Endoscopic retrograde cholangiopancreatography (ERCP) is the treatment of choice for symptomatic choledocholithiasis during pregnancy. In pregnant patients, aside from the risks inherent in the procedure and sedation, there is the added concern of the potentially damaging effects of ionizing radiation on the fetus.
AimTo describe the maternal and fetal results of ERCP performed to resolve symptomatic choledocholithiasis in pregnant patients.
Materials and methodsA retrospective, descriptive, observational, and cross-sectional study was conducted. It included pregnant patients with choledocholithiasis that underwent ERCP within the time frame of June 2017 and June 2018.
ResultsThe study included 9 pregnant patients, with a mean gestational age of 24.1 weeks, that underwent ERCP. There were no maternal or fetal complications associated with sedation, mean fluoroscopy time was 26.7s, and one patient (11.1%) presented with mild post-ERCP pancreatitis that was resolved through medical management. Pregnancy progression was normal in 100% of the cases, resulting in the birth of neonates with a normal Apgar score, a mean weight of 3120g, a mean length of 49.94cm, and a mean gestational age of 38.37 weeks. At follow-up at 6 months, the infants had a mean weight of 7.1kg and a mean length of 66.94cm.
ConclusionsThe results from our hospital center were similar to those described in the international literature, showing that ERCP in our medical environment is a feasible, safe, and efficacious method for both the mother and fetus. When performed by an experienced endoscopist, it should be considered the treatment of choice for choledocholithiasis in pregnant patients.
La colangiopancreatografía retrógrada endoscópica (CPRE) es el tratamiento de elección para la coledocolitiasis sintomática durante el embarazo. Además de los riesgos inherentes al procedimiento y a la sedación, en pacientes embarazadas se agrega la preocupación por los potenciales efectos dañinos que la radiación ionizante pudiera tener sobre el feto.
ObjetivoDescribir los resultados maternos y fetales obtenidos con la CPRE para la resolución de la coledocolitiasis sintomática en pacientes embarazadas.
Material y métodosEstudio observacional, descriptivo, retrospectivo y transversal. Se incluyó a pacientes embarazadas con coledocolitiasis tratadas con CPRE durante el periodo comprendido de junio de 2017 a junio de 2018.
ResultadosSe incluyó a 9 pacientes embarazadas tratadas mediante CPRE con una media de edad gestacional de 24.1 semanas. No se presentaron complicaciones maternas ni fetales asociadas a la sedación; la media de tiempo de fluoroscopia fue de 26.7 segundos, una paciente (11.1%) presentó pancreatitis post-CPRE leve que se resolvió con manejo médico. En el 100% de los casos el embarazo fue normoevolutivo y culminó con el nacimiento de un producto con Apgar normal, con una media de peso de 3,120g, una media de talla de 49.94cm y una media de 38.37 semanas de gestación. El seguimiento a 6 meses de los niños demostró una media de peso de 7.1kg y una media de talla de 66.94cm.
ConclusionesLos resultados obtenidos en el hospital sede son similares a los descritos en la literatura mundial y demuestran que en nuestro medio la CPRE es un método factible, eficaz y seguro tanto para la madre como para el feto, por lo que, en manos expertas, debe considerarse el tratamiento de elección para la coledocolitiasis en pacientes embarazadas.
