Choledocholithiasis presents in 5-10% of the patients with biliary lithiasis. Numerous treatment algorithms have been considered for this disease, however, up to 10% of these therapeutic procedures may fail. Intraoperative choledochoscopy has become a useful tool in the treatment of patients with difficult-to-manage choledocholithiasis.
ObjectivesTo determine the usefulness of intraoperative choledochoscopy in the laparoendoscopic treatment of difficult stones that was carried out in our service.
Patients and methodsA cross-sectional study was conducted. The case records were reviewed of the patients that underwent intraoperative choledochoscopy during biliary tree exploration plus laparoscopic choledochoduodenal anastomosis within the time frame of March 1, 2011 and May 31, 2012, at the Hospital General Dr. Manuel Gea González. Transabdominal choledochoscopies were performed with active stone extraction when necessary, followed by peroral choledochoscopies through the recently formed bilioenteric anastomosis. The data were analyzed with descriptive statistics and measures of central tendency.
ResultsThe mean age was 71 years, 57% of the patients were women, and the ASA III score predominated. Active extraction of stones with 7 to 35mm diameters was carried out in 4 of the cases and the absence of stones in the biliary tract was corroborated in all the patients. The mean surgery duration was 18minutes (range: 4 to 45min).
ConclusionsCholedochoscopy is a safe and effective minimally invasive procedure for the definitive treatment of difficult stones.
La coledocolitiasis se presenta en el 5 al 10% de los pacientes con colecistitis litiásica. Se han considerado múltiples algoritmos de tratamiento para esta afección; sin embargo, hasta el 10% de estos procedimientos terapéuticos pueden ser fallidos. La coledocoscopia transoperatoria se ha convertido en una herramienta útil en el tratamiento de pacientes con coledocolitiasis de difícil manejo.
ObjetivosDeterminar la utilidad de la coledocoscopia transoperatoria en el tratamiento laparo-endoscópico de litos difíciles en nuestro servicio.
Pacientes y métodosSe realizó un estudio transversal, en el que se revisaron los expedientes de los pacientes sometidos a coledocoscopia transquirúrgica durante exploración de la vía biliar más coledocoduodeno-anastomosis laparoscópica, en el periodo comprendido entre el 1 de marzo del 2011 y el 31 de mayo del 2012 en el Hospital General Dr. Manuel Gea González. Se realizaron coledocoscopias transabdominales, con extracción activa de litos en caso necesario, y posteriormente coledocoscopias transorales a través de la anastomosis bilioentérica recién formada. Se analizaron los datos con estadística descriptiva y medidas de tendencia central.
ResultadosLa edad promedio fue de 71 años, 57% mujeres, con predominio de puntuación ASA III. Se realizó la extracción activa de litos con diámetros de 7 a 35mm en 4 de los casos y en el total se corroboró ausencia de litos en la vía biliar. La duración promedio del procedimiento fue de 18 min (rango 4 a 45min).
ConclusionesLa coledocoscopia es un procedimiento eficaz y seguro para el tratamiento definitivo de los litos difíciles, en el ámbito de los procedimientos de invasión mínima.
Choledocholithiasis presents in 5 to 10% of patients with biliary lithiasis and up to 18% of patients with biliary pancreatitis. An estimated 21 to 34% of the stones spontaneously migrate from the biliary tract and up to 25 to 36% carry the risk for causing pancreatitis or cholangitis if they become obstructed. Numerous treatment algorithms have been considered, such as endoscopic retrograde cholangiopancreatography (ERCP) prior to cholecystectomy, intraoperative ERCP and postoperative ERCP. However, 5 to 10% of these procedures may fail due to access difficulty or stone extraction impossibility. Stones that are regarded as difficult are those that are larger than 15mm, that cannot be trapped in a basket, stones that are located in the intrahepatic biliary tract, those associated with chronic biliary tract stricture, stones that are present in patients that have undergone surgeries modifying the continuity of the proximal digestive tract (Billroth II gastrectomy or gastric bypass), and those in patients with Mirizzi syndrome.1 These conditions dramatically reduce the possibility of minimally invasive therapies. For instance, residual stones have been reported in 5 to 14% of the cases managed with laparoscopic biliary tract exploration. 1–3
Choledochoscopy was described for the first time in 1891 by Bakes, who designed a rigid instrument with a valve and a mirror that used a frontal light source for seeing inside the bile ducts. It was not until 1941 that McIver described a rigid optic choledochoscope equipped with an irrigation channel and an external light source. In 1965, the American Cystoscope Makers introduced the first flexible choledochoscope into the market.4
Today, intraoperative choledochoscopy has become a useful tool in the intraoperative treatment of patients with difficult-to-manage choledocholithiasis that undergo biliary tract exploration. 5–7 It enables direct visualization of the stone and its active extraction with the help of balloons and baskets. In addition, it is indispensible for corroborating the absence of stones, once the procedure is over, thus ensuring 0% of residual stones. 8–11
The aim of this study was to determine the usefulness of intraoperative choledochoscopy in the laparoendoscopic treatment of difficult stones.
