SARS-CoV-2 emerged in 2019 and had a huge impact on the world. The area of endoscopy suffered great changes, causing a reduction in the number of procedures and its indications. The aim of our study was to compare the quantity, indication, and type of procedures in 2019 with those in 2020.
MethodA retrospective, observational, analytic, and cross-sectional study was conducted, obtaining information from the endoscopy registry. The STROBE checklist was employed.
Statistical analysisThe quantitative variables were analyzed with descriptive statistics (measures of central tendency and dispersion) and the categorical variables with frequencies and percentages. The quantitative variables were compared, using the Student’s t test/Mann–Whitney U test, and the categorical variables with contingency tables, using the Fisher’s exact test.
ResultsIn 2019, a total of 277 procedures were performed, compared with 139 in 2020. Mean patient age was 98.53 months (61.46 SD) in 2019 and 77.02 months (59.81 SD) in 2020; 352 diagnostic procedures and 136 therapeutic procedures were carried out in 2019, compared with 51 diagnostic procedures and 88 therapeutic procedures in 2020. The number of diagnostic and therapeutic procedures were inverted (72.1%–36.7% and 27.9%–63.3%, respectively) (p<0.0001). Esophageal varices, upper gastrointestinal bleeding (UGIB), and foreign body extraction were the indications, in order of predominance in 2019, compared with foreign body extraction (p<0.05), UGIB, and esophageal varices in 2020. There were no differences regarding colonoscopy.
ConclusionThere was a clear difference in indication and type of procedure, with an increase in foreign body extraction in preschoolers.
En 2019 surgió el SARS-CoV-2 que tuvo un gran impacto a nivel mundial, el área de endoscopia sufrió grandes cambios provocando una reducción del número de procedimientos y sus indicaciones.
ObjetivoComparar: cantidad, indicación y tipo de procedimientos del 2019 contra 2020.
MétodoEstudio observacional, analítico, transversal y retrospectivo obteniendo la información del registro de endoscopia. Se utilizó la lista de cotejo STROBE.
Análisis estadísticoVariables cuantitativas analizadas con estadística descriptiva (medidas de tendencia central y dispersión) y para las categóricas, frecuencias y porcentajes. Para comparar se utilizó T de Student/U de Mann-Whitney para las variables cuantitativas; tablas de contingencia con prueba Ji cuadrada o exacta de Fisher para categóricas.
ResultadosEn el 2019 se realizaron 277 procedimientos en comparación de 139 en 2020. Media de edad en el 2019 fue de 98.53 meses (DE 61.46) y para el 2020 la media fue 77.02 (DE 59.81), tipo de procedimiento en 2019, 352 fueron procedimientos diagnósticos y 136 terapéuticos, mientras que, en 2020, 51 fueron diagnósticos y 88 terapéuticos. Se invirtió la proporción de procedimientos diagnósticos (72.1% al 36.7%) y terapéuticos (27.9% a 63.3%), (p<0.0001). Las indicaciones en 2019 predominaron várices esofágicas, hemorragia de tubo digestivo alto (HTDA) y extracción de cuerpo extraño, en comparación con el 2020 donde predominó extracción de cuerpo extraño (p<0.05), HTDA y várices esofágicas. En la colonoscopia no hubo diferencias.
ConclusiónHubo una clara diferencia en la indicación y tipo de procedimiento, hubo un incremento en la extracción de cuerpos extraños en pre-escolares.
In 2019, a new highly contagious virus named SARS-CoV-2, associated with severe acute respiratory syndrome, emerged.1–3 In January 2020, the World Health Organization (WHO) declared the presence of this virus to be a Public Health Emergency of International Concern, and in March of the same year, a pandemic.2 The SARS-CoV-2 world crisis has negatively impacted the number and type of surgical procedures performed due to the need to recategorize emergency, urgent, and elective procedures.4–6As a consequence, this brought about an 81.4% reduction in endoscopic procedures, according to a survey conducted by the European Society of Paediatric Gastroenterology, Hepatology and Nutrition (ESPGHAN).7
By January 25, 2021, there were an estimated 1,771,749 persons infected with COVID-19 and 150,273 deaths from the disease in Mexico, signifying a lethality of 6%.8 This infection rate was reflected at the Instituto Nacional de Pediatría, resulting in the temporary closure of the endoscopy units due to a lack of negative pressure and laminar flow. Consequently, procedures have had to be restricted to operating rooms, and because they must also be used by the rest of the surgical services, this has caused an important decrease in the performance of endoscopic procedures.