Hormonal changes due to pregnancy (increased estrogens and progesterone) increase the saturation of cholesterol in bile and reduce the contractility of the gallbladder, resulting in an increased risk for the formation of bile duct stones.1 The reported prevalence of gallstone disease during pregnancy varies from 3.3% to 12%. In fact, acute cholecystitis is the second most common non-obstetric emergency in pregnant patients.2
The complications derived from gallstones, such as pancreatitis and choledocholithiasis, are less frequent. The estimated incidence of stones in the common bile duct in pregnant women is 1/1000.3 Between 58% and 72% of pregnant patients with choledocholithiasis that are managed only with analgesics (conservative treatment) have a new episode of pain and require rehospitalization during the same pregnancy. Therefore, the current recommendation is to remove the bile duct stones upon diagnosis.3,4
Endoscopic retrograde cholangiopancreatography (ERCP) is less invasive and has a lower morbidity rate than surgical exploration of the biliary tract, and thus is considered the treatment of choice for symptomatic choledocholithiasis during pregnancy. The ERCP rate in pregnant women is calculated at 1 in every 1415 pregnancies.4
The main maternal complications that can present after an ERCP are bleeding (0.3–2%), cholangitis (0.5–3%), acute cholecystitis (0.5%), and duodenal perforation (0.08–0.6%). Different studies have shown that those complications present with the same frequency in pregnant and nonpregnant women that undergo ERCP. A 2016 retrospective study by Inamdar et al. included 907 pregnant patients and 2721 nonpregnant women, with similar demographic characteristics, that underwent ERCP due to choledocholithiasis. Pregnancy was identified as an independent risk factor for the development of post-ERCP pancreatitis (12% vs. 5%; RR 2.8, CI: 2.1–3.8; p<0.001). Those authors emphasized the fact that despite the increased risk for pancreatitis, ERCP should not be postponed in patients with a clear indication for the procedure.5
One of the main concerns of performing ERCP in pregnant patients is the harmful effect that ionizing radiation could have on the mother and fetus.4,6
The possible teratogenic effects of ionizing radiation are divided into: deterministic effects and stochastic effects. Deterministic effects, such as growth retardation, mental retardation, and fetal malformations, are those that can present when surpassing a certain threshold dose and stochastic effects, such as genetic anomalies, are those that theoretically could present at any dose.1,4
The threshold dose for the presence of deterministic effects on the human fetus is 50mGy, according to the American College of Obstetricians and Gynecologists and between 100 and 200mGy, according to the International Radiation Protection Association. Said doses are much higher than those that are usually reached during the average ERCP performed by an experienced endoscopist (0.1–3mGy).1
Different strategies are directed at reducing the dose of radiation that both the mother and fetus are exposed to, resulting in what is known as reduced-radiation ERCP. Those methods consist of placing a lead apron over the maternal pelvis, utilizing the fluoroscope for the least possible amount of time, keeping the image intensifier as close as possible to the patient, utilizing the magnification mode only when indispensable, employing modern fluoroscopic equipment, and collimating the X-ray beam to the area of interest.7
Our aim was to describe both the maternal and fetal results of ERCP performed for the treatment of symptomatic choledocholithiasis in pregnant patients at a secondary care hospital in Mexico City, within the time frame of June 2017 and June 2018.
Materials and methodsA retrospective, descriptive, observational, and cross-sectional study was conducted that included all pregnant patients with symptomatic choledocholithiasis that underwent ERCP at the Hospital General Dr. Manuel Gea González, within the time frame of June 2017 and June 2018.
ERCP was performed only in pregnant patients at high risk for choledocholithiasis, according to the American Society for Gastrointestinal Endoscopy (ASGE) criteria. Patients at intermediate risk underwent magnetic resonance cholangiography (MRC) and cases with confirmed choledocholithiasis underwent ERCP.
The patients were treated in conjunction with the Gynecology and Obstetrics Service. Maternal blood pressure, oxygen saturation, and electrocardiographic tracing were monitored during the procedure. Fetal heart rate was reviewed by the gynecologists before and immediately after the procedure. Transrectal indomethacin was administered to all the patients as prophylaxis for pancreatitis.
All the procedures were performed by an experienced endoscopist, applying the reduced-radiation ERCP techniques. After an 8-h fast, the patients were placed in the left lateral decubitus position to prevent compression of the vena cava. A 0.5mm lead apron was placed over the pelvis of all the patients to protect the fetus. Sedation was carried out by an experienced anesthesiologist, utilizing meperidine or propofol. The common bile duct was selectively cannulated with a guided sphincterotome and opacified with non-ionic water-soluble contrast medium diluted at 50%, along with therapeutic instrumentation, as required in each case. All patients underwent control fluoroscopy, collimating the X-ray beam to the area of interest, and radiographs were intentionally not taken to reduce the dose of radiation the mother and fetus were exposed to.
The demographic data and laboratory test results (complete blood count, blood chemistry, liver function tests, and coagulation times) were recorded, as were the liver and bile duct ultrasound studies, fluoroscopy times, technical details and complications of the ERCP, type of delivery (vaginal or C-section), weeks of gestation at birth, the presence of neonate malformations and mortality, Apgar score at 1min and at 5min of life, and weight and length at birth and at 6 months.