MethodsA cross-sectional study was conducted that reviewed the case records of patients that had undergone intraoperative choledochoscopy during biliary tract exploration plus laparoscopic choledochoduodenal anastomosis (LCDA) within the time frame of March 1, 2011 and May 31, 2012 at the Hospital General Dr. Manuel Gea González.
All the patients were admitted to the General and Endoscopic Surgery Division having had previous ERCP, with one or more of the following events: failed ERCP, choledocholithiasis recurrence, persistent cholestasis secondary to biliary tract dilation, and repeat cholangitis.
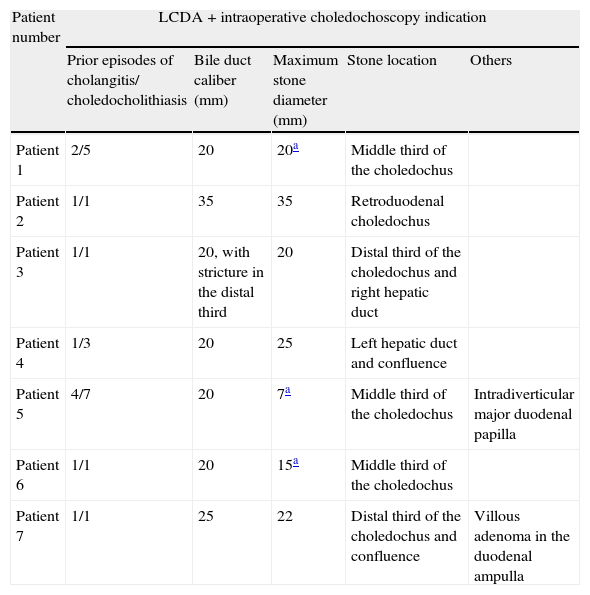
For these reasons, the surgical team decided to perform LCDA. Table 1 shows a summary of the indications for this surgical procedure in these patients.
Characteristics of the biliary tract and choledochoduodenal anastomosis indications in the patients.
| Patient number | LCDA + intraoperative choledochoscopy indication | ||||
| Prior episodes of cholangitis/ choledocholithiasis | Bile duct caliber (mm) | Maximum stone diameter (mm) | Stone location | Others | |
| Patient 1 | 2/5 | 20 | 20a | Middle third of the choledochus | |
| Patient 2 | 1/1 | 35 | 35 | Retroduodenal choledochus | |
| Patient 3 | 1/1 | 20, with stricture in the distal third | 20 | Distal third of the choledochus and right hepatic duct | |
| Patient 4 | 1/3 | 20 | 25 | Left hepatic duct and confluence | |
| Patient 5 | 4/7 | 20 | 7a | Middle third of the choledochus | Intradiverticular major duodenal papilla |
| Patient 6 | 1/1 | 20 | 15a | Middle third of the choledochus | |
| Patient 7 | 1/1 | 25 | 22 | Distal third of the choledochus and confluence | Villous adenoma in the duodenal ampulla |
LCDA: Laparoscopic choledochoduodenal anastomosis; mm: millimeters
Antimicrobial administration was indicated in all the patients; it was therapeutic in 5 patients presenting with cholangitis and prophylactic in the remaining patients, given that the gastrointestinal tract is exposed in this surgery.
