Metabolic (dysfunction) associated fatty liver disease (MAFLD) and gallstone disease are entities that share similar risk factors. Numerous publications confirm their elevated frequency, but few studies have considered their prevalence and possible association.
AimsTo determine the prevalence of MAFLD in patients with gallstone disease and the usefulness of liver biopsy for diagnosing the liver disease.
Materials and methodsA prospective study was conducted on patients that underwent laparoscopic cholecystectomy, in whom liver biopsy was performed.
Variables analyzedAnthropometric characteristics, biochemical profile, conventional ultrasound, risk factors, and histopathologic study of the liver biopsy.
Statistical analysisDescriptive statistics were carried out for the quantitative variables and the Student’s t test and multivariate analysis through binary logistic regression were employed for the continuous variables, utilizing IBM-SPSS, 25.0 (Windows) software.
ResultsA total of 136 patients were classified into 2 groups: 40 (29.41%) with normal liver and 96 (70.59%) with MAFLD. Of the 136 patients, 71 patients (52.21%) corresponded to hepatic steatosis, 21 (15.44%) to steatohepatitis, and 4 (2.94%) to cirrhosis. Perisinusoidal inflammation was found in 39 cases (28.68%) and fibrosis was found in 10 (7.35%). The risk factors for both groups were age, diabetes, high blood pressure, and obesity. Glucose, triglyceride, and aminotransferase levels were significantly higher in the MAFLD group and conventional ultrasound demonstrated moderate concordance for its detection.
Discussion and conclusionsThe results confirmed the elevated frequency of MAFLD associated with gallstone disease, justifying liver biopsy during cholecystectomy for diagnosing MAFLD.
La esteatosis hepática metabólica (EHMet) y la colelitiasis son entidades que comparten factores de riesgo similares. Numerosas publicaciones confirman su elevada frecuencia, sin embargo, pocos estudios han considerado su prevalencia y posible asociación.
ObjetivoDeterminar la prevalencia de EHMet en pacientes con colelitiasis y la utilidad de la biopsia hepática para el diagnóstico de la enfermedad.
Material y métodosEstudio prospectivo de pacientes sometidos a colecistectomía laparoscópica a los cuales se realizó biopsia hepática.
Variables analizadasCaracterísticas antropométricas, perfil bioquímico, ultrasonido convencional, factores de riesgo y estudio histopatológico de biopsia hepática.
Análisis estadísticoSe emplearon estadísticas descriptivas para variables cuantitativas y t de Student y análisis multivariado mediante regresión logística binaria para variables continuas, empleando el programa IBM-SPSS, 25.0 (Windows).
ResultadosCiento treinta y seis pacientes, clasificados en 2 grupos: hígado normal 40 (29.41%) y EHMet 96 (70.59%) de ellos 71 (52.21%) correspondieron a esteatosis hepática, 21 (15.44%) a esteatohepatitis y 4 (2.94%) a cirrosis. En 39 casos (28.68%) se encontró inflamación perisinusoidal y en 10 (7.35%) fibrosis. Los factores de riesgo para ambos grupos fueron edad, diabetes, hipertensión arterial y obesidad; los niveles de glucosa, triglicéridos y aminotransferasas fueron significativamente superiores en EHMet y el ultrasonido convencional fue un estudio de moderada concordancia para su detección.
Discusión y conclusionesLos resultados confirman la elevada frecuencia de EHMet asociada a colelitiasis por lo cual se justifica realizar la biopsia hepática durante la colecistectomía para establecer su diagnóstico.