All the patients remained under in-hospital surveillance after ERCP, to detect possible complications associated with the procedure. Post-ERCP pancreatitis was defined as the presence of epigastric pain radiating to the back, during the 48h after the procedure, accompanied by amylase and lipase levels at least 3-times higher than normal values.
Statistical analysisThe data were recorded on a data collection sheet specifically designed for the line of research carried out and then placed in a database (Microsoft Excel, Microsoft Corporation, Seattle, WA, USA). The statistical analysis was carried out using the SPSS 21 program (IBM Corporation, Armonk, NY, USA). Mean and standard deviation (SD) were used as measures of central tendency and dispersion, respectively, for the quantitative variables with normal distribution. Median and interquartile range were employed for the distribution-free quantitative variables. Nominal qualitative variables were expressed as frequency measures.
Ethical considerationsAll the pregnant patients that underwent ERCP were informed of the risks and possible complications associated with the procedure and signed written statements of informed consent, accepting its performance. No statements of informed consent were requested for the publication of the present study, because as a descriptive, observational study, no intervention was carried out, the clinical course of the patients was not altered, and no personal data that could identify the patients were published.
ResultsNine ERCPs were performed on pregnant patients within the time frame of June 2017 to June 2018. Mean maternal age was 28.89 years (SD 3.86), mean gestational age was 24.1 WG (5 patients were in the second trimester and 4 in the third), with a SD of 8.89. Mean diameter of the extrahepatic bile duct prior to the procedure was 7.87mm (measured through transabdominal ultrasound), with a SD of 3.96.
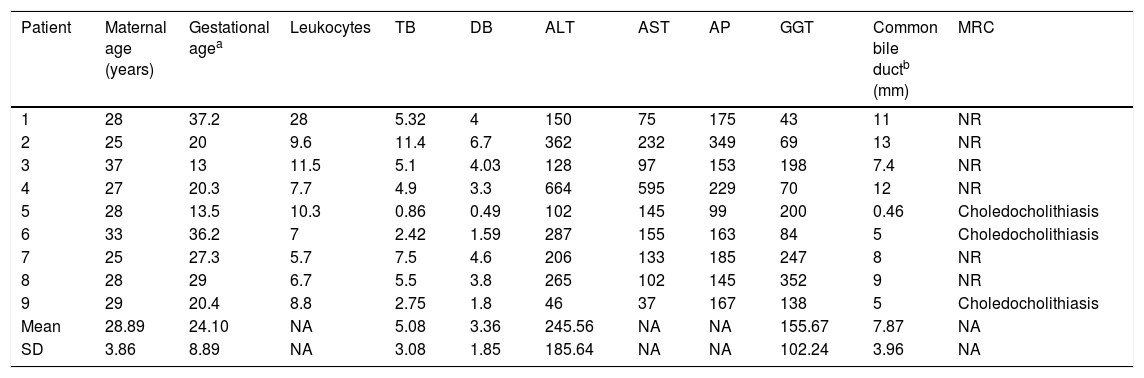
Imaging and laboratory data were grouped according to the ASGE criteria for establishing the risk for presenting with choledocholithiasis, resulting in 6 patients (66.7%) with high risk and 3 patients (33.3%) with intermediate risk. The patients at intermediate risk underwent MRC, which demonstrated the presence of stones inside the common bile duct. Table 1 shows the mean and SD of the imaging and laboratory data with normal distribution. The distribution-free variables were leukocytes, AST, and AP, with a median of 8.8, 133, and 167, respectively, and an interquartile range of 4.1, 108, and 58, respectively.
