In the Western world, gastric cancer is diagnosed at late stages of the disease. Radical surgery conditions survival,1 but complete resection (R0) is not always possible. When the tumor extends beyond the stomach and affects the neighboring organs, the pancreas is involved in up to 50% of the cases,2 and the justification for radical surgery is not clear in terms of survival. The addition of pancreaticoduodenectomy to the gastrectomy is not a customary procedure, nor is it accepted as the gold standard for the surgical treatment of advanced gastric cancer. However, there are exceptions that do justify its application, as in the case we present below.
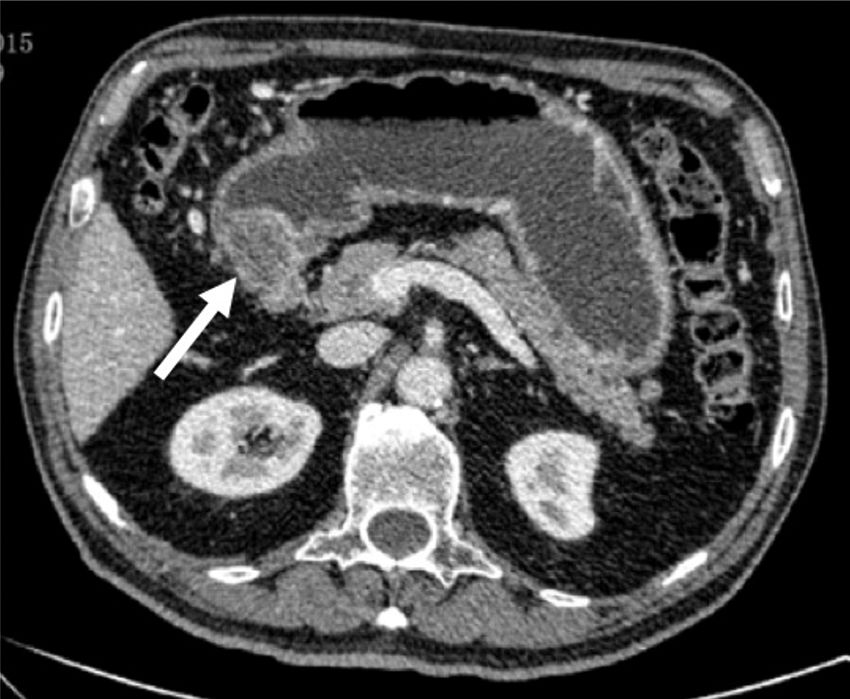
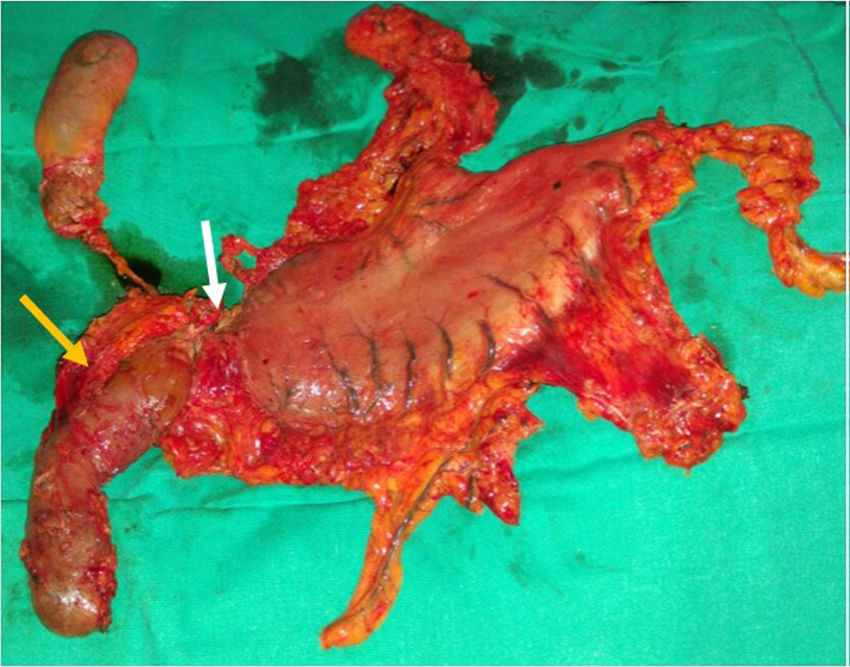
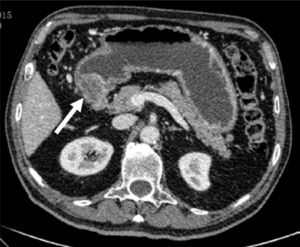
A 76-year-old man presented with epigastric pain and constitutional syndrome of 3-month progression. Upper gastrointestinal endoscopy was carried out that identified a large antropyloric ulcer that did not allow the passage of the endoscope. Biopsy showed infiltrating adenocarcinoma. The extension study reported an antropyloric stricturing neoplasia, with perigastric adenopathies and stage II-B (T3N1M0) disease in the hepatogastric ligament (fig. 1). The patient underwent neoadjuvant chemoradiotherapy with 9 cycles of paclitaxel-carboplatin and 45Gy over a 2-month period. Restaging chest and abdominal CT revealed partial response and salvage surgery was decided upon. Exploratory laparoscopy identified a stony tumor in the pylorus, with adenopathies of suspected malignancy in the hepatoduodenal ligament. There was apparent infiltration of the entire thickness of the gastric wall and the tumor extended into the duodenum, passing the gastroduodenal artery and reaching the papilla. Whether it was a tumor or residual fibrosis from the chemotherapy could not be determined. Diagnosis was negative for malignant cells after peritoneal wash-out, resulting in conversion to open surgery and the performance of total gastrectomy, cephalic pancreaticoduodenectomy, lymphadenectomy, and the classic Whipple reconstruction. Intraoperative biopsy confirmed disease-free surgical margins (fig. 2). The histologic study of the surgical specimen revealed grade G1, 3.5 x 3-mm residual tubular adenocarcinoma with a marked response to the neoadjuvant treatment and 12 lymph nodes with no signs of malignancy (ypT1b ypN0).
After 3 years of follow-up, the patient is currently asymptomatic with no signs of disease recurrence.
Gastric cancer is one of the main causes of death by cancer worldwide. Its outcome is poor, due to late diagnosis. The pancreas is the organ that is the most frequently affected and is considered an independent factor for poor prognosis.3 Complete oncologic resection of the disease is vital for optimum results, but radical surgery that involves the duodenum and pancreas results in elevated morbidity and mortality and has traditionally been thought not to improve survival and therefore was not indicated.4 More recent studies show that surgical advances have reduced morbidity and mortality and achieved increases in disease-free survival rates.5–7 Our case is an example of the indication for and safety of the procedure, obtaining clear benefits with respect to survival and quality of life.
