Any alarm symptoms in patients with irritable bowel syndrome (IBS) should be carefully evaluated. Colonoscopy is a standard diagnostic procedure for evaluating the colonic mucosa and ruling out probable diseases responsible for patient symptoms. We analyzed the colonoscopy findings in patients with and without IBS.
Material and methodsNinety-six patients with IBS and 101 without IBS were consecutively enrolled in the study. All the patients in the IBS group met the Rome IV criteria, and underwent colonoscopy due to the appearance of red flags. The colonoscopy findings were compared between the 2 groups of patients.
ResultsThe main indications for colonoscopy in the IBS group were progressive abdominal pain (36.7%), rectal bleeding with fresh blood (17.7%), and occult blood in stool (12.5%). In the non-IBS group, the most prevalent indicators were rectal bleeding with fresh blood (37.6%), colorectal cancer surveillance (21.8%), and abdominal pain (13.9%). The most common macroscopic findings in the 2 groups were hemorrhoids, polyps, and anal fissure. There were no statistically significant differences with respect to the microscopic and macroscopic findings between groups.
ConclusionsWe concluded that the prevalence of organic lesions in the colon of patients with IBS was the same as that in the patients without IBS. The Rome IV criteria accurately predicted IBS. Additional evaluation through colonoscopy in IBS should be based on the presence of alarm features.
Cualquier síntoma alarmante debe evaluarse cuidadosamente en los pacientes con síndrome del intestino irritable (SII). La colonoscopia es un procedimiento de diagnóstico estándar para evaluar la mucosa del colon y descartar probables enfermedades responsables de los síntomas de los pacientes. Analizamos los hallazgos colonoscópicos en pacientes con SII y pacientes sin SII.
Material y métodosNoventa y seis pacientes con SII y 101 sin SII fueron registrados en el estudio de forma consecutiva. Todos los pacientes del grupo con SII cumplieron los criterios de Roma IV y se sometieron a una colonoscopia debido a la aparición de signos alarmantes. Los hallazgos de la colonoscopia se compararon entre los grupos de pacientes.
ResultadosLos principales indicadores para colonoscopia en el grupo con SII fueron dolor abdominal progresivo (36.7%), sangrado rectal fresco (17.7%) y sangre oculta en heces (12.5%). En el grupo sin SII, los indicadores de mayor prevalencia fueron sangrado rectal fresco (37.6%), vigilancia del cáncer colorrectal (21.8%) y dolor abdominal (13.9%). En ambos grupos, los hallazgos macroscópicos más comunes fueron hemorroides, pólipos y fisura anal. No hubo diferencias estadísticamente significativas entre los grupos en los hallazgos macroscópicos y microscópicos.
ConclusionesConcluimos que la prevalencia de lesiones orgánicas en el colon de pacientes con SII es la misma que en pacientes sin SII. Los criterios de Roma IV predijeron el SII con precisión. La evaluación colonoscópica adicional en el SII debe basarse en la presencia de signos de alarma.
Irritable bowel syndrome (IBS) is the most common of the functional gastrointestinal disorders (FGIDs).1 A recent review has shown that the mean prevalence of IBS varies widely, ranging from 1.1% in Iran and France to 35.5% in Mexico.2,3 However, different reports on IBS frequency in the Iranian population revealed that the prevalence of IBS is between 1.1 and 25%. The wide discrepancy may be due to differences in population cohorts or inconsistency in socioeconomic and cultural status.4
Colonoscopy is not a routine diagnostic modality in IBS. The British guidelines do not suggest routine colonoscopy in adults that meet the IBS diagnostic criteria.5 Likewise, the American College of Gastroenterology does not recommend routine colonoscopy in patients under 45 years of age, with IBS symptoms and no alarm signs.6 Recent clinical trials in patients fulfilling the Rome III criteria, with no alarm features, have shown that a positive diagnostic strategy with limited blood tests is similar in safety, compared with a rule-out strategy that employs extensive laboratory testing and sigmoidoscopy.7 However, most patients with symptoms consistent with IBS and warning signs are referred for colonoscopy, to rule out organic diseases, such as inflammatory bowel disease (IBD) and colorectal cancer (CRC).8
AimTo the best of our knowledge, there have been no studies comparing colonoscopy findings and mucosal lesions in IBS patients and controls in Iran. The aim of the present study was to compare organic lesions between IBS and non-IBS patients.
Materials and methodsStudy design and populationThe present study was prospectively conducted from April to September 2018 at an academic referral center affiliated with the Shiraz University of Medical Sciences, Shiraz, Iran. The study population was made up of the IBS group and the non-IBS group. The IBS group, consecutively enrolled in the study, were patients that met the Rome IV9 inclusion criteria, but presented with alarm signs. They underwent colonoscopy to rule out organic lesions and corroborate the diagnosis of IBS. Colonoscopy indications were the presence of progressive pain, weight loss, rectal bleeding with fresh blood, occult blood in the stool, abnormal laboratory results, or any other alarm sign. The non-IBS group, also consecutively enrolled in the study, were patients that had an indication for colonoscopy.
