Gastroparesis is a syndrome characterized by a delay in gastric emptying, in the absence of mechanical obstruction. Its main symptoms are: nausea, vomiting, and early satiety.1 Idiopathic etiology is the most frequent, but postoperative and metabolic (diabetes mellitus) etiologies have also been regularly documented.2 The criterion standard for diagnosis is gastric emptying scintigraphy, in which a standardized diet radiomarked with 99m TC colloidal sulfur is ingested, obtaining images at 0, 60, 120, 180, and 240min. Emptying delay is defined as > 10% gastric retention in 4h.3 Treatment consists of controlling symptoms and improving emptying.4 The response rate of dietary and drug modifications, including metabolic control in diabetic patients, is low (< 20%).5 Intrapyloric botulinum toxin injection, a current treatment, has a temporary and poor response rate (15-20%).6 Surgical management includes electric stimulation, pyloroplasty, and total or subtotal gastrectomy, with regular results (40-60%) and high morbidity and mortality.1,2 Per oral endoscopic myotomy (POEM) is a technique that was developed for the treatment of achalasia, and has shown good safety and efficacy.7 The idea of performing an endoscopic pyloromyotomy (G-POEM) was recently developed, utilizing the basic components of POEM to improve gastric emptying through gravity, despite the presence of gastroparesis. Initial results on different populations, including a multicenter study, have shown good safety and efficacy in humans (> 80% initial response).8–10
Gastroparesis is a frequent pathology in the Mexican population. The aim of this report was to describe the case of a Mexican patient with refractory gastroparesis treated with the G-POEM procedure.