The aim of the present study was to compare the number and type of endoscopic procedures performed at the Gastroenterology and Nutrition Service of the Instituto Nacional de Pediatría, before and during the SARS-CoV-2 pandemic.
Materials and methodsA retrospective, observational, analytic, and cross-sectional study was conducted at the Instituto Nacional de Pediatría. The STROBE checklist for cross-sectional studies was utilized. Records from January to December of 2019 from the area of endoscopy were reviewed and compared with the records from 2020. The demographic characteristics, indications for the procedure, type of procedure, and endoscopic findings were obtained.
Because of its retrospective design, the study was classified as negligible-risk research. Based on the Regulation of the General Health Law in Health Research, Second Title, of the Ethical Aspects in Research on Humans, Chapter 1, Article 23, given that this is a negligible-risk analysis, informed consent was not requested.
Statistical analysisThe analysis was carried out, using the SPSS version 22.0 program. Through descriptive statistics, the quantitative variables were expressed as measures of central tendency and dispersion and the categorical variables as frequencies and percentages. The Student’s t test or Mann-Whitney test were utilized to compare the quantitative variables, and contingency tables with the Fisher’s exact test to compare the categorical variables.
Ethical considerationsThe study was conducted following the international regulations in bioethics and met the norms of the Instituto Nacional de Pediatría. It was reviewed by the institutional ethics committee. No experiments were carried out on humans or animals and there was complete data confidentiality. This study is classified as a negligible-risk study, given that clinical records were reviewed, retrospective documental research methods and techniques were employed, and no interventions on or intentional modifications of the physiologic, psychologic, and social variables of the individuals that participated in the study were performed, thus informed consent was not required.
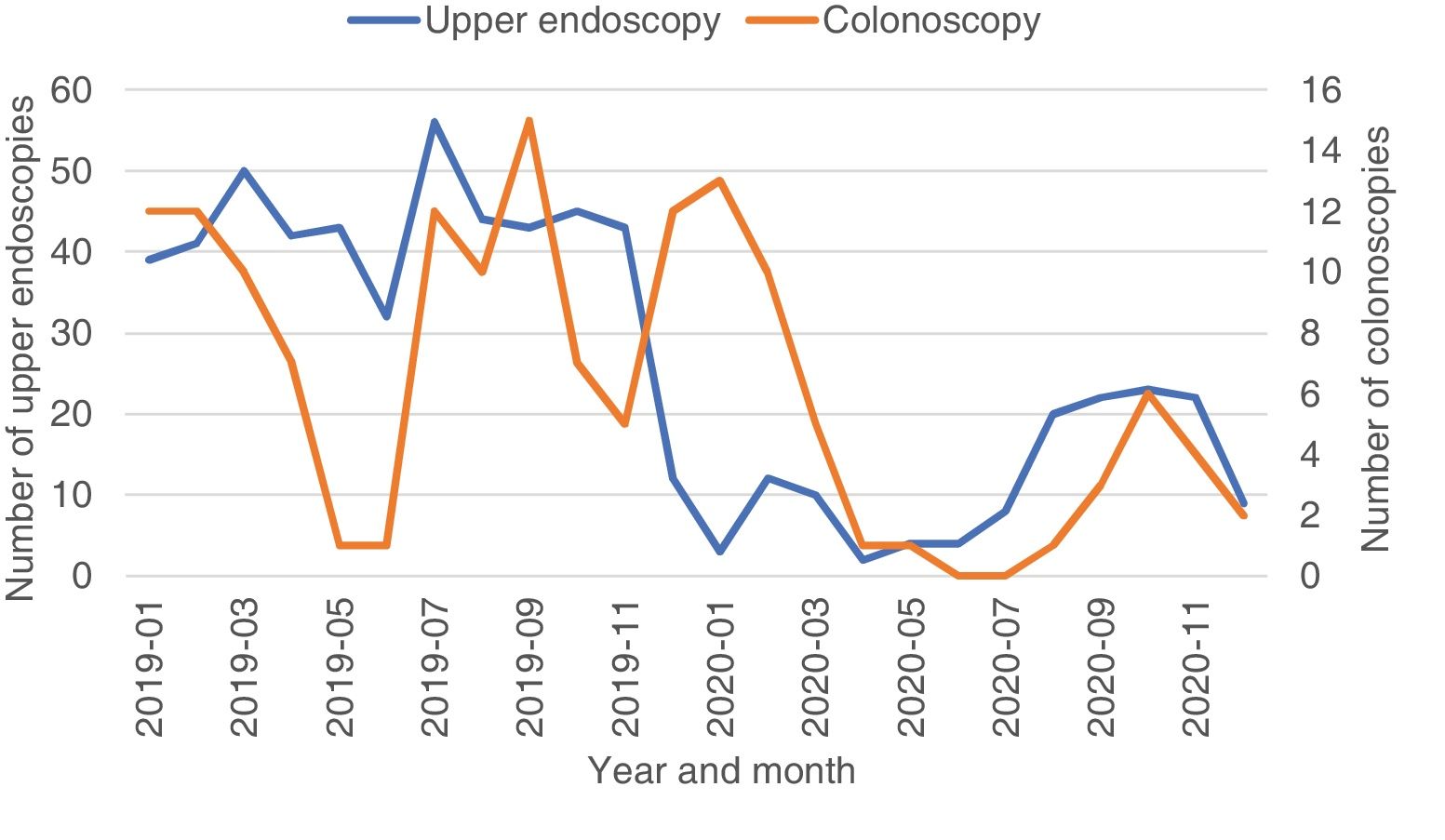
ResultsUpper endoscopyIn the descriptive analysis, a total of 277 upper endoscopy procedures were performed in 2019, compared with 139 procedures in 2020 (Fig. 1). In 2019, mean patient age was 98.53 months (61.46 standard deviation [SD]), whereas in 2020, it was 77.02 months (59.81 SD). In 2019, the procedures were performed on 277 males and 213 females, whereas they were performed on 79 males and 60 females in 2020. In 2020, there was no statistically significant difference by sex, with respect to the number of patients treated (p>0.999).
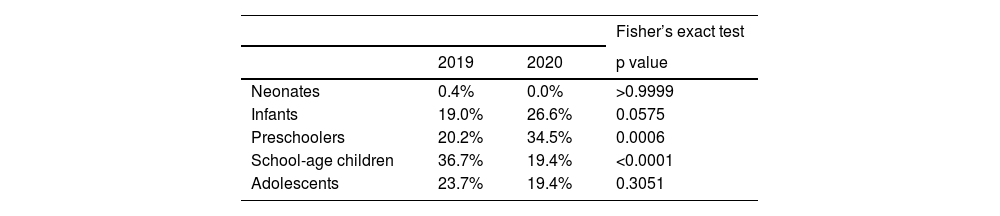
The patients were divided into age groups and Table 1 shows the comparison made between 2019 and 2020, using the Fisher’s exact test.
Regarding the type of procedure, in 2019, 352 were diagnostic procedures and 136 were therapeutic, whereas in 2020, 51 were diagnostic and 88 were therapeutic, resulting in an inversion in the number of diagnostic procedures (from 72.1% to 36.7%) and therapeutic procedures (from 27.9% to 63.3%), (p<0.0001).