The exclusion criteria in both groups were oliguric renal failure, severe congestive heart failure, immobilized patients, confirmed hypomotility of the colon, and refusal to participate in the study tests and examinations.
Demographic data were collected. Standard bowel preparation protocol consisted of polyethylene glycol solution, senna syrup, and bisacodyl tablets.
Statistical analysisThe Statistical Package for the Social Sciences (SPSS®) version 16 was used for the data analysis. An independent t-test was employed to compare means, and the chi-square and Fisher's exact tests were used for the categorical variables. A p value below 0.05 was considered statistically significant.
Ethical considerationsThe local ethics committee of the Shiraz University of Medical Sciences approved the study protocol (IR.SUMS.MED.REC.1396.103). Written informed consent was obtained from each of the study patients.
ResultsOf the 208 patients, 11 were excluded due to a history of severe congestive heart failure and oliguric renal failure. The IBS group included 96 patients, the majority of whom were males (55.2%), with a mean age in years (± SD) of 43.23 (± 12.69). Of the 101 patients in the non-IBS group, 63.3% were females, with a mean age in years (± SD) of 47.66 (± 14.11). There was no significant difference in mean age between the two groups (p=0.595).
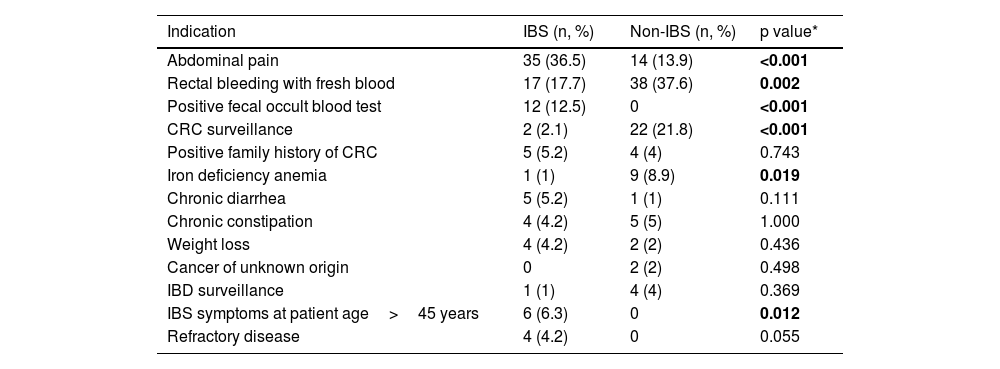
The main indications for colonoscopy in the IBS group were abdominal pain, rectal bleeding with fresh blood, and a positive fecal occult blood test. Patients in the non-IBS group mainly underwent colonoscopy due to rectal bleeding with fresh blood, CRC surveillance, and abdominal pain (Table 1).
The most common indications for colonoscopy in the IBS and non-IBS groups.
| Indication | IBS (n, %) | Non-IBS (n, %) | p value* |
|---|---|---|---|
| Abdominal pain | 35 (36.5) | 14 (13.9) | <0.001 |
| Rectal bleeding with fresh blood | 17 (17.7) | 38 (37.6) | 0.002 |
| Positive fecal occult blood test | 12 (12.5) | 0 | <0.001 |
| CRC surveillance | 2 (2.1) | 22 (21.8) | <0.001 |
| Positive family history of CRC | 5 (5.2) | 4 (4) | 0.743 |
| Iron deficiency anemia | 1 (1) | 9 (8.9) | 0.019 |
| Chronic diarrhea | 5 (5.2) | 1 (1) | 0.111 |
| Chronic constipation | 4 (4.2) | 5 (5) | 1.000 |
| Weight loss | 4 (4.2) | 2 (2) | 0.436 |
| Cancer of unknown origin | 0 | 2 (2) | 0.498 |
| IBD surveillance | 1 (1) | 4 (4) | 0.369 |
| IBS symptoms at patient age>45 years | 6 (6.3) | 0 | 0.012 |
| Refractory disease | 4 (4.2) | 0 | 0.055 |
CRC: colorectal cancer; IBD: inflammatory bowel disease; IBS: irritable bowel syndrome.