Metabolic (dysfunction) associated fatty liver disease (MAFLD) has become one of the most frequent chronic liver diseases, with an estimated prevalence in the general adult population of 25-40%,1–4 increasing in the at-risk population to 62-84%, and whose natural progression conditions its advanced stages of cirrhosis and hepatocellular carcinoma.5–7 Because of its elevated prevalence and high morbidity and mortality rates, MAFLD is considered a public health problem that not only affects individual health and the family economy, but also greatly impacts healthcare costs worldwide.8–11 One of the most important risk factors is obesity, which has notably increased in Mexico. In 2019, obesity held second place in the adult population across the globe, as well as first place in childhood obesity, with a frequency of 15.7-42.1% in the general population.12–22
Likewise, gallstone disease has a high prevalence in productive-age women and shares similar risk factors with MAFLD, such as obesity, diabetes, high blood pressure, dyslipidemia, and multiparity.23–28
The relation between the two entities has been reported by different groups worldwide, but information in Mexico is scarce. Therefore, we decided to conduct the present study to determine their prevalence and possible association.29–32
Our aim was to determine the prevalence of MAFLD in patients with gallstone disease and the usefulness of liver biopsy in diagnosing MAFLD.
Materials and methodsA prospective, observational, and comparative study was carried out on patients diagnosed with symptomatic gallstone disease that underwent laparoscopic cholecystectomy and liver biopsy, within the time frame of January 2017 and March 2020, after having given their informed consent. They were seen at private hospitals in the city of Veracruz, in collaboration with the Department of Pathologic Anatomy at the Instituto de Investigaciones Médico-Biológicas of the Universidad Veracruzana. The study variables were age, sex, weight, height, body mass index (BMI), family history, and associated comorbidities (obesity, high blood pressure, diabetes mellitus, and number of pregnancies). The blood levels of hemoglobin, hematocrit, leukocytes, neutrophils, lymphocytes and platelets, glucose, blood urea nitrogen, urea, creatinine, total cholesterol, high density lipoprotein, direct bilirubin, indirect bilirubin, aspartate aminotransferase (AST), alanine aminotransferase (ALT), total protein, and albumin were analyzed, and the results of conventional ultrasound imaging were evaluated.
Inclusion criteria: patients of both sexes in whom hepatitis B and/or hepatitis C were ruled out and patients whose alcohol intake was below 150g/week.
Exclusion criteria: patients with gallstones, of both sexes, with positive viral markers for hepatitis B or hepatitis C, and patients whose alcohol intake was high.
Study universe: consecutive patients that underwent cholecystectomy due to gallstones.
Wedge biopsy of the liver was performed in segment 4 of the right lobe. The samples were fixed in 10% formaldehyde and underwent hematoxylin & eosin and Masson’s trichrome staining at the Department of Pathologic Anatomy of the Instituto de Investigaciones Médico-Biológicas. They were interpreted and classified according to the NAFLD Activity Score (NAS) proposed by Kleiner et al.33
Statistical analysis: the results were analyzed using the descriptive statistics of measures of central tendency and dispersion for the quantitative variables and using the Student’s t test and a multivariate analysis through binary logistic regression for the continuous variables. Statistical significance was set at a p of 0.05 and the IBM-SPSS version 25.0 for Windows software was employed.
Ethical considerations: the study was conducted according to the Declaration of Helsinki and the NOM-012-SSA3-2012, and the protocol was approved by the Bioethics and Research Committee of the Faculty of Medicine of the Universidad Veracruzana in Veracruz-Boca del Río.
ResultsA total of 142 patients diagnosed with gallstone disease that underwent laparoscopic cholecystectomy and liver biopsy were evaluated. Six of the patients were eliminated because they did not meet the inclusion criteria, leaving 136 patients to make up the study group. The mean age of the study patients was 50.85±15.28 years (range: 21-82) and there was a predominance of women (108 [79.40%]) over men (28 [20.60%]).
