: 0.5-6ml). Echoendoscopic control with Doppler was carried out on 100 patients that showed complete variceal obliteration in 93% of the subjects. Rebleed occurred in 8% of the patients with gastric varices and in 3% with esophageal varices. However, complete obliteration was observed in 3% of the cases. In regard to complications, only one patient presented with symptomatic pulmonary embolization.11
The combination of echoendoscopic-guided coil introduction and CYA injection as treatment of gastric roof varices is efficacious and safe and can be used when conventional treatment fails.
Comparative studies are needed to determine its role as first-line treatment in fundal variceal bleeding.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of dataThe authors declare that no patient data appear in this article.
Right to privacy and informed consentThe authors declare that no patient data appear in this article.
Financial disclosureNo financial support was received in relation to this article.
Conflict of interestThe authors declare that there is no conflict of interest.
Please cite this article as: Jer Hwang H, Málaga I, Curvale C, Guidi M, Matano R. Tratamiento ecoendoscópico con coil y N-butil-2-cianocrilato de hemorragia varicosa gástrica refractaria. Revista de Gastroenterología de México. 2019;84:108–110.