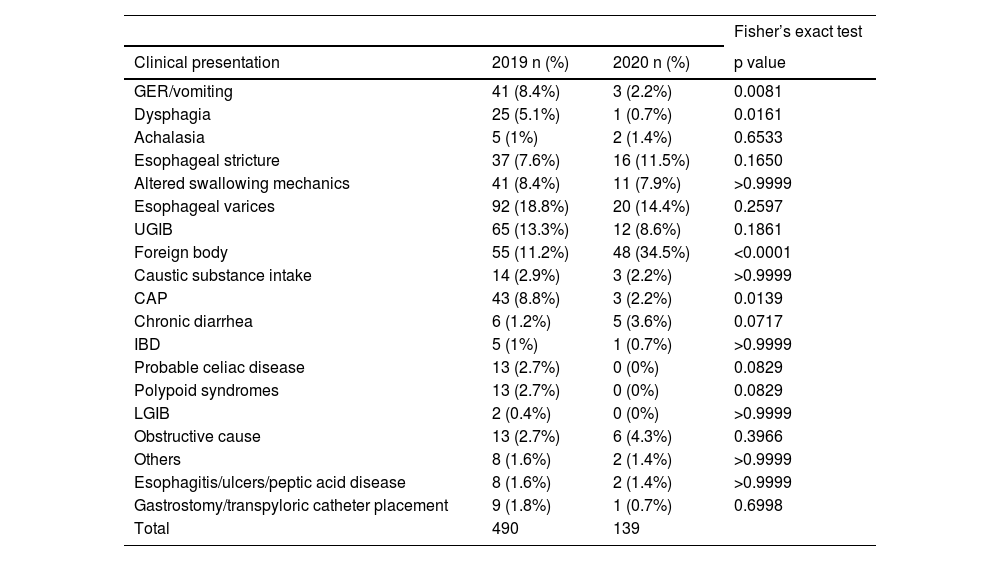
With respect to indications for upper endoscopy, in 2019, the order of predominance was esophageal varices, upper gastrointestinal bleeding (UGIB), and foreign body extraction, compared with foreign body extraction, UGIB, and esophageal varices in 2020. Table 2 shows all the indications.
Indications for upper endoscopy.
| Fisher’s exact test | |||
|---|---|---|---|
| Clinical presentation | 2019 n (%) | 2020 n (%) | p value |
| GER/vomiting | 41 (8.4%) | 3 (2.2%) | 0.0081 |
| Dysphagia | 25 (5.1%) | 1 (0.7%) | 0.0161 |
| Achalasia | 5 (1%) | 2 (1.4%) | 0.6533 |
| Esophageal stricture | 37 (7.6%) | 16 (11.5%) | 0.1650 |
| Altered swallowing mechanics | 41 (8.4%) | 11 (7.9%) | >0.9999 |
| Esophageal varices | 92 (18.8%) | 20 (14.4%) | 0.2597 |
| UGIB | 65 (13.3%) | 12 (8.6%) | 0.1861 |
| Foreign body | 55 (11.2%) | 48 (34.5%) | <0.0001 |
| Caustic substance intake | 14 (2.9%) | 3 (2.2%) | >0.9999 |
| CAP | 43 (8.8%) | 3 (2.2%) | 0.0139 |
| Chronic diarrhea | 6 (1.2%) | 5 (3.6%) | 0.0717 |
| IBD | 5 (1%) | 1 (0.7%) | >0.9999 |
| Probable celiac disease | 13 (2.7%) | 0 (0%) | 0.0829 |
| Polypoid syndromes | 13 (2.7%) | 0 (0%) | 0.0829 |
| LGIB | 2 (0.4%) | 0 (0%) | >0.9999 |
| Obstructive cause | 13 (2.7%) | 6 (4.3%) | 0.3966 |
| Others | 8 (1.6%) | 2 (1.4%) | >0.9999 |
| Esophagitis/ulcers/peptic acid disease | 8 (1.6%) | 2 (1.4%) | >0.9999 |
| Gastrostomy/transpyloric catheter placement | 9 (1.8%) | 1 (0.7%) | 0.6998 |
| Total | 490 | 139 | |
CAP: chronic abdominal pain; GER: gastroesophageal reflux; IBD: inflammatory bowel disease; LGIB: lower gastrointestinal bleeding; UGIB: upper gastrointestinal bleeding.
