A 65-year-old previously healthy woman presented with general malaise, headache, and unintentional weight loss of 7 kg of one-month progression.
She sought medical attention in the private sector and the physician documented anemia, with hemoglobin of 4.6 g/dl, mean corpuscular volume of 66.60 fl, and mean corpuscular hemoglobin of 19.60 pg. Considering the diagnosis of hypochromic microcytic anemia, complementary laboratory studies with an iron profile were performed: serum iron, 14.70 µg/dl (50–212 µg/dl); total iron binding capacity, 501.30 µg/dL (155–355 µg/dl); ferritin, 11.52 ng/ml (11–306.8 ng/ml); and transferrin saturation index, 2.93% (14–50%). Iron deficiency anemia was suspected, and treatment was begun with oral and intravenous iron. Endoscopy of the proximal gastrointestinal tract, reaching the third portion of the duodenum, was carried out, with normal macroscopic findings. Colonoscopy was performed up to the ileocecal valve with no relevant data. Three months later, the patient continued to present with anemia and general malaise. Bone marrow biopsy and aspirate were carried out that showed adequate development of the 3 hematopoietic lines.
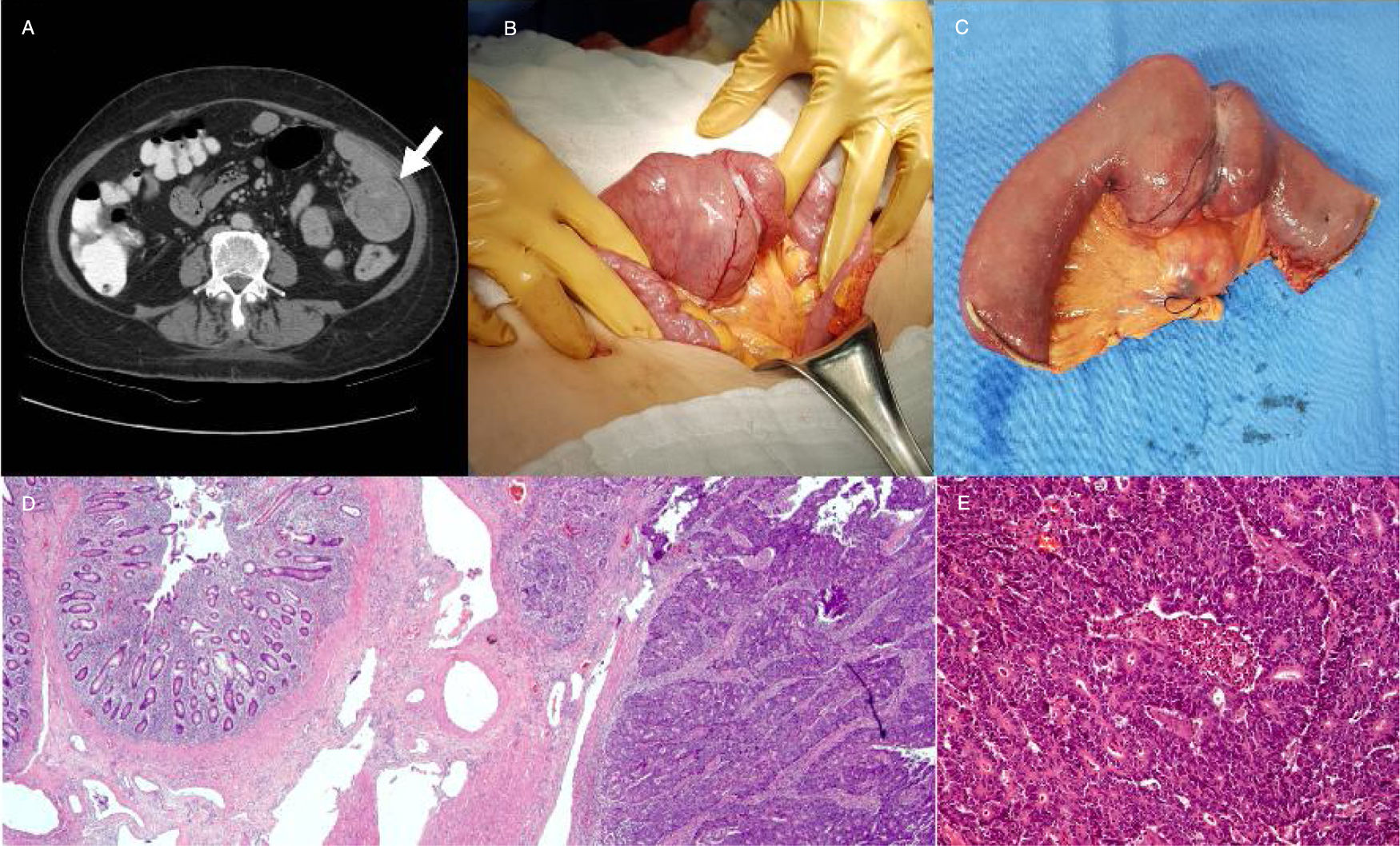
Due to symptom persistence, the patient was referred to our hospital center. The initial evaluation revealed hemoglobin of 9.2 g/dl, mean corpuscular volume of 28.2 pg, and reticulocytes of 3.42%. The iron profile showed serum iron, 3 µg/g; total iron binding capacity, 237 µg/dl; ferritin, 13.6 ng/ml; and transferrin saturation index, 1%. Abdominal computed tomography scan identified jejunal thickening secondary to a lesion with an infiltrating aspect that conditioned partial intestinal obstruction (Fig. 1A). Enteroscopy study revealed an exophytic tumor located 50 cm from the pylorus, occluding 90% of the intestinal lumen. Biopsy was performed and the histopathologic report stated moderately differentiated adenocarcinoma. Surgical treatment was proposed. Supraumbilical midline laparotomy identified a tumor in the proximal region of the jejunum, with no infiltration into the neighboring structures or signs of peritoneal metastases. Fifteen centimeters of the proximal jejunum were resected, and an end-to-end manual anastomosis was performed. A segment of the adjacent mesentery was also resected, following oncologic principles, with dissection of the adipose tissue and lymph nodes up to the mesenteric root (Fig. 1B and C). The histopathologic report confirmed the diagnosis of moderately differentiated adenocarcinoma and stated there was no infiltration into the serosa, surgical margins were negative, and there was metastasis to one of the eighteen lymph nodes (Fig. 1D and E). In the postoperative period, the patient tolerated oral diet, had no abdominal pain, and no signs of a systemic inflammatory response. She was released from the hospital on postoperative day 5 and is currently under an adjuvant chemotherapy regimen of folinic acid, fluorouracil, and oxaliplatin.