A 25-year-old woman had a past medical history of well-controlled hypothyroidism and chronic constipation that did not respond to medical treatment. She required a subtotal colectomy due to colonic inertia, and in a second surgical stage, she underwent bowel transit restitution that was performed 10 years ago. Her current illness began 4 years prior to her hospital admission, with nausea, vomiting, early satiety, and a 15-kg weight loss. The evaluation protocol began with endoscopic study that ruled out mechanical obstruction. A gastric emptying scan showed 46% retention at 4h, resulting in the diagnosis of idiopathic gastroparesis. Medical and dietary treatment was begun, providing partial symptom improvement, and thus the gastroparesis was considered treatment-refractory. The G-POEM procedure was planned, once the patient gave her informed consent and authorization from the hospital ethics committee was obtained. The patient's quality of life and the magnitude of her symptoms were evaluated prior to the G-POEM through the Gastroparesis Cardinal Symptom Index (GCSI) questionnaire,11 with a score of 37/45.
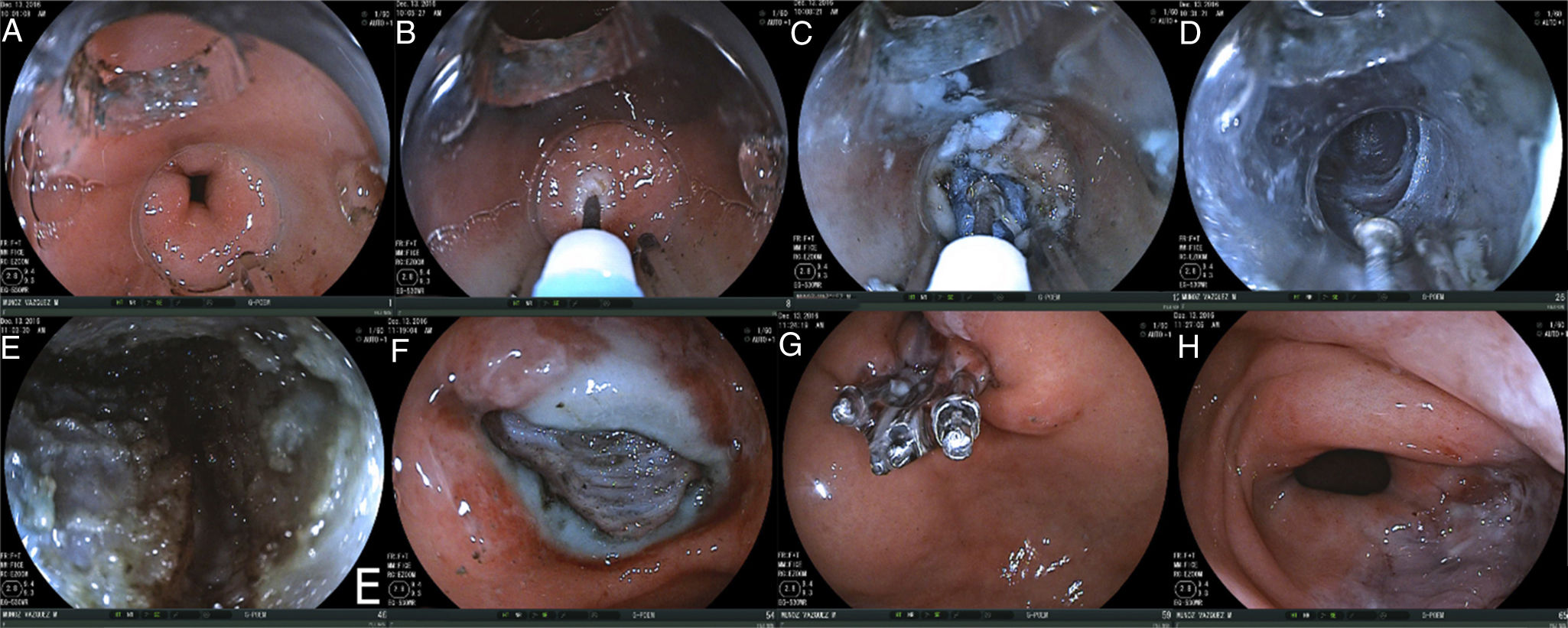
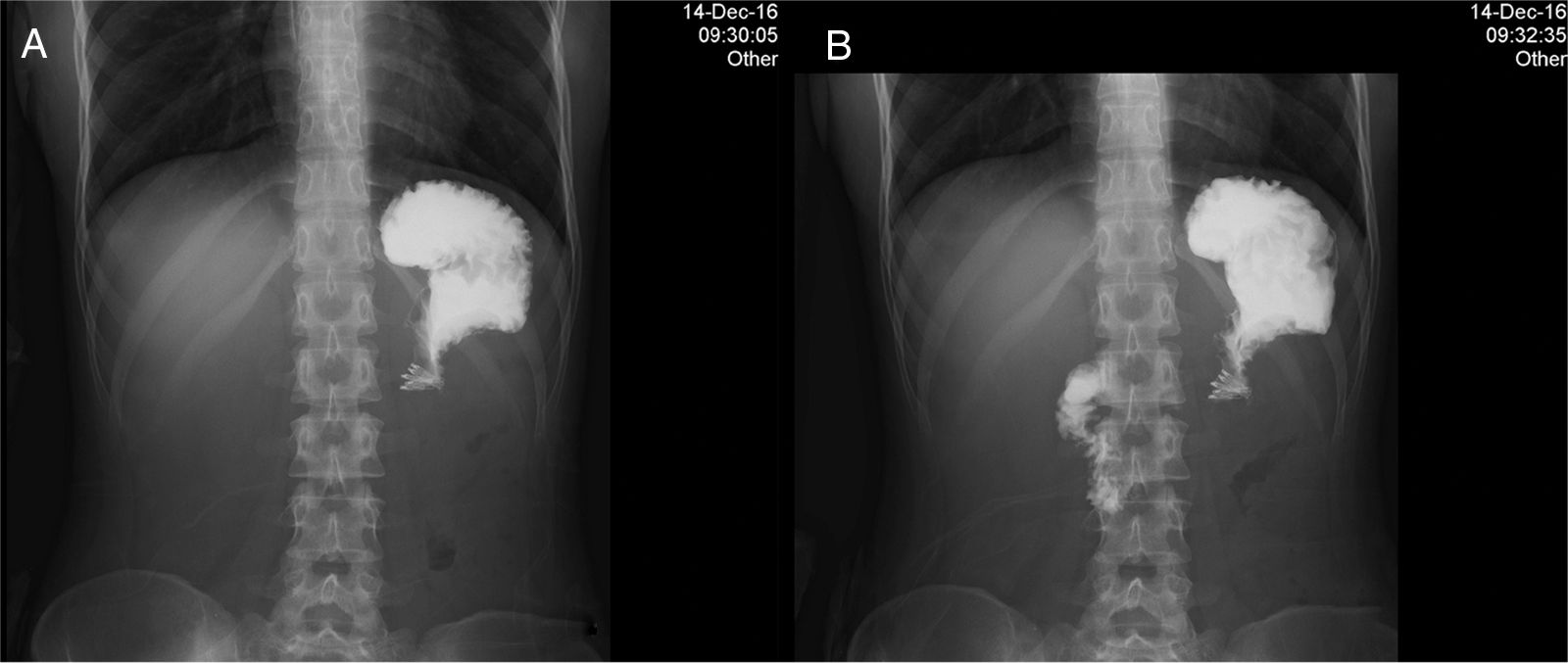
The patient fasted 24h before the procedure and was given 1g IV of cefotaxime as prophylaxis. A conventional model EG590WR endoscope (Fujinon, Saitama, Japan) was employed, along with a DH-28GR hood (Fujinon, Saitama, Japan), and an ERBE VIO-200D electrosurgical unit with a hybrid knife (Tübingen, Germany). The parameters were: injection (ERBEJET, effect 50), incision (ENDOCUT Q, effect 3, cutting duration 3, cutting interval 3), tunnelization (SWIFT COAG, effect 3 at 70W), myotomy (ENDOCUT Q), and hemostasis (SOFT COAG, effect 3 at 40W). Hemoclips (Boston Scientific, USA) and a CO2 insufflator (ENDOSTRATUS, Medivators, Minneapolis, MN, USA) were also used. The G-POEM technique consisted of the following steps: 1) revision and injection: the antrum was viewed and a combination of 0.9% sodium chloride solution with 0.5% methylene blue was injected 5cm before the pylorus, above the lesser curvature; 2) incision: a 20-mm longitudinal incision was made; 3) tunnelization: a submucosal tunnel was created from that point until passing the pylorus and reaching the proximal region