First described by Thilesus in 16701, cholecystocutaneous fistula (CCF) is the connection of the gallbladder to the external environment, through a rupture in the layers of the abdominal wall, forming a fistulous tract2. In the nineteenth century (1890), Courvoisier reported 169 cases from a case series of 499 perforations of the gallbladder. The last case series was published in 1949; the authors were Henry and Orr and they reported 37 cases3.
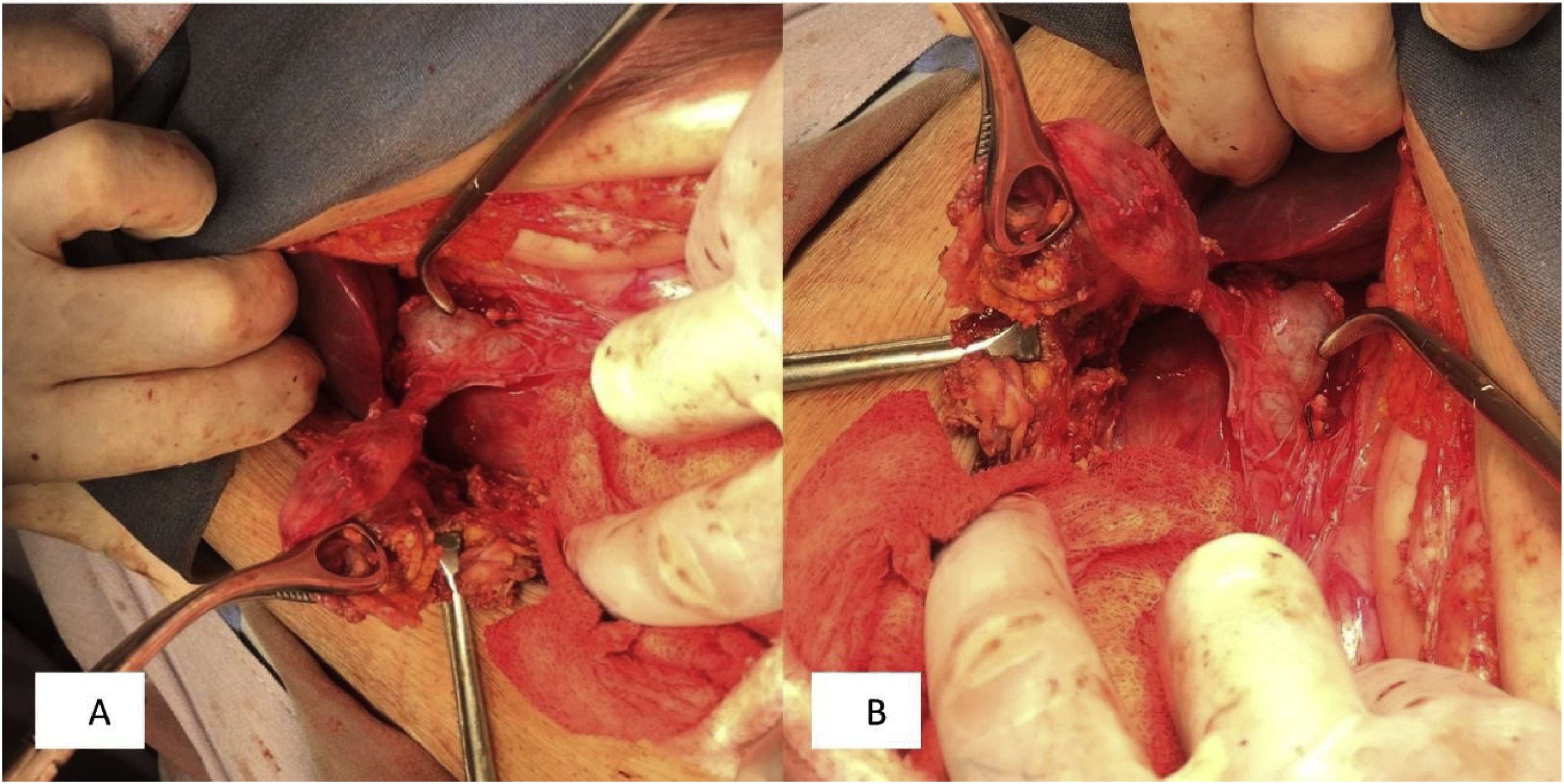
We present herein the case of a 73-year-old woman that had no past medical history of chronic-degenerative diseases or surgical interventions. Two weeks prior to hospital admission, she presented with an increase in volume in the left flank, and one week before, local hyperemia and hyperthermia. A fetid green exudate then began to seep out of the umbilicus, accompanied by moderate abdominal pain, for which the patient sought medical attention. Her vital signs at admission were blood pressure, 110/60 mmHg; heart rate, 105 beats per minute; respiratory rate, 16 breaths per minute; and temperature, 37.8 °C. Physical examination revealed no hernial defect, only the presence of a fetid, apparently intestinal exudate, draining from the umbilicus. An approximately 8 × 10 cm region of the wall of the left flank was hyperthermal and hyperemic, indurated, and severely painful when palpated. Rebound tenderness was present and peristalsis was reduced (Fig. 1). Laboratory work-up reported hemoglobin, 10 g/dl; leukocytes, 3.8 cells/mm3; neutrophils, 98%, with toxic granulations; platelets, 150,000; sodium, 129 mmol/l; potassium, 2.9 mmol/l; chloride, 115 mmol/l; glucose, 76 mg/dl; and creatinine, 2.1 mg/dl. Due to the signs of peritoneal irritation, associated with a systemic inflammatory response (tachycardia, leukopenia, and neutrophilia), together with the lack of an imaging study, emergency surgery was decided upon, with the suspicion of abdominal sepsis and a probable enterocutaneous fistula. An exploratory laparotomy was performed that produced the following findings: a 300 ml abscess in the abdominal wall, connected to the abdominal cavity; destruction of the aponeurosis, with a 12 × 15 cm defect; and the presence of a cholecystocutaneous fistula at the level of the umbilicus (Fig. 2). Fistulectomy was performed and no stones were observed (Fig. 3). The aponeurosis was closed, employing tension, and the use of prosthetic material was ruled out due to the type of intervention. A carbapenem was administered during the postoperative period, and given the patient’s favorable progression, she was released.
CCFs account for 8 to 26.5% of cholecystoenteric fistulas and are the second most common fistulas, after cholecystoduodenal fistula. According to Costi et al., the female/male ratio is 2.47:1. The mean age of patients at diagnosis is 68.9 years (range 37–90), and more specifically, 70.8 years in Western articles and 62.1 years in Asian reports4.
Gallbladder neoplasia, anatomic anomalies, and injuries related to surgical procedures stand out among the causes of CCF, albeit the majority are associated with gallstones5. Polyarteritis nodosa, corticosteroid therapy, typhoid fever, and trauma have been described as predisposing factors3,6.