Demographic and paraclinical characteristics of the patients.
| Patient | Maternal age (years) | Gestational agea | Leukocytes | TB | DB | ALT | AST | AP | GGT | Common bile ductb (mm) | MRC |
|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 28 | 37.2 | 28 | 5.32 | 4 | 150 | 75 | 175 | 43 | 11 | NR |
| 2 | 25 | 20 | 9.6 | 11.4 | 6.7 | 362 | 232 | 349 | 69 | 13 | NR |
| 3 | 37 | 13 | 11.5 | 5.1 | 4.03 | 128 | 97 | 153 | 198 | 7.4 | NR |
| 4 | 27 | 20.3 | 7.7 | 4.9 | 3.3 | 664 | 595 | 229 | 70 | 12 | NR |
| 5 | 28 | 13.5 | 10.3 | 0.86 | 0.49 | 102 | 145 | 99 | 200 | 0.46 | Choledocholithiasis |
| 6 | 33 | 36.2 | 7 | 2.42 | 1.59 | 287 | 155 | 163 | 84 | 5 | Choledocholithiasis |
| 7 | 25 | 27.3 | 5.7 | 7.5 | 4.6 | 206 | 133 | 185 | 247 | 8 | NR |
| 8 | 28 | 29 | 6.7 | 5.5 | 3.8 | 265 | 102 | 145 | 352 | 9 | NR |
| 9 | 29 | 20.4 | 8.8 | 2.75 | 1.8 | 46 | 37 | 167 | 138 | 5 | Choledocholithiasis |
| Mean | 28.89 | 24.10 | NA | 5.08 | 3.36 | 245.56 | NA | NA | 155.67 | 7.87 | NA |
| SD | 3.86 | 8.89 | NA | 3.08 | 1.85 | 185.64 | NA | NA | 102.24 | 3.96 | NA |
MRC: magnetic resonance cholangiography; NA: not applicable (see Results); NR: not required; SD: standard deviation.
One patient (11.1%) presented with clinical signs of cholangitis, corroborated by purulent discharge during the ERCP. Another patient had undergone laparoscopic cholecystectomy at a different hospital and was referred to our center due to the suspicion of bile duct injury after presenting with the passage of bile through the abdominal drain. As part of the diagnostic approach, MRC was performed, revealing the presence of a single stone in the distal third of the common bile duct and an intraperitoneal bile collection secondary to a cystic duct stump leak. The multidisciplinary team that included the Gynecology and Obstetrics, Gastrointestinal Endoscopy, and General Surgery Services decided the patient should undergo laparoscopic drainage of the intraperitoneal bile collection and ERCP with the rendezvous technique (anterograde introduction of the hydrophilic guidewire through the cystic duct up to the ampulla of Vater, and its recovery in the duodenal lumen through conventional duodenoscopy).
The common bile duct was selectively cannulated in 100% of the patients. In one of the patients (11.1%), the guidewire initially passed into the pancreatic duct, and so the precut sphincterotomy technique was carried out to cannulate the common bile duct. Biliary sphincterotomy with balloon sweeping was performed in 7 patients (77.7%), achieving the extraction of all stones in the common bile duct (resolved choledocholithiasis). A plastic stent was initially placed in 3 patients (2 in the third trimester and one in the second), with no further bile duct instrumentation: one was placed due to coagulopathy secondary to cholangitis and sphincterotomy was not performed; another was placed due to an 18mm stone in the proximal third of the common bile duct, whose distal diameter was 9mm, preventing the stone's expulsion; and the other was placed due to an intraperitoneal bile collection and high output bile leakage through the cystic duct stump. Once they gave birth, those 3 patients underwent a second endoscopic procedure to remove the plastic stents and definitively resolve the choledocholithiasis.
Mean radiation time was 26.67s, with a SD of 12.91. Radiation time was lower in the 2 patients in whom only a plastic stent was placed with no further bile duct instrumentation, as well as in the patient that underwent ERCP with the rendezvous technique. In that patient, anterograde cannulation of the common bile duct was performed under direct vision and the single stone reported in the MRC was spontaneously expelled when the sphincterotomy was carried out. Therefore, fluoroscopy was utilized only to corroborate the absence of other bile duct filling defects. The patient with accidental pancreatic duct cannulation, in whom the common bile duct was accessed through the precut sphincterotomy technique, had the longest radiation time (53s).
