Acute pancreatitis (AP) is a rare complication of pregnancy and its diagnosis ranges from 1/1,000 to 1/10,000 pregnancies. Hypertriglyceridemia is the third most frequent cause of gestational AP, after gallstones and alcohol, and occurs in approximately 4% of cases.1 It usually presents in women with pre-existing lipid metabolism anomalies.2
We present herein a case of hypertriglyceridemia-induced AP in a healthy pregnant woman with no past history of lipid anomalies. The pregnancy was the only known triggering factor for the hypertriglyceridemia.
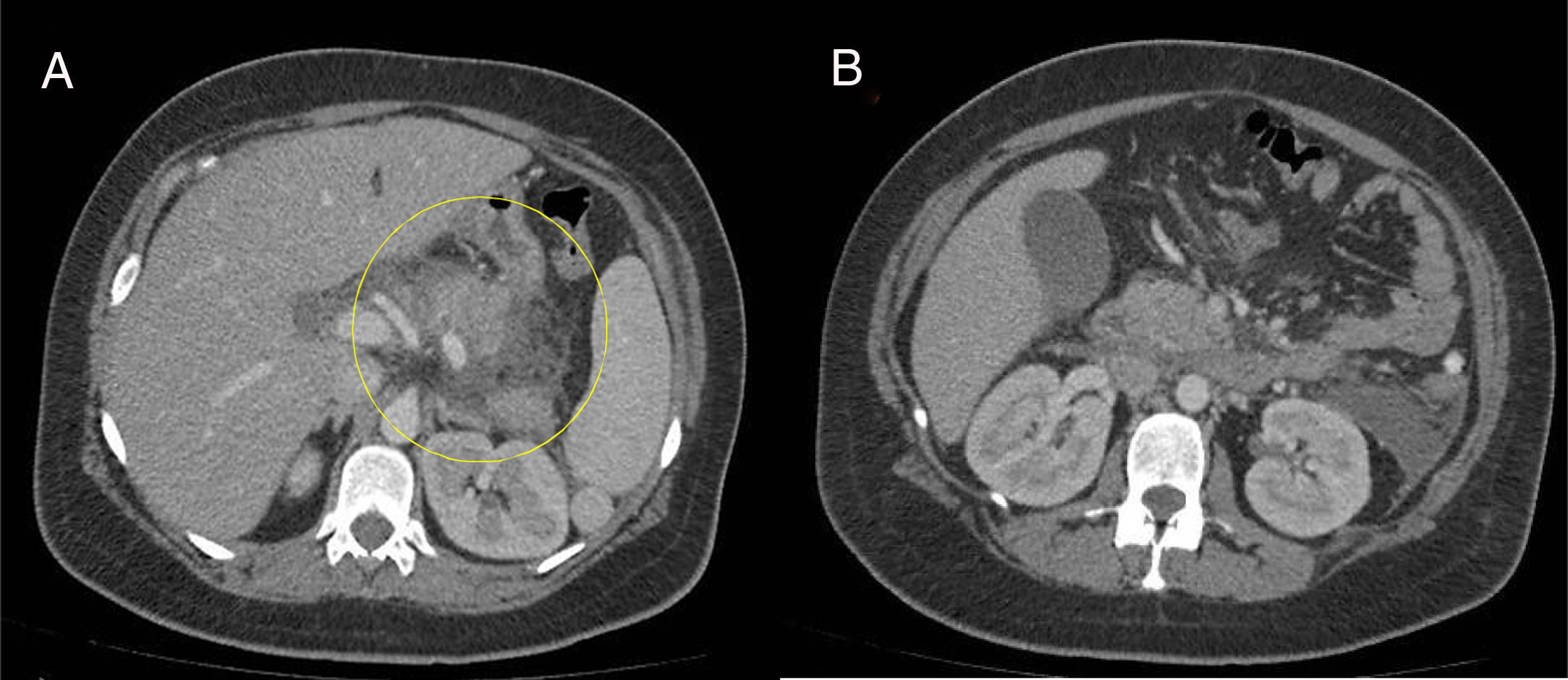
The patient had an unremarkable personal and family history. It was her first pregnancy and reached 39 + 4 weeks. She presented with glycosuria from the beginning of gestation, with a normal O'Sullivan test. The patient was admitted to our service due to photopsias, epigastralgia, vomiting, and elevated blood pressure (161/93mmHg), proteins in urine of 3 (+), and unassessable biochemistry due to “lipemic” serum. Given the possibility of severe preeclampsia because of her neurologic and gastrointestinal symptoms and blood pressure values,3 it was decided to bring the pregnancy to term. Urgent cesarean section was performed due to the suspicion of loss of fetal wellbeing. Upon opening the parietal peritoneum, abundant chelated ascites was observed, and the rest of the cavity was normal (no pathology was found in the cecal appendix, sigmoid colon, gallbladder, or gastric antrum or pylorus). In the immediate postoperative period and 24h after symptom onset, laboratory tests were performed that reported lipase of 1,117 U/l (62-230), triglycerides of 5,860mg/dl (50-165), cholesterol of 810mg/dl (150-200), and glucose of 510mg/dl (65-100). Abdominal ultrasound identified a slight increase in the size of the pancreas with indistinct edges and reduced echogenicity. An abdominal tomography scan (fig. 1) revealed a mildly edematous pancreas with no necrosis, surrounded by a non-encapsulated, homogeneous, peripheral fluid collection. The gallbladder was normal in size with no signs of stones.