The pathophysiology begins with the increase in the intraluminal pressure of the gallbladder, secondary to obstruction caused by stones, impeding the blood flow and lymphatic drainage, resulting in wall necrosis and perforation. It can be an acute event that leads to peritonitis and abscesses surrounding the gallbladder, or to a chronic process that conditions the formation of internal and external fistulas, mainly from the fundus of the gallbladder1. Perforation of the gallbladder generally occurs at the level of the fundus6.
Biliary fistulas are classified into two groups: internal and external. The latter connect to any part of the anterior surface of the trunk. Seventy-five percent of internal fistulas connect to the duodenum, 15% to the colon, and 10% to the jejunum, stomach, or bronchi2.
A fistula tends to become evident upon the discharge of bile or stones through the abdominal wall. The most common site of the opening is the upper abdominal quadrant and the right flank or the umbilical orifice. Sites can also include the left lateral costal margin, the right iliac fossa, the right groin, or the right gluteus. Its presentation can also be more insidious and its diagnosis more difficult, when only pus is drained or subcutaneous abscesses are formed6,7. Abscesses are recurrent, usually with no other accompanying symptomatology, and even cases of acalculous fistula have been described. When an abscess persists after having been drained multiple times, the diagnosis of fistula should be suggested, and in cases of unexplained suppuration or wall cellulitis, a routine imaging study should be performed3.
Abdominal ultrasound or tomography are useful for making the diagnosis, but fistulography is the confirmatory imaging study, enabling visualization of the tract3. Cholecystocutaneous fistula can be treated with two different strategies. The first entails a two-step approach: percutaneous drainage and antibiotic therapy, followed by cholecystectomy. The second directly involves the performance of cholecystectomy, through laparotomy, with en bloc excision of the aponeurotic sheath, skin, and fistula orifice. The two-step approach is reserved for patients with sepsis and poor general condition8, such as the patient in our report.
Ethical considerationsThe authors declare that all ethical responsibilities in relation to data protection, the right to privacy, and informed consent were met.
Authorization by the institutional ethics committee was not required, given that no patient anonymity norms were unmet or violated and no experimental procedures putting the patient’s integrity at risk were performed.
The authors declare that this article contains no personal data that could identify the patient.
Financial disclosureNo specific grants were received from public sector agencies, the business sector, or non-profit organizations in relation to this study.
Conflict of interestThe authors declare that there is no conflict of interest.
Please cite this article as: Ballesteros-Suárez E, Navarro-Tovar F, Díaz-Barrientos CZ, Marín-Pardo EI, Hernández-Pérez E. Fístula colecistocutánea, una patología poco común en la actualidad. Rev Gastroenterol Méx. 2023;88:177–179.