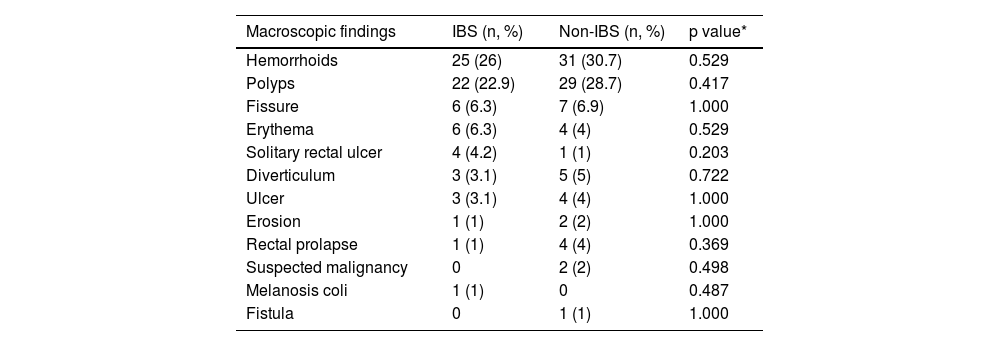
The most common macroscopic findings in the colonoscopy reports of the two groups were hemorrhoids, polyps, and fissure, respectively (Table 2).
Macroscopic findings from the colonoscopy reports in the IBS and non-IBS groups.
| Macroscopic findings | IBS (n, %) | Non-IBS (n, %) | p value* |
|---|---|---|---|
| Hemorrhoids | 25 (26) | 31 (30.7) | 0.529 |
| Polyps | 22 (22.9) | 29 (28.7) | 0.417 |
| Fissure | 6 (6.3) | 7 (6.9) | 1.000 |
| Erythema | 6 (6.3) | 4 (4) | 0.529 |
| Solitary rectal ulcer | 4 (4.2) | 1 (1) | 0.203 |
| Diverticulum | 3 (3.1) | 5 (5) | 0.722 |
| Ulcer | 3 (3.1) | 4 (4) | 1.000 |
| Erosion | 1 (1) | 2 (2) | 1.000 |
| Rectal prolapse | 1 (1) | 4 (4) | 0.369 |
| Suspected malignancy | 0 | 2 (2) | 0.498 |
| Melanosis coli | 1 (1) | 0 | 0.487 |
| Fistula | 0 | 1 (1) | 1.000 |
IBS: irritable bowel syndrome.
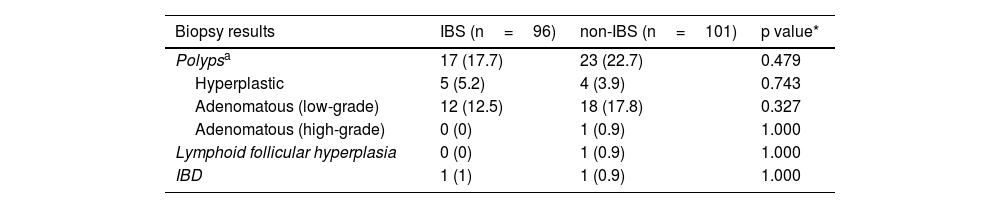
The normal/total percentage of biopsies taken from the IBS and non-IBS groups were 71/89 (79.7%) and 33/58 (56.8%), respectively. Table 3 shows the frequency of pathologic biopsies in both groups. No statistically significant difference was observed between the groups, regarding the prevalence of polyps.
Frequency of pathologic biopsies in the IBS and non-IBS groups.
| Biopsy results | IBS (n=96) | non-IBS (n=101) | p value* |
|---|---|---|---|
| Polypsa | 17 (17.7) | 23 (22.7) | 0.479 |
| Hyperplastic | 5 (5.2) | 4 (3.9) | 0.743 |
| Adenomatous (low-grade) | 12 (12.5) | 18 (17.8) | 0.327 |
| Adenomatous (high-grade) | 0 (0) | 1 (0.9) | 1.000 |
| Lymphoid follicular hyperplasia | 0 (0) | 1 (0.9) | 1.000 |
| IBD | 1 (1) | 1 (0.9) | 1.000 |
IBD: inflammatory bowel disease; IBS: irritable bowel syndrome.
Since the 1980s, various symptom-based criteria have been developed by gastroenterologists, for diagnosing IBS. Those criteria aim to decrease extensive and unnecessary testing for making the IBS diagnosis. The Rome IV criteria were introduced in 2016 and are now the gold standard for diagnosing IBS.10 In that setting, the physician needs to consider alarm features and rule out selected organic diseases. Important alarm features are symptom onset after 45 years of age, severe or worsening abdominal pain or other recent symptoms, rectal bleeding with fresh blood or melena, unexplained weight loss, nocturnal symptoms, iron deficiency anemia, and a family history of specific structural diseases, such as CRC, IBD, or celiac disease.