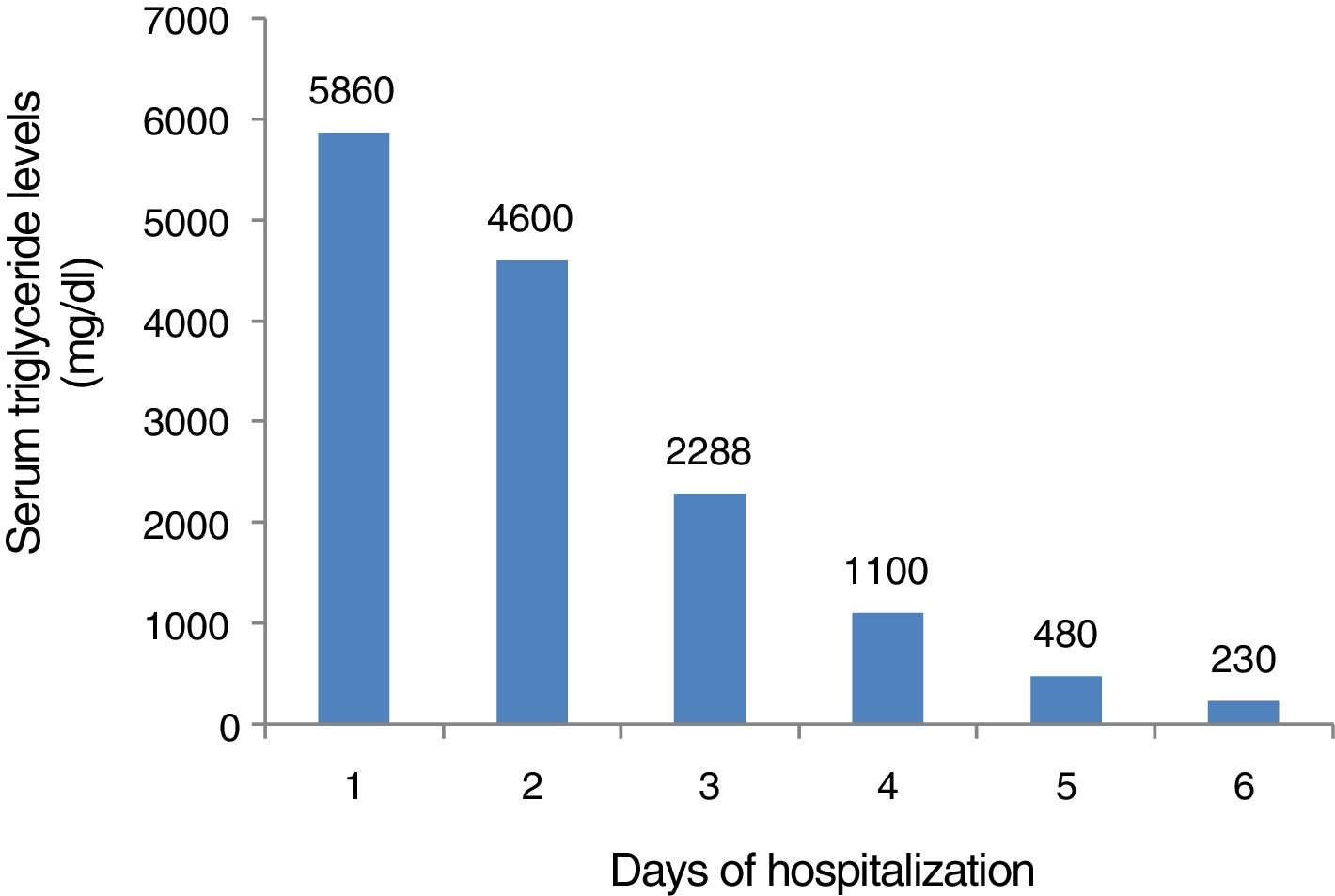
With the diagnosis of edematous AP due to hypertriglyceridemia, treatment was begun with intravenous hydration, insulin therapy, and low-molecular-weight heparin infusion. The patient was evaluated by the endocrine service with the recommendation of fibrate therapy initiation (fenofibrate, 145mg at night), long-term dietary restriction of fats, and introduction of middle chain triglycerides and omega-3 fatty acids. The patient presented with normalization of her blood pressure and improved laboratory test results, with a gradual decrease in triglyceride level (fig. 2), and so was released from the hospital on postoperative day six. Normal values of the APO E genotype and apolipoprotein A1, B, CII, and E were confirmed. One year after the gastrointestinal episode, the patient was asymptomatic, with an almost normal triglyceride level (193mg/dl), and under treatment with a diet of 1,800kcal.
Pregnancy is associated with a mild increase in triglycerides and cholesterol, caused by elevated levels of estrogens, progestogens, and placental lactogen that lead to reduced LPL gene activity and VLDL-C clearance.4 Despite those alterations in the lipid profile, triglyceride levels rarely exceed 300mg/dl in the third trimester. Triglyceride levels above 1,000mg/dl suppose a risk for the development of pancreatitis and other complications, such as preeclampsia, gestational diabetes, and preterm birth.5,6 The significant increase in triglyceride levels produces an oxidative environment with endothelial damage,5 which can favor preeclampsia. Some authors have related maternal hyperlipidemia during pregnancy with the increase of precursory atherosclerotic lesions in the fetus.5 All of the above leads to increased morbidity and mortality for both the mother and the fetus.