A) Computed tomography scan showing the thickening of the proximal jejunum that conditioned partial bowel obstruction. B and C) Jejunal resection with regional mesenteric lymphadenectomy. D and E) Malignant epithelial tumor arranged in nests, with a cribriform pattern, corresponding to moderately differentiated adenocarcinoma, with no infiltration into the serosa.
Small bowel malignant tumors are rare and account for 2% of all primary gastrointestinal cancers.1 The incidence of adenocarcinoma is greater in the seventh decade of life, albeit the disease can present at earlier ages in patients with predisposing conditions, such as inflammatory bowel disease, familial adenomatous polyposis, nonpolyposis colorectal cancer, or celiac disease.2 Small bowel adenocarcinomas are asymptomatic in the early stages, delaying diagnosis for approximately 6 to 8 months, but as the disease progresses, symptoms such as abdominal pain and gastrointestinal bleeding present.3 The scenario of a patient with weight loss and anemia of unidentified cause should always lead to the suspicion of a neoplastic process. Thus, extension studies should be focused on the detection of lesions in the jejunum-ileum. Because of their location, they are not accessible through the conventional screening methods of routine colonoscopy and endoscopy. Currently, the main treatment is the segmental resection of the small bowel with negative surgical margins and regional mesenteric lymphadenectomy.4 Adjuvant chemotherapy for clinical stage III small bowel adenocarcinoma improves general survival and current first-line treatment is capecitabin or 5-fluorouracil combined with oxaliplatin.5
In conclusion, adenocarcinoma of the jejunum is a diagnostic challenge for the physician due to its extreme rareness. As with other malignant tumors, patient survival is related to the clinical stage of the disease at the time of diagnosis. Therefore, when there is anemia with probable chronic bleeding as the cause, a small bowel neoplastic lesion should be suspected, and extension studies should be focused on corroborating or ruling out said pathology.
Ethical disclosuresProtection of human and animal subjects. The authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of data. The authors declare that they have followed the protocols of their work center on the publication of patient data, protecting patient anonymity.
Right to privacy and informed consent. The authors have obtained the written informed consent of the patients or subjects mentioned in the article. The corresponding author is in possession of this document.
Financial disclosureNo financial support was received in relation to this article.
Conflict of interestThe authors declare that there is no conflict of interest.
Please cite this article as: Sánchez-Morales GE, Moctezuma-Velázquez P, Padrón-Martínez AC, Núñez-Saavedra IJ, Medina-Franco H. Adenocarcinoma de yeyuno, lección aprendida de un diagnóstico tardío. Revista de Gastroenterología de México. 2020;85:213–214.