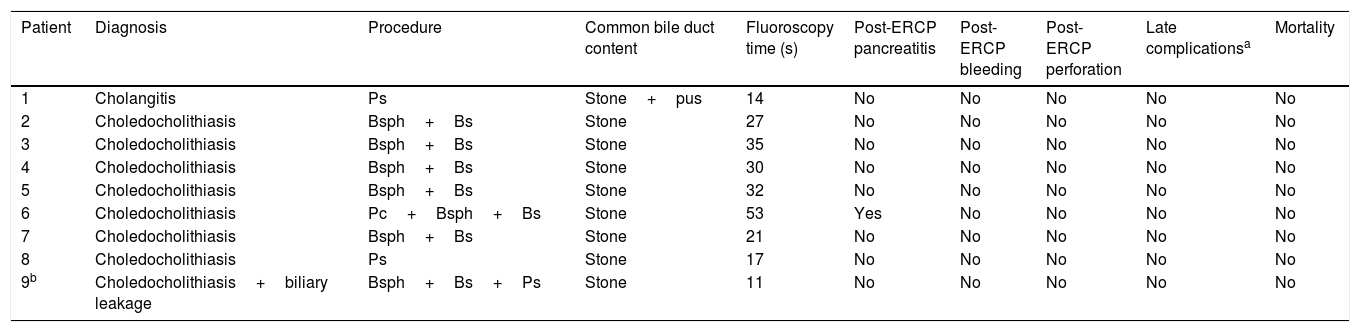
There were no maternal or fetal complications associated with sedation, nor were there cases of perforation or bleeding associated with the procedure. One patient (11.1%) developed mild post-ERCP pancreatitis that resolved in 48h with medical management (Table 2).
Maternal results.
| Patient | Diagnosis | Procedure | Common bile duct content | Fluoroscopy time (s) | Post-ERCP pancreatitis | Post-ERCP bleeding | Post-ERCP perforation | Late complicationsa | Mortality |
|---|---|---|---|---|---|---|---|---|---|
| 1 | Cholangitis | Ps | Stone+pus | 14 | No | No | No | No | No |
| 2 | Choledocholithiasis | Bsph+Bs | Stone | 27 | No | No | No | No | No |
| 3 | Choledocholithiasis | Bsph+Bs | Stone | 35 | No | No | No | No | No |
| 4 | Choledocholithiasis | Bsph+Bs | Stone | 30 | No | No | No | No | No |
| 5 | Choledocholithiasis | Bsph+Bs | Stone | 32 | No | No | No | No | No |
| 6 | Choledocholithiasis | Pc+Bsph+Bs | Stone | 53 | Yes | No | No | No | No |
| 7 | Choledocholithiasis | Bsph+Bs | Stone | 21 | No | No | No | No | No |
| 8 | Choledocholithiasis | Ps | Stone | 17 | No | No | No | No | No |
| 9b | Choledocholithiasis+biliary leakage | Bsph+Bs+Ps | Stone | 11 | No | No | No | No | No |
Bs: balloon sweep; Bsph: biliary sphincterotomy; Pc: Precut; Ps: plastic stent.
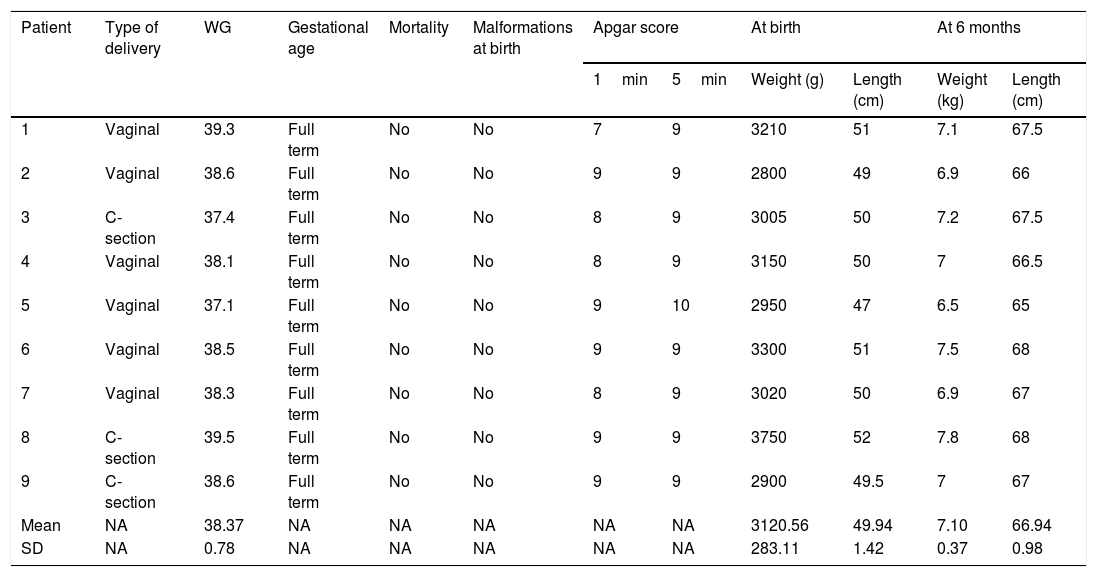
Delivery was vaginal in 6 patients (66.7%) and the other 3 patients (33.3%) underwent C-section. Pregnancy was normal in 100% of the patients, resulting in the birth of full-term neonates (mean gestational age at birth was 38.37 weeks, with a SD of 0.78). There were no cases of fetal mortality or malformations at birth. The Apgar score was normal in 100% of the neonates (above 7), mean birthweight was 3120.56g, with a SD of 283.11, and mean length at birth was 49.94cm, with a SD of 1.42.