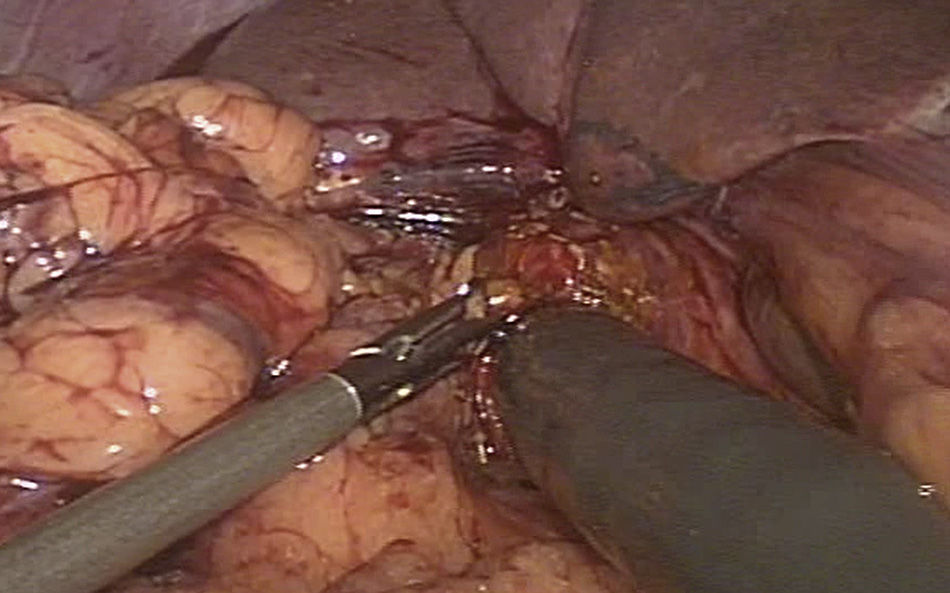
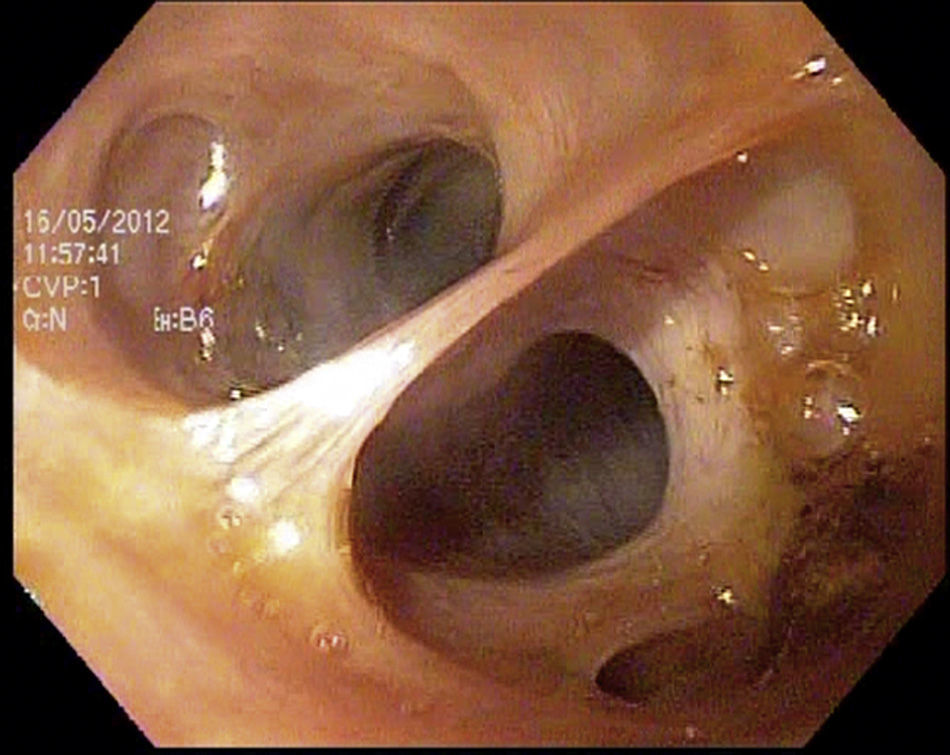
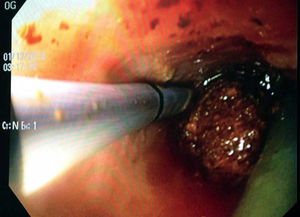
Joint intraoperative management was carried out. After a laparoscopic surgical approach, intraoperative choledochoscopy was performed through an anterior longitudinal choledochotomy using an Olympus GIF-H180 gastroscope with a 9.9mm diameter and a 2.8mm working channel (fig. 1), introduced by way of a 12mm laparoscopic working port.