Adequate evaluation of tumor extension, the basal situation of the patient, and the technical possibility of surgically removing the apparently affected zone are indispensable elements for the success of said aggressive management. In their review of pancreatic involvement in gastric cancer, Roberts et al.8 pointed out that intraoperative overdiagnosis took place in one-third of the patients with locally advanced gastric cancer, conditioning over-treatment and considerable morbidity and mortality, but they also stated that microscopic involvement could go undetected. Hence, the importance of neoadjuvant treatment for optimizing results.2 Ozer et al.9 proposed the performance of echoendoscopy in all patients with locally advanced gastric cancer, to increase diagnostic accuracy. Even so, they attributed the final resection decision to surgical findings. With the use of echoendoscopy in the present case, it was not possible to pass through the stricture, nor could the distinction be made between tumor or fibrosis from or a desmoplastic reaction to the chemoradiotherapy, thus the definitive therapeutic decision was made intraoperatively. The initial staging accuracy of gastric cancer aids in making the correct therapeutic decision. It also enables better selection of the patients that can benefit from surgery that extends beyond the customary limits of standard oncologic gastrectomy and it can also prevent unnecessary high-morbidity surgeries.
The performance of a cephalic pancreaticoduodenectomy associated with oncologic gastrectomy due to advanced gastric adenocarcinoma is a safe and feasible option in exceptional cases. However, it should not be routinely recommended, given the morbidity of pancreaticoduodenectomy and the poor survival rate in patients with gastric cancer invading the second portion of the duodenum. In the context of multidisciplinary management, the excellent response to neoadjuvant oncologic treatment and an adequately trained surgical team for performing the procedure with minimum morbidity, can offer survival benefits and be the keys to the success of that strategy in selected patients.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of dataThe authors declare that they have followed the protocols of their work center on the publication of patient data.
Right to privacy and informed consentThe authors declare that no patient data appear in this article.
Financial disclosureNo financial support was received in relation to this article.
Conflict of interestThe authors declare that there is no conflict of interest.
Please cite this article as: Acosta-Mérida MA, Ortiz-López D, Callejón-Cara MM, Rahy-Martín A, Marchena-Gómez J. Adenocarcinoma gástrico: ¿debemos asociar pancreaticoduodenectomía ante sospecha intraoperatoria de infiltración? Revista de Gastroenterología de México. 2019;84:405–407.