of the duodenum; 4) myotomy: total thickness myotomy of the pyloric muscle was performed 2cm proximal to it; 5) closure: 5 hemoclips were placed (fig. 1). Procedure duration was 60min and there were no complications. Bowel transit with water-soluble contrast material at 24h ruled out leakage into the submucosal tunnel, and adequate passage of the contrast medium into the duodenum was observed less than 2min from its administration, indicating treatment success (fig. 2). Oral fluid intake was begun and the patient was sent home 48h after the procedure with no complications. At the check-up one week later, symptoms had improved 33% (GSCI score of 23/45). Control gastric emptying scan showed an 8% emptying delay at 240min.
Steps of the G-POEM procedure. A) Initial viewing of the pylorus prior to the procedure. B) Injection. C) Longitudinal incision. D) Creation of the submucosal tunnel. E) Myotomy of the pyloric muscle. F) Incision at the end of the procedure. G) incision closure with hemoclips. H) The pylorus is clearly observed to be more open after the procedure.
In conclusion, G-POEM is a technically feasible procedure at centers with experience in endoscopic dissection and is a new alternative in the treatment of patients that have refractory gastroparesis or are at high risk for surgical morbidity and mortality. The procedure offers good initial results in terms of safety and efficacy, as shown in the present case, but intermediate and long-term prospective studies with a greater number of patients are needed to determine the true role of this procedure in the treatment of gastroparesis.
Conflict of InterestThe authors declare that there is no conflict of interest.
Please cite this article as: Hernández-Mondragón OV, Solórzano-Pineda OM, Blancas-Valencia JM, González-Martínez MA, Villanueva-Pérez RM. Piloromiotomía endoscópica por vía oral para el tratamiento de gastroparesia refractaria: reporte del primer caso en México. Revista de Gastroenterología de México. 2018;83:459–461.