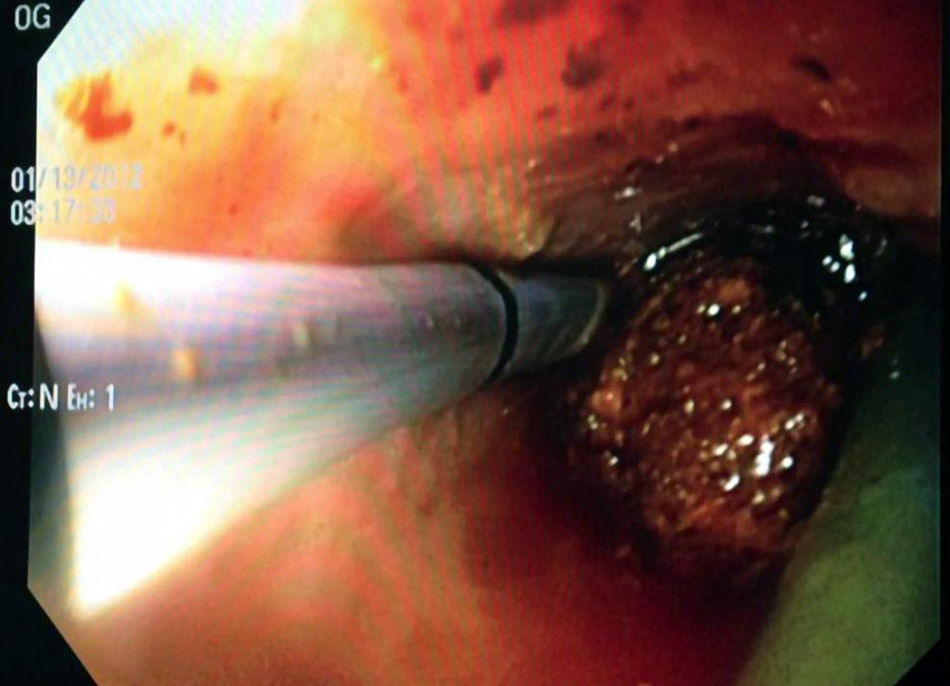
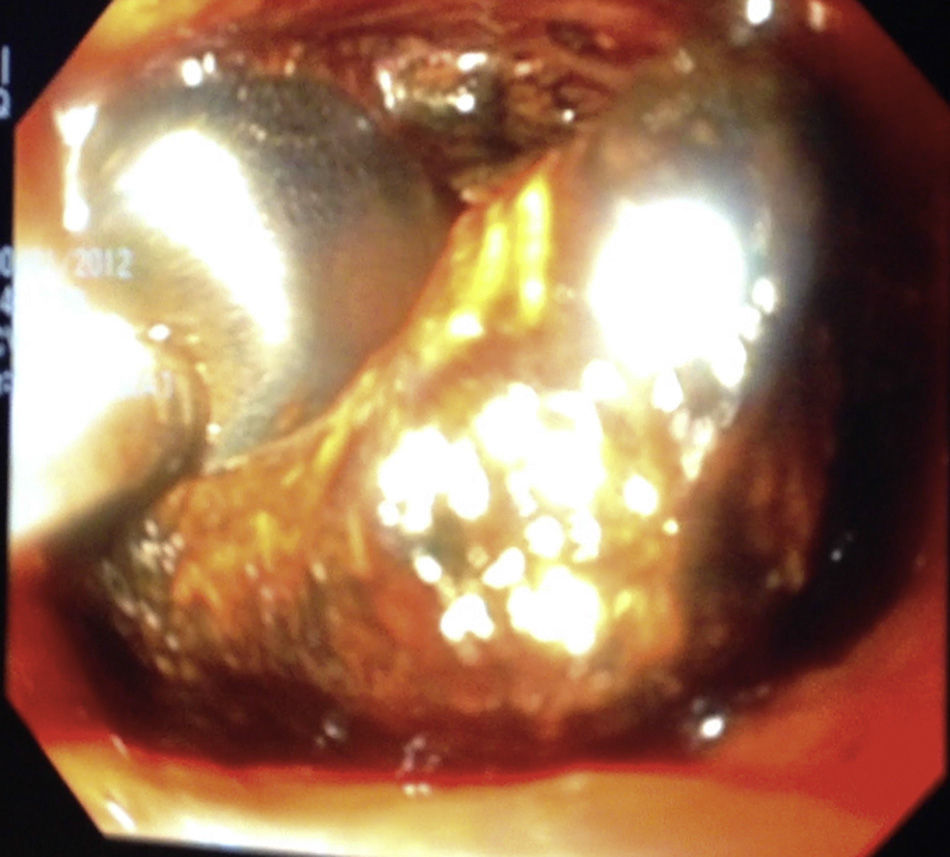
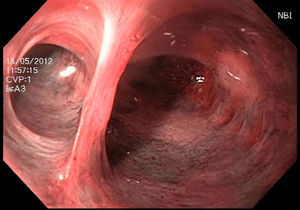
Choledochoscopy was performed both distal and proximal to the choledochotomy, with active stone extraction through the use of a Dormia basket and endoscopic balloon (figs. 2 and 3), until the absence of stones and the complete permeability of the proximal and distal biliary tract were confirmed (figs. 4 and 5).
