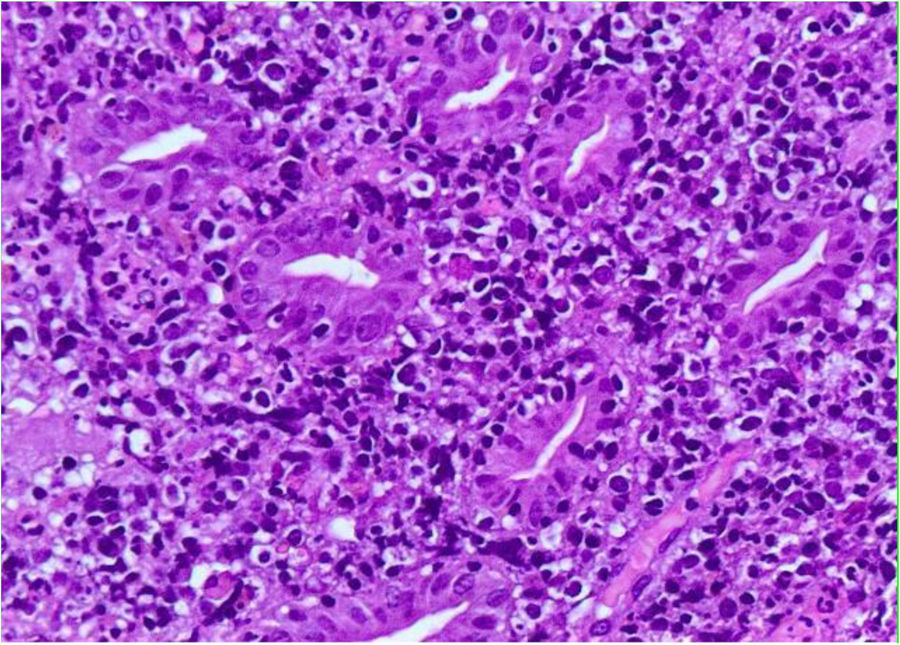
An 83-year-old man with a past medical history of initial stage chronic lymphocytic leukemia (Rai 0/Binet A) was admitted to the hospital due to nausea, vomiting, and constipation of several days’ progression. An abdominal CT scan showed thickening of the walls of the third and fourth parts of the duodenum, as well as a large aortic aneurysm extrinsically compressing the duodenum (Fig. 1). A gastroduodenoscopy revealed an almost completely ulcerated stricture in the third part of the duodenum (Figs. 2 and 3). Biopsy showed large lymphoid cells infiltrating the duodenal mucosa that were scarcely cohesive, with scant cytoplasm, positive for CD 20, and negative for CD 3 (Fig. 4), consistent with large B-cell lymphoma. Richter’s syndrome appears in 2-10% of the patients with chronic lymphocytic leukemia, and is its transformation into an aggressive lymphoma, usually diffuse large B-cell lymphoma. It generally manifests with adenopathies, splenomegaly, and worsening of B symptoms. Our patient presented with symptoms of partial obstruction and chemotherapy was begun. He received 3 cycles (2 R-miniCHOP and R-GemOx-Dex), with no improvement, and finally underwent laparoscopic gastrojejunostomy. Progression was unfavorable and in the following weeks he presented with acute abdomen secondary to extensive mesenteric ischemia. He was operated on again but died in the postoperative period.
The gastrointestinal location of Richter’s syndrome is very rare. There are only ten cases described in the literature, at different levels of the digestive tract (stomach, colon, or rectum) and with diverse clinical manifestations, such as recurrent gastric ulcer, perforation, intestinal obstruction, and gastrointestinal bleeding.
Ethical considerationsThe authors declare that no experiments were performed on humans or animals for this study. They have followed the protocols of their work center in relation to the publication of patient data, preserving absolute patient confidentiality and anonymity. Therefore, requesting informed consent for the publication of this article was not required.
Protection of human and animal subjects. The authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of data. The authors declare that they have followed the protocols of their work center on the publication of patient data.
Right to privacy and informed consent. The authors declare that they have preserved absolute patient anonymity. Therefore, requesting informed consent for the publication of this article was not required.
Financial disclosureNo financial support was received in relation to this study/article.
Conflict of interestThe authors declare that there is no conflict of interest.
Please cite this article as: Arenas García V, Casal Álvarez J, Cano Calderero FX. Estenosis duodenal secundaria a síndrome de Richter. Revista de Gastroenterología de México. 2020;85:207–208.