At the follow-up appointment at 6 months, all the infants presented with adequate weight-for-age (mean weight of 7.10kg, with a SD of 0.37) and normal length-for-age (mean length of 66.94cm, with a SD of 0.98) (Table 3).
Fetal results.
| Patient | Type of delivery | WG | Gestational age | Mortality | Malformations at birth | Apgar score | At birth | At 6 months | |||
|---|---|---|---|---|---|---|---|---|---|---|---|
| 1min | 5min | Weight (g) | Length (cm) | Weight (kg) | Length (cm) | ||||||
| 1 | Vaginal | 39.3 | Full term | No | No | 7 | 9 | 3210 | 51 | 7.1 | 67.5 |
| 2 | Vaginal | 38.6 | Full term | No | No | 9 | 9 | 2800 | 49 | 6.9 | 66 |
| 3 | C-section | 37.4 | Full term | No | No | 8 | 9 | 3005 | 50 | 7.2 | 67.5 |
| 4 | Vaginal | 38.1 | Full term | No | No | 8 | 9 | 3150 | 50 | 7 | 66.5 |
| 5 | Vaginal | 37.1 | Full term | No | No | 9 | 10 | 2950 | 47 | 6.5 | 65 |
| 6 | Vaginal | 38.5 | Full term | No | No | 9 | 9 | 3300 | 51 | 7.5 | 68 |
| 7 | Vaginal | 38.3 | Full term | No | No | 8 | 9 | 3020 | 50 | 6.9 | 67 |
| 8 | C-section | 39.5 | Full term | No | No | 9 | 9 | 3750 | 52 | 7.8 | 68 |
| 9 | C-section | 38.6 | Full term | No | No | 9 | 9 | 2900 | 49.5 | 7 | 67 |
| Mean | NA | 38.37 | NA | NA | NA | NA | NA | 3120.56 | 49.94 | 7.10 | 66.94 |
| SD | NA | 0.78 | NA | NA | NA | NA | NA | 283.11 | 1.42 | 0.37 | 0.98 |
NA: not applicable; SD: standard deviation; WG: weeks of gestation at the time of birth.