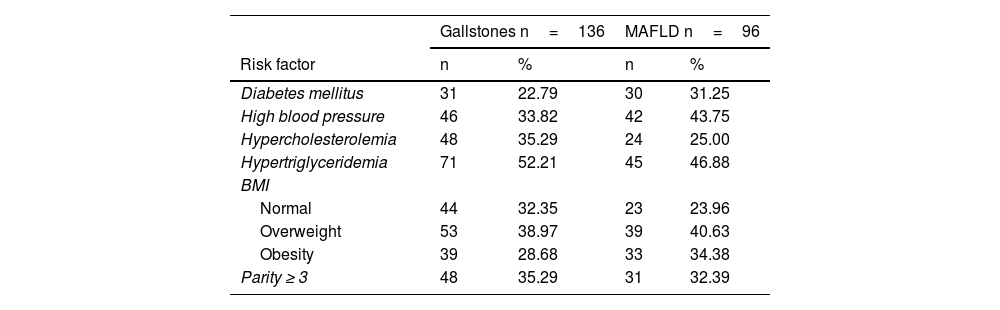
The risk factors found in the patients with gallstones were diabetes mellitus in 31 cases (22.79%), high blood pressure in 46 cases (33.82%), and dyslipidemia in 119 cases (87.5%); in relation to BMI, 97 patients (71.3%) presented with normal weight or overweight and 39 patients (28.68%) presented with obesity; and 48 women (35.29%) (range: 0-10) were multiparous (≥ 3 births). The risk factors in the MAFLD group were diabetes mellitus in 30 cases (31.25%), high blood pressure in 42 cases (43.75%), and dyslipidemia in 69 cases (71.88%); in relation to BMI, 62 patients (64.58%) presented with normal weight or overweight and 33 patients (34.38%) presented with obesity; 31 women (32.29%) were multiparous (≥ 3 births) (Table 1).
Risk factors in the study population with gallstones and metabolic (dysfunction) associated fatty liver disease.
| Gallstones n=136 | MAFLD n=96 | |||
|---|---|---|---|---|
| Risk factor | n | % | n | % |
| Diabetes mellitus | 31 | 22.79 | 30 | 31.25 |
| High blood pressure | 46 | 33.82 | 42 | 43.75 |
| Hypercholesterolemia | 48 | 35.29 | 24 | 25.00 |
| Hypertriglyceridemia | 71 | 52.21 | 45 | 46.88 |
| BMI | ||||
| Normal | 44 | 32.35 | 23 | 23.96 |
| Overweight | 53 | 38.97 | 39 | 40.63 |
| Obesity | 39 | 28.68 | 33 | 34.38 |
| Parity ≥ 3 | 48 | 35.29 | 31 | 32.39 |
BMI: body mass index; MAFLD: metabolic (dysfunction) associated fatty liver disease.
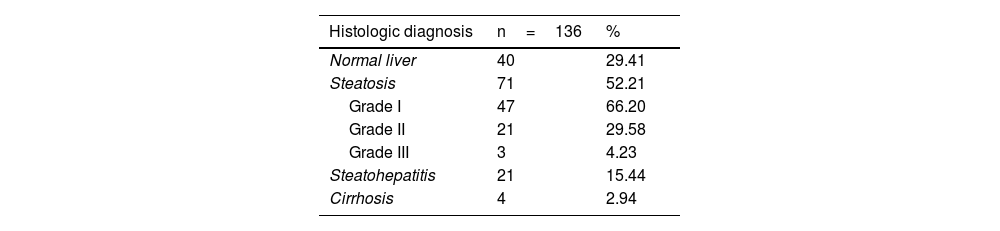
Based on the histologic findings in the liver biopsies, the patients were divided into 2 groups: group 1=40 patients (29.41%) with normal results and group 2=96 patients (70.59%) with MAFLD. The diagnoses in group 2 were hepatic steatosis in 71 cases (52.21%) (the majority of which were mild [66.20%]), steatohepatitis in 21 cases (15.44%), and cirrhosis in 4 cases (2.94%). In the patients with MAFLD, perisinusoidal inflammation was identified in 39 cases (28.68%), fibrosis in 10 cases (7.35%), and cirrhosis in 4 cases (2.94%) (Table 2).