Intraoperative choledochoscopy. The image shows a stone located in the confluence of the biliary tract, as well as the blue endoprosthesis that was palliatively placed during the ERCP. The laparoscopic grasper with which the stone was extracted can also be seen. ERCP: endoscopic retrograde cholangiopancreatography.
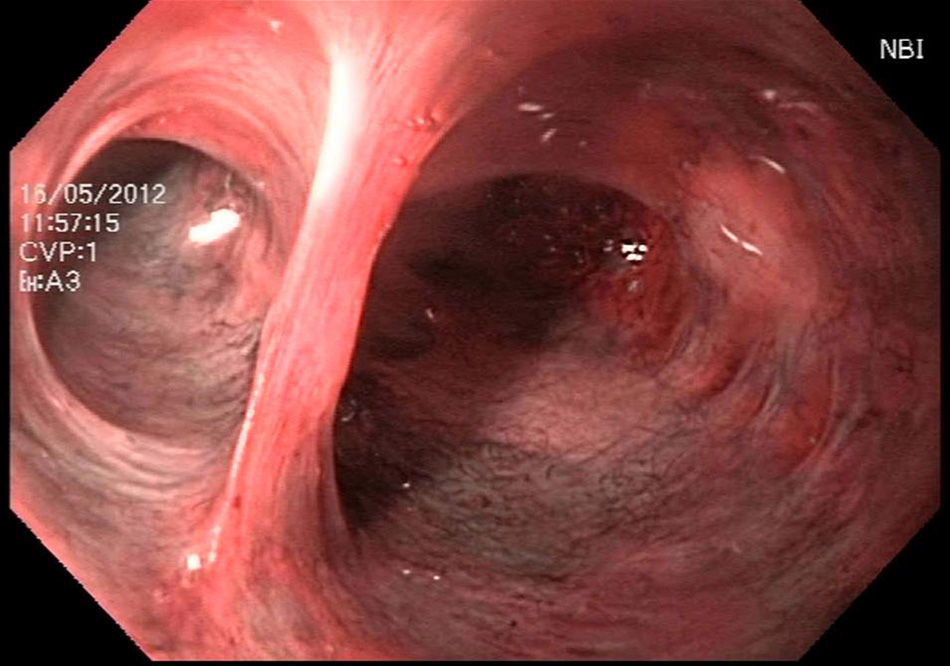
Once the surgical team finished the LCDA, peroral intraoperative choledochoscopy was performed through the recently formed anastomosis (fig. 6).
A descriptive statistical analysis of the variables was done through measures of central tendency and dispersion according to the data distribution, using the SPSS version 17 statistical package.
ResultsAll the patients (n=7) underwent peroral and transabdominal intraoperative choledochoscopy.
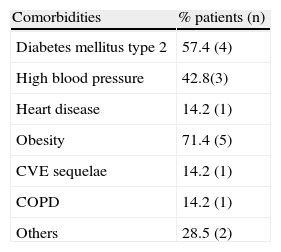
The mean age was 71 years (range 52-85 years), and there was a predominance of female patients (57.1%). In accordance with the Physical Status Classification established by the American Society of Anesthesiologists (ASA), one patient had an ASA II score, 5 had an ASA III score, and one had an ASA IV score. Patient comorbidities are described in Table 2.