For the past 20 years, ERCP has been considered the treatment of choice for symptomatic choledocholithiasis in pregnant women. Different case series have shown its effectiveness and adequate safety profile. The first case series was published in 1990, conducted by Braillie et al., and included 5 pregnant patients that underwent ERCP due to choledocholithiasis. The disease was resolved in all cases, and no adverse effects were reported in the mothers or fetuses.8
In a case series published in 2009, Tang et al. reported the results of 65 pregnant patients that underwent ERCP. Mean fluoroscopy time was 1:45min and the rate of post-ERCP pancreatitis was 16%. No adverse effects were reported in the fetuses at birth, but there was a higher rate of pre-term deliveries in the patients that underwent ERCP during the first trimester (20% vs. 4% in the rest of the patients).9
In 2011, Cappell conducted a systematic review of the literature that included 46 studies and 296 pregnant patients that underwent ERCP due to symptomatic choledocholithiasis. Of those patients, 6.4% presented with post-ERCP pancreatitis and 1% presented with gastrointestinal bleeding associated with sphincterotomy. A total of 8.1% of the patients required 2 or more ERCPs during the same pregnancy. Fluoroscopy time was not reported in all the studies of the review, and the mean times of those reported varied greatly, ranging from as short as 3s to as long as 105s.10
In an effort to eliminate stochastic effects (not dependent on the radiation dose administered), an ERCP technique not using fluoroscopy has been proposed. It consists of the cannulation of the suspected bile duct, confirmed through bile aspiration, and followed by sphincterotomy and balloon sweeping. To ensure that the ERCP has been successful, an endoscopic ultrasound study is required prior to the procedure that shows the number of stones present in the bile duct, so that the same number of stones are removed during the ERCP.1,2
In their case series published in 2009, Akcakaya et al. reported on 6 pregnant patients that underwent ERCP without fluoroscopy. None of the patients presented with post-ERCP complications (pancreatitis, bleeding, perforation, etc.), abortions, pre-term deliveries, or neonates with malformations.2
Published in 2016, Ersoz et al. conducted a retrospective case series on pregnant patients that underwent nonradiation ERCP. It included 22 patients that underwent ERCP with biliary sphincterotomy and balloon dilation of the common bile duct. Two of the patients (9%) presented with post-ERCP pancreatitis and one of them (4.5%) presented with gastrointestinal bleeding associated with the sphincterotomy. Pregnancy was normal in all the cases, with each patient giving birth to a healthy, full-term neonate.1
In 2014, Wu et al. conducted a systematic review of the literature that included 180 pregnant patients from 22 studies that underwent nonradiation ERCP. They reported a post-ERCP pancreatitis rate of 1.1%, bleeding of 2.2%, and incomplete stone extraction requiring a second endoscopic procedure during the same pregnancy of 6.7%. Because nonradiation ERCP is technically demanding, those cases are usually referred to tertiary care centers that have expert endoscopists, possibly explaining the low complication rates reported.11
The results from our hospital coincide with those reported internationally, demonstrating that ERCP is a feasible, safe, and efficacious method in our medical environment for both the mother and fetus. Therefore, in the hands of the experienced endoscopist, it should be considered the option of choice for treating symptomatic choledocholithiasis in pregnant patients.
To obtain good results, it is essential to strictly follow the safety protocols established in the international guidelines: pre-procedure and post-procedure obstetric evaluation, use of category A or B drugs at the lowest possible dose for sedation performed by an anesthesiologist, placement of the patient in the left lateral decubitus position to prevent compression of the vena cava, maternal heart beat monitoring during the procedure, etc.
Finally, we consider that even though the development of nonradiation ERCP techniques is a plausible effort for eliminating the possible harmful effects of radiation on the mother and fetus, those methods still have certain limitations that make their generalized application in our medical environment difficult. First, they are only useful in uncomplicated patients, given that patients with difficult stones or with other pathologies, such as biliary leakage or bile duct stricture, inevitably require fluoroscopy. Second, the majority of endoscopic units in Mexico do not have endoscopic ultrasound equipment, and even if they did, costs would increase considerably.
In our opinion, the abovementioned disadvantages of nonradiation ERCP, added to the adequate safety profile in terms of morbidity and mortality of reduced-radiation ERCP, make the reduced-radiation method the more feasible and efficacious technique for the treatment of choledocholithiasis in pregnant patients in our medical environment.
Financial disclosureNo financial support was received in relation to this study/article.
Conflict of interestThe authors declare that there is no conflict of interest.
Please cite this article as: Arce-Liévano E, del Río-Suárez I, Valenzuela-Salazar C, Délano-Alonso R, Bada-Yllán O, Herrera-Esquivel JJ, et al. Resultados de la colangiopancreatografía retrógrada endoscópica para el tratamiento de la coledocolitiasis sintomática en pacientes embarazadas: Experiencia reciente de un hospital de segundo nivel de la Ciudad de México. Revista de Gastroenterología de México. 2021;86:21–27.