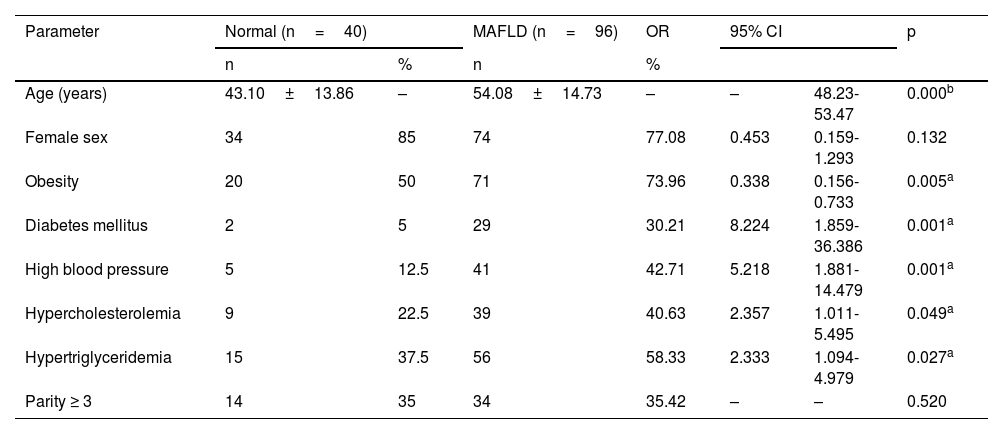
In order of frequency, the statistically significant risk factors for MAFLD were type 2 diabetes mellitus, high blood pressure, hypercholesterolemia, and hypertriglyceridemia; on the other hand, sex and obesity were shown to have an odds ratio (OR) of –1.0 as protective factors against MAFLD, and in relation to age in years, the mean age was significantly higher in the MAFLD group (p<0.05) (Table 3).
Anthropometric characteristics and risk factors of the study groups (group 1 [normal liver] and group 2 [MAFLD]).
| Parameter | Normal (n=40) | MAFLD (n=96) | OR | 95% CI | p | ||
|---|---|---|---|---|---|---|---|
| n | % | n | % | ||||
| Age (years) | 43.10±13.86 | – | 54.08±14.73 | – | – | 48.23-53.47 | 0.000b |
| Female sex | 34 | 85 | 74 | 77.08 | 0.453 | 0.159-1.293 | 0.132 |
| Obesity | 20 | 50 | 71 | 73.96 | 0.338 | 0.156-0.733 | 0.005a |
| Diabetes mellitus | 2 | 5 | 29 | 30.21 | 8.224 | 1.859-36.386 | 0.001a |
| High blood pressure | 5 | 12.5 | 41 | 42.71 | 5.218 | 1.881-14.479 | 0.001a |
| Hypercholesterolemia | 9 | 22.5 | 39 | 40.63 | 2.357 | 1.011-5.495 | 0.049a |
| Hypertriglyceridemia | 15 | 37.5 | 56 | 58.33 | 2.333 | 1.094-4.979 | 0.027a |
| Parity ≥ 3 | 14 | 35 | 34 | 35.42 | – | – | 0.520 |
CI: confidence interval; MAFLD: metabolic (dysfunction) associated fatty liver disease; OR: odds ratio.
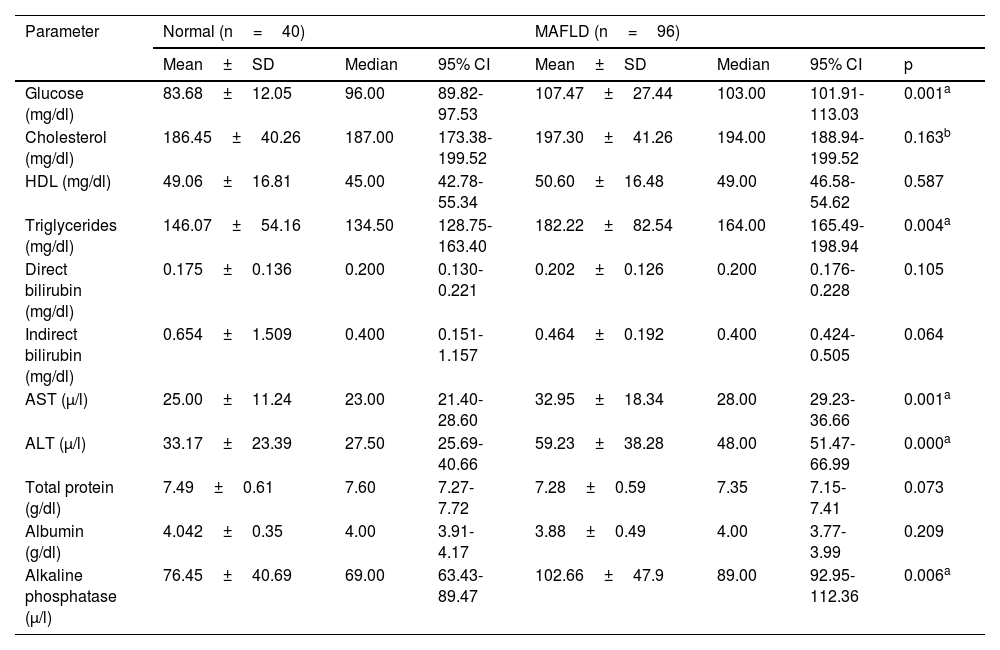
In relation to the biochemical profile, the serum levels of glucose, triglycerides, AST, ALT, and alkaline phosphatase were significantly higher in the MAFLD patients than in the patients with normal results (p<0.05); in some parameters, such as indirect bilirubin and total protein, their values were slightly higher, but not statistically significant (Table 4).