Comorbidities of the patients that underwent the laparoendoscopic procedure.
| Comorbidities | % patients (n) |
| Diabetes mellitus type 2 | 57.4 (4) |
| High blood pressure | 42.8(3) |
| Heart disease | 14.2 (1) |
| Obesity | 71.4 (5) |
| CVE sequelae | 14.2 (1) |
| COPD | 14.2 (1) |
| Others | 28.5 (2) |
CVE: Cerebrovascular event; COPD: Chronic obstructive pulmonary disease.
During transabdominal choledochoscopy, active stone extraction was carried out through the use of a Dormia basket and endoscopic balloon in 4 patients, 3 of whom presented with intrahepatic lithiasis that was resolved with no complications. In the other 3 patients, the stones had been successfully removed during the preoperative ERCP. The absence of biliary tract stones was secured in 100% of the cases. The mean intraoperative endoscopy duration was 18minutes (range 4 to 45minutes).
In all the peroral intraoperative choledochoscopies both permeability and watertight closure of the choledochoduodenal anastomosis were secured.
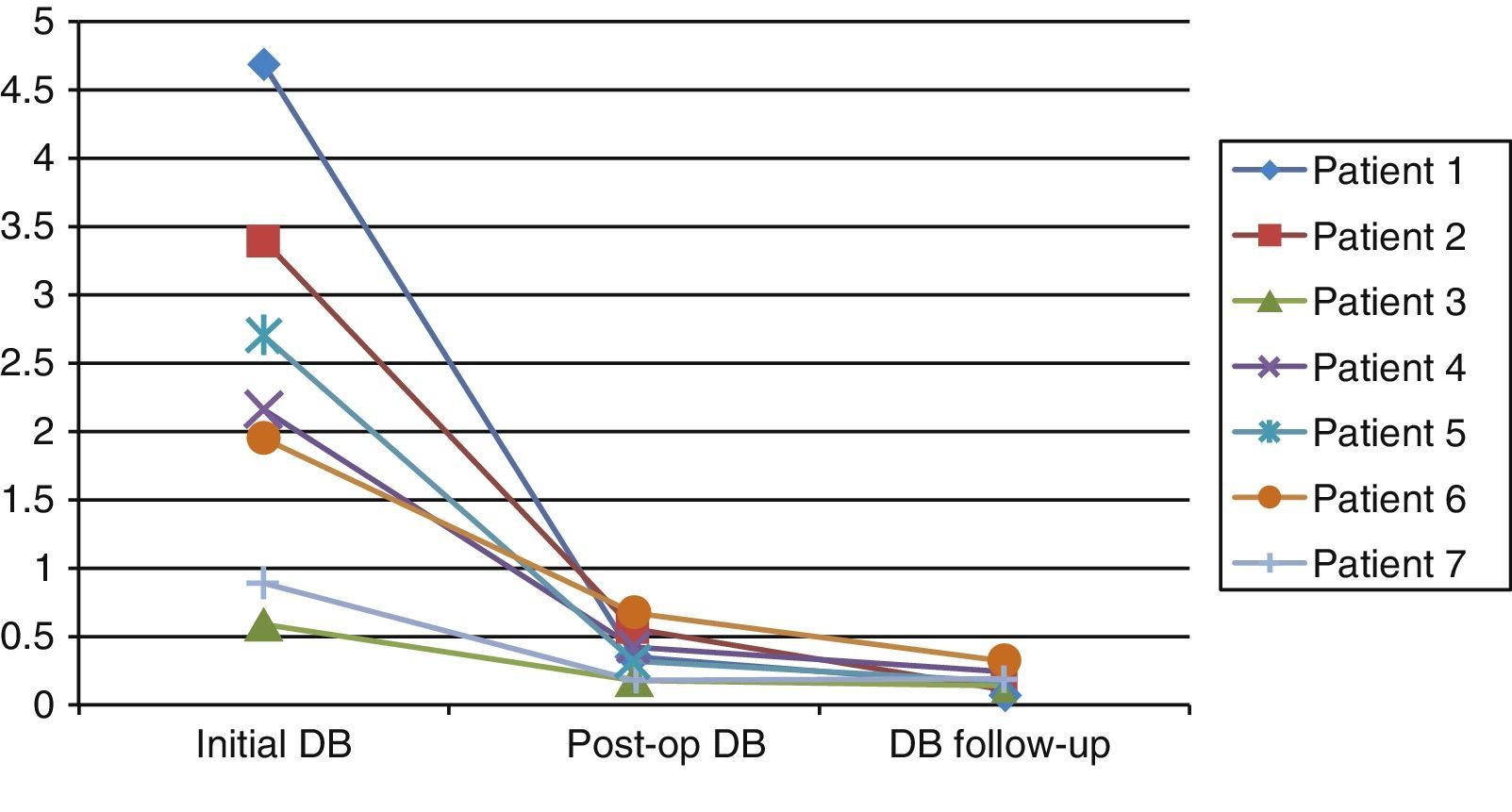
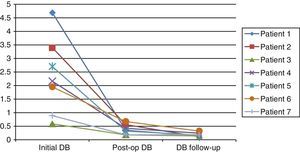
No complication attributable to the laparoendoscopic procedure developed and the biochemical parameters normalized progressively (fig. 7). The mean follow-up period duration was 155 days (range 28 to 420 days).