Further evaluation of individuals presenting with alarm features is recommended, particularly through colonoscopy.3,11,12 About one-third of individuals suffering from IBS are estimated to undergo colonoscopy during their clinical assessment.13 Notably, most diagnostic evaluations eventually have a negative result, and additional work-up rarely changes the diagnosis in patients meeting the Rome criteria.14 Thus, it is crucial to have negative clinical and paraclinical results in patients with warning signs.12 Lieberman et al. reported that IBS evaluation was one of the most common reasons for performing colonoscopy in patients<50 years of age.15
Undiagnosed underlying IBD is a matter of concern in IBS cases. We found that only 1% of the IBS patients were ultimately diagnosed with IBD, and the result was the same in the controls. Differentiation between IBS and IBD can be challenging because of their shared symptoms, such as abdominal pain and a change in bowel habits. Evidence suggests that patients usually present with IBS-like symptoms before IBD diagnosis. Moreover, those symptoms are more common in IBD patients.16,17 In a prospective study comparing controls and non-constipated IBS cases, regarding the prevalence of organic colonic lesions, those authors concluded that less than 1% of the IBS patients, and none of the controls, were finally diagnosed with IBD, results that are comparable to ours. However, it should be noted that routine colonoscopy is no longer recommended in IBS patients that do not present with alarm signs. At present, IBD screening with non-invasive biomarkers may be justified and practical. For instance, measuring the fecal calprotectin level can predict intestinal inflammation and is cost-effective and beneficial in adults.18 The fecal calprotectin cutoff level of<40μg/g and C-reactive protein cutoff level of<0.5mg/dl can rule out IBD in IBS patients. Likewise, the addition of fecal calprotectin and CRP may enhance the reliability of IBS symptom-based diagnoses.19
Missing CRC in IBS patients is always a major concern at the healthcare services. In the present study, neither the IBS patients nor the controls were finally diagnosed with CRC. That result is consistent with the data in previously published articles. In a recent case-control study in Taiwan, IBS did not increase the incidence of CRC, during 10 years of follow-up. However, there was a notable exception to that general pattern during the first 2 years, especially in the first 3 months, when a significant association was observed between IBS and CRC.20
Similarly, a study in Denmark revealed no significant association between IBS and CRC over a decade of follow-up, except in the first 3 months.21 In a similar population-based investigation, Rodriguez et al. concluded that the increased risk of CRC was observed only in the first year after IBS diagnosis.22 There appears to be a strong and positive correlation between IBS and CRC, within the first year of IBS diagnosis. The similarity of colon cancer symptoms to IBS symptoms has been suggested to possibly lead to primary IBS misdiagnosis.20,22
CRC is the third most commonly occurring cancer worldwide.23 Approximately 80% of CRC develops from chromosomal instability. Adenomatous polyps are considered primary lesions that are eventually transformed into CRC by extensively alternating chromosomes, aberrantly activating growth-promoting pathways, and suppressing apoptosis.24 Adenomatous polyps may progress to cancer over 10, or even 15, years.25 In our study, the prevalence of adenomatous polyps in the right colon of the non-IBS patients was higher, compared with the IBS patients. The progression to CRC of proximal polyps or large adenomas (≥ 20mm) has also been shown to be significantly higher, compared with the general population.26 Polyp distribution was similar in the transverse and left colon of patients in our two study groups. Interestingly, similar research results have indicated that the prevalence of several polyps in IBS patients is lower than in controls.15,27 In summary, the present study demonstrated that the prevalence of organic colonic lesions in the IBS patients and the non-IBS patients was in the same range. It should be underlined that the predictive value of the Rome IV criteria for diagnosing IBS is acceptable. Further evaluation via colonoscopy in IBS should be based on the presence of alarm features.
In conclusion, to the best of our knowledge, this is the first study to evaluate organic lesions in the Iranian population. We compared colonic lesions in IBS and non-IBS patients that underwent colonoscopy examinations. We found that the prevalence of structural lesions of the colon in patients meeting the Rome IV criteria was not noticeably different from that in other patients. The present result emphasizes the acceptability of the predictive value of the Rome IV criteria for diagnosing IBS.
Financial disclosureThis study was part of a thesis submitted to the school of medicine. The vice chancellor for research at the Shiraz University of Medical Sciences financially supported the study (grant No. 1397-01-01-17970).
Conflict of interestThe authors declare that there is no conflict of interest.
The authors wish to thank the Shiraz University of Medical Sciences and the Center for Development of Clinical Research of the Nemazee Hospital, as well as Dr. Nasrin Shokrpour, for her editorial assistance.
Please cite this article as: Ejtehadi F, Anbardar MH, Imanieh MH, Niknam R, Sivandzadeh GR. Lesiones colónicas orgánicas en pacientes con síndrome del intestino irritable: un estudio comparativo. Rev Gastroenterol Méx. 2023;88:208–213.