Biochemical profile of the group 1 (normal liver) and group 2 (MAFLD) patients.
| Parameter | Normal (n=40) | MAFLD (n=96) | |||||
|---|---|---|---|---|---|---|---|
| Mean±SD | Median | 95% CI | Mean±SD | Median | 95% CI | p | |
| Glucose (mg/dl) | 83.68±12.05 | 96.00 | 89.82-97.53 | 107.47±27.44 | 103.00 | 101.91-113.03 | 0.001a |
| Cholesterol (mg/dl) | 186.45±40.26 | 187.00 | 173.38-199.52 | 197.30±41.26 | 194.00 | 188.94-199.52 | 0.163b |
| HDL (mg/dl) | 49.06±16.81 | 45.00 | 42.78-55.34 | 50.60±16.48 | 49.00 | 46.58-54.62 | 0.587 |
| Triglycerides (mg/dl) | 146.07±54.16 | 134.50 | 128.75-163.40 | 182.22±82.54 | 164.00 | 165.49-198.94 | 0.004a |
| Direct bilirubin (mg/dl) | 0.175±0.136 | 0.200 | 0.130-0.221 | 0.202±0.126 | 0.200 | 0.176-0.228 | 0.105 |
| Indirect bilirubin (mg/dl) | 0.654±1.509 | 0.400 | 0.151-1.157 | 0.464±0.192 | 0.400 | 0.424-0.505 | 0.064 |
| AST (μ/l) | 25.00±11.24 | 23.00 | 21.40-28.60 | 32.95±18.34 | 28.00 | 29.23-36.66 | 0.001a |
| ALT (μ/l) | 33.17±23.39 | 27.50 | 25.69-40.66 | 59.23±38.28 | 48.00 | 51.47-66.99 | 0.000a |
| Total protein (g/dl) | 7.49±0.61 | 7.60 | 7.27-7.72 | 7.28±0.59 | 7.35 | 7.15-7.41 | 0.073 |
| Albumin (g/dl) | 4.042±0.35 | 4.00 | 3.91-4.17 | 3.88±0.49 | 4.00 | 3.77-3.99 | 0.209 |
| Alkaline phosphatase (μ/l) | 76.45±40.69 | 69.00 | 63.43-89.47 | 102.66±47.9 | 89.00 | 92.95-112.36 | 0.006a |
ALT: alanine aminotransferase; AST: aspartate aminotransferase; CI: confidence interval; HDL: high density lipoprotein; SD: standard deviation.