Descent progression of direct bilirubin in the patients; from their preoperative and immediate postoperative condition, as well as their outpatient follow-up status.
Initial DB: direct bilirubin prior to the endoscopic retrograde cholangiopancreatography, with stone extraction and endoprosthesis placement; Post-op DB: direct bilirubin after the laparoscopic choledochoduodenal anastomosis; DB follow-up: direct bilirubin in the outpatient follow-up.
Choledochoscopy has traditionally been a desired tool by surgeons during biliary tract exploration because it turns a «blind» procedure into one of direct vision and enables the retained stone rate to be reduced to zero, while increasing diagnostic capacity. 1,4,7,8,10,12–14Choledochoscopy has been proposed as routine procedure in all cholecystectomies, assuming that choledocholithiasis would be found in 5 to 10% of the patients.9,10 Performed through the cystic duct, it is feasible in 85 to 90% of the cases and its therapeutic and technical success rates are similar. Nevertheless, this approach is limited to stones that are under 10mm and located in the portion of the biliary tract that is distal to the cystic duct. 11,13,15 Even though some techniques have been described for those that are proximal to the duct, none have been standardized.16
Several therapeutic algorithms have been suggested for the management of choledocholithiasis: preoperative, intraoperative, and postoperative ERCP. The first option has a therapeutic success rate of approximately 95%. The second alternative is considered to cost less and involve a shorter hospital stay, but not all centers can provide it. Postoperative ERCP implies a longer hospital stay, as well as the obvious consequences in relation to resources if there are complications associated with the endoscopic procedure or if the procedure fails.10 A previously published work by a surgical team demonstrated the advantages of LCDA for managing difficult stones.17
In the present case series, intraoperative choledochoscopy was employed to carry out active stone extraction and to corroborate the adequate cleansing of the biliary tract in a situation in which a simple laparoscopic exploration of the biliary tract would have been insufficient due to the location, size, and characteristics of the stones. As has been reported, choledochoscopy is the most effective method for treating cases presenting with difficult stones. 7,14
Peroral choledochoscopy by way of the anastomosis allows for the adequate diameter of the diversion and its watertight closure to be corroborated, thus ensuring that there will be fewer complications such as leaks, fistulas, and early strictures as a consequence of the procedure.
No incident resulting from peroral choledochoscopy by way of an anastomosis was found in the literature review.
ConclusionsFrom our point of view, peroral and transabdominal intraoperative choledochoscopy are useful tools for the laparoscopic treatment of patients presenting with difficult-to-manage stones, given that they ensure adequate biliary tract clearance and enable the caliber and watertight closure of the anastomosis to be evaluated.
Multidisciplinary management is essential for offering decisive and definitive treatment for this complex pathology, with the benefit of a minimally invasive approach.
We recognize that the sample size of our study was a limitation, making it necessary to complement the information herein with future studies conducted on larger samples.
Financial disclosureNo financial support was received in relation to this article.
Conflict of interestThe authors declare that there is no conflict of interest.
Please cite this article as: Cuendis-Velázquez A, Rojano-Rodríguez ME, Morales-Chávez CE, González Angulo-Rocha A, Fernández-Castro E, Aguirre-Olmedo I, et al. Utilidad de la coledocoscopia transquirúrgica en el tratamiento de litos biliares difíciles. Revista de Gastroenterología de México. 2014;79:22–27.