Whether the hypertriglyceridemia in AP should be treated is a matter of discussion. Within the first 24-48h of symptom onset, triglyceride levels drop as a consequence of fasting. Plasmapheresis can be used in patients with triglyceride levels above 1,000mg/dl, whose lipase levels are 3 times above normal, and that have signs of hypocalcemia, lactic acidosis, or organ dysfunction. A systematic review on its usefulness reported reduced triglyceride levels of up to 84% in a single plasmapheresis session.7 If plasmapheresis is not available or plasma glucose levels are above 500mg/dl, intravenous regular insulin perfusion can be started. Some studies report the use of heparin, alone or with insulin, but its indication is not clear.8 Insulin and heparin infusions stimulate lipase lipoprotein activity that then eliminates triglycerides from the plasma.9
In our patient, neither pancreatic enzymes nor triglycerides were determined in the emergency service and diagnosis was made after the cesarean section. Despite the presentation of AP complicated by acute fluid collections, both the mother and the neonate progressed favorably with conservative treatment. Pregnant women are a risk group for the development of hyperglyceridemia-induced AP, given that pregnancy, itself, favors the increase in triglyceride levels, which is sometimes extreme. There must be high diagnostic suspicion, because in patients such as ours, there was no pre-gestational lipid alteration. The appearance of that type of AP is rare. Through early diagnosis and adequate management, the maternal mortality rate has currently decreased to 1% and the perinatal mortality rate to 18%.10
Financial disclosureNo financial support was received in relation to this article.
Conflict of interestThe authors declare that there is no conflict of interest.
Please cite this article as: Pérez-Martínez N, Mancebo-Mata A, García-Martín R, Varela-Trastoy P. Pancreatitis aguda por hipertrigliceridemia, causa inusual de dolor abdominal en el embarazo. Revista de Gastroenterología de México. 2019;84:517–518.