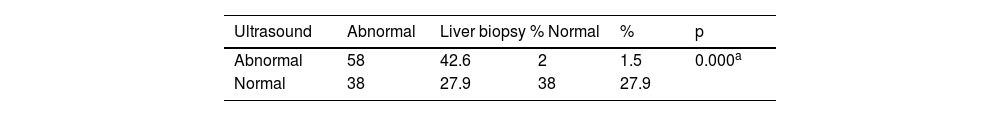
Conventional ultrasound imaging results in the subjects with a histologic diagnosis of normal liver showed no alterations in 38 cases (95.0%) and identified alterations suggestive of MAFLD in 2 cases (5.9%), whereas in the cases with a histologic diagnosis of MAFLD, 38 cases (53.52%) were reported as normal and 33 (46.48%) were suggestive of steatosis, with a Cohen’s kappa coefficient of 0.44 and a 95% CI of 0.29-0.59, revealing moderate diagnostic concordance and only a total level of good concordance of 0.71 (Table 5).
Concordance between patients with a histologically normal liver, patients with MAFLD, and conventional ultrasound findings.
| Ultrasound | Abnormal | Liver biopsy % Normal | % | p | |
|---|---|---|---|---|---|
| Abnormal | 58 | 42.6 | 2 | 1.5 | 0.000a |
| Normal | 38 | 27.9 | 38 | 27.9 | |
MAFLD is a chronic progressive disease characterized by abnormal fat accumulation that presents in persons that consume fewer than 20g of alcohol daily, and in persons in whom other causes have been ruled out, such as medications, iron metabolism alterations, viral infections, and causes secondary to bariatric surgery and malnutrition. The broad spectrum of MAFLD includes simple steatosis, steatohepatitis, cirrhosis of the liver, and hepatocellular carcinoma,15,26and it has become one of the most common causes of chronic liver disease. It affects one-fourth of the world population (14-35%),15–18 with variations in different regions. The highest rates are in Western Europe and the United States, where differences between diverse social groups have been found (45% in Hispanics, 33% in Whites, and 24% in African Americans).1,5,34,35 A significant increase is estimated worldwide in the coming decades. By 2030 it is calculated to reach 24.6% in Japan, 26.2% in China, 43% in Germany, and 49% in Spain.36–38 Isolated reports in Latin America show a prevalence of 17-33% in the general population, similar to that of the rest of the world,20,39,40 describing an increase to 44% in patients with overweight and obesity that underwent liver biopsy.38 In Mexico, the reported prevalence of MAFLD varies, depending on the population studied and the methodology employed for its detection. At the beginning of the year 2000, prevalence was reported at 4.6-15.7% in population studies,16–19 whereas through conventional ultrasound imaging, prevalence was 28.65% in subjects above 18 years of age.20,21 Recently, in a population study conducted by Bernal-Reyes et al. that included 585 individuals above 18 years of age from different regions of Mexico, prevalence was 42.1%.22
On the other hand, gallstone disease has a high prevalence worldwide, estimated to present in 8 to 11% of the adult population. The highest incidence is in White adults (8-15%) in reports from Austria, Germany, Spain, Switzerland, and the United States, describing approximately 600,000 new cases annually; incidence is intermediate (3-8%) in the United Kingdom, Germany, Japan, Ireland, Norway, and New Zealand; and incidence is low (0.8-3%) in Blacks and in Asian countries.39,40 Rates in Argentina, Bolivia, and Chile have been reported to be similar to those in the United States, and prevalence in Latin America, including Mexico, is 5-15%.41–44 In the present study, 70.59% of the patients with gallstone disease had histologic alterations characterized as MAFLD and 29.41% had normal liver, which are higher figures than those reported in population studies or ultrasound findings. They are also higher than the results of a similar study conducted by Ramos-de la Medina et al. in 2008 that reported gallstones in only 45% of the cases.32 Likewise, steatosis was the predominant clinical disease, presenting in 52.21% of the patients, whereas 15.44% of the cases corresponded to steatohepatitis, and 2.94% to cirrhosis (Table 3).
In a meta-analysis conducted in 2016, Shabanzadeh et al. established the fact that there are risk factors implicit in gallstone disease that are difficult to modify, such as age, predominance of female sex over male sex (at a ratio of 4.3:1), and genetic alterations in indigenous groups in the United States and Eastern Asia.45–47 In our group of patients with gallstone disease, the mean age was 54.08±14.7 years, higher than the 43.10±13.86 years of age of the patients with normal weight (95% CI: 48.23-53.47 and p=0.0000). There was a predominance of women (79.4%) over men (20.6%) The majority of women were married (77.9%) and were housewives (54.4%). High blood pressure, diabetes, obesity, dyslipidemia, and multiparity,48–52 as well as gallbladder stasis and bacterial permeation,53–56 were associated with gallbladder disease.
In our study, approximately 90% of the patients diagnosed with MAFLD had at least one of the components of metabolic syndrome and 30% met 3 of its diagnostic criteria, conferring upon that group an 11-times higher risk for presenting with obesity, type 2 diabetes, and high blood pressure, compared with the normal weight patients (p<0.05). Even though hypertriglyceridemia and multiparity were also higher in that group, they did not reach statistical significance, similar to that reported in the international literature. In relation to the frequency of MAFLD with sex, it was higher in women (74 cases, 77.08%) than in men (22 cases, 22.92%), (p=0.168).
In the initial phases of MAFLD, the clinical data are scarce and nonspecific, and its diagnosis tends to be incidental, upon finding elevated aminotransferases or minimal changes identified through conventional ultrasound and liver function tests. Therefore, the 2019 Mexican Consensus on NAFLD by the Asociación Mexicana de Gastroenterología and the Asociación Mexicana de Hepatología recommend their performance as screening methods directed at the high-risk population, in particular, patients with one or more components of metabolic syndrome.57 In our case series the AST values in the healthy liver were 25.00±11.24 μ/l (95% CI: 21.40-28.60) vs. 32.95±18.34 μ/l (95% CI: 29.23-36.66) in MAFLD (p=0.001), and the ALT values were 33.17±23.39u/l (95% CI: 21.40-28.60) vs. 59.23±38.28 μ/l (95% CI: 51.47-66.99), respectively (p=0.000). Conventional ultrasound had moderate concordance for detecting steatosis in our series.
The biochemical profile of lipids and liver function tests in the patients with MAFLD showed significantly higher levels of glucose, triglycerides, and alkaline phosphatase, compared with the patients with normal liver (p<0.05), whereas the levels of direct bilirubin, indirect bilirubin, total protein, and albumin showed no statistical significance between the two groups.
In our study, ultrasound imaging had a concordance of 42.6% with the abnormal liver and a total level of concordance of 0.71, p≤0.000, with a kappa index of 0.41 and a 95% CI of 0.29-0.59, which we considered moderate, in relation to the histopathologic findings.
ConclusionsOur results demonstrated an elevated prevalence of MAFLD in patients that presented with cholelithiasis between the fourth and sixth decades of life, and even though there were a majority of women in the MAFLD and normal liver groups, the risk for gallstone disease was slightly predominant in men.
MAFLD and gallstone disease share risk factors and biochemical behavior, such as components of metabolic syndrome.
Even though liver biopsy is not exempt from morbidity and mortality, the possibility of bleeding and the need for its control under direct vision is reduced to a minimum. Therefore, we believe that the surgical treatment of cholelithiasis can be performed simultaneously with liver biopsy, given that the surgical procedure is safe, efficacious, and relatively inexpensive and liver biopsy is the gold standard in diagnosing MAFLD.
Financial disclosureThe study was carried out utilizing funds from the participating institutions.
Conflict of interestDr. José María Remes Troche is a consultant and speaker for the Asofarma and Takeda laboratories.
The rest of the authors have no conflict of interest.
Please cite this article as: Roesch-Dietlen F, Pérez-Morales AG, Grube-Pagola P, González-Santes M, Díaz-Roesch F, Triana-Romero A, Roesch-Ramos L, Remes-Troche JM, Cruz-Aguilar M. Prevalencia de la esteatosis hepática metabólica (EHMet) en pacientes con litiasis vesicular. Estudio de una cohorte de casos en el sur-sureste de México. Rev Gastroenterol Méx. 2023;88:225–231.