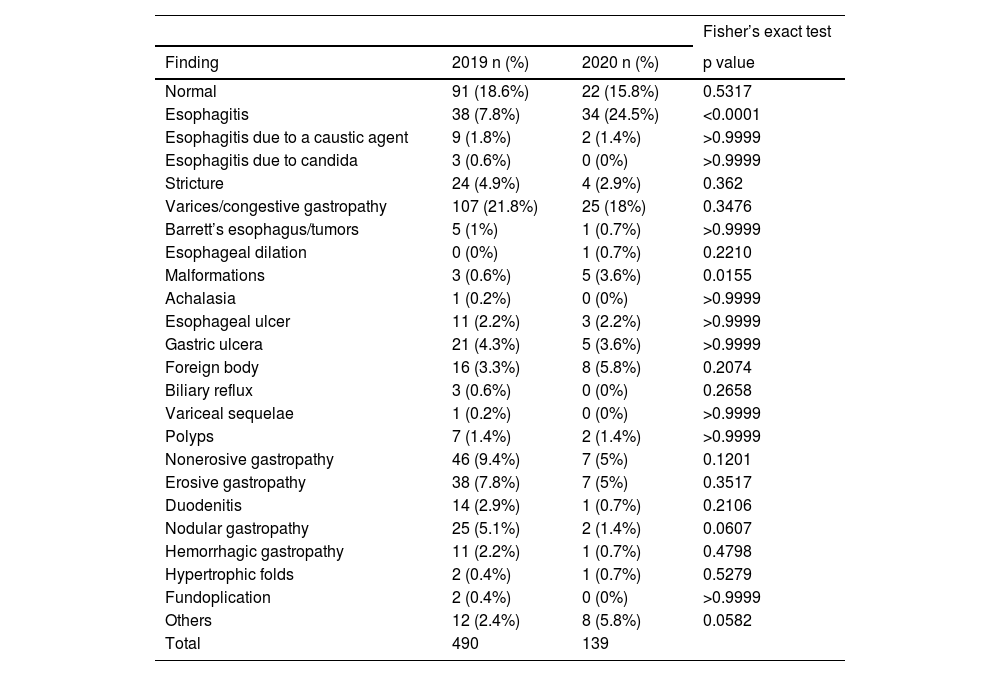
Table 3 shows that esophagitis and malformations were the findings that were significantly increased in 2020.
Endoscopic findings.
| Fisher’s exact test | |||
|---|---|---|---|
| Finding | 2019 n (%) | 2020 n (%) | p value |
| Normal | 91 (18.6%) | 22 (15.8%) | 0.5317 |
| Esophagitis | 38 (7.8%) | 34 (24.5%) | <0.0001 |
| Esophagitis due to a caustic agent | 9 (1.8%) | 2 (1.4%) | >0.9999 |
| Esophagitis due to candida | 3 (0.6%) | 0 (0%) | >0.9999 |
| Stricture | 24 (4.9%) | 4 (2.9%) | 0.362 |
| Varices/congestive gastropathy | 107 (21.8%) | 25 (18%) | 0.3476 |
| Barrett’s esophagus/tumors | 5 (1%) | 1 (0.7%) | >0.9999 |
| Esophageal dilation | 0 (0%) | 1 (0.7%) | 0.2210 |
| Malformations | 3 (0.6%) | 5 (3.6%) | 0.0155 |
| Achalasia | 1 (0.2%) | 0 (0%) | >0.9999 |
| Esophageal ulcer | 11 (2.2%) | 3 (2.2%) | >0.9999 |
| Gastric ulcera | 21 (4.3%) | 5 (3.6%) | >0.9999 |
| Foreign body | 16 (3.3%) | 8 (5.8%) | 0.2074 |
| Biliary reflux | 3 (0.6%) | 0 (0%) | 0.2658 |
| Variceal sequelae | 1 (0.2%) | 0 (0%) | >0.9999 |
| Polyps | 7 (1.4%) | 2 (1.4%) | >0.9999 |
| Nonerosive gastropathy | 46 (9.4%) | 7 (5%) | 0.1201 |
| Erosive gastropathy | 38 (7.8%) | 7 (5%) | 0.3517 |
| Duodenitis | 14 (2.9%) | 1 (0.7%) | 0.2106 |
| Nodular gastropathy | 25 (5.1%) | 2 (1.4%) | 0.0607 |
| Hemorrhagic gastropathy | 11 (2.2%) | 1 (0.7%) | 0.4798 |
| Hypertrophic folds | 2 (0.4%) | 1 (0.7%) | 0.5279 |
| Fundoplication | 2 (0.4%) | 0 (0%) | >0.9999 |
| Others | 12 (2.4%) | 8 (5.8%) | 0.0582 |
| Total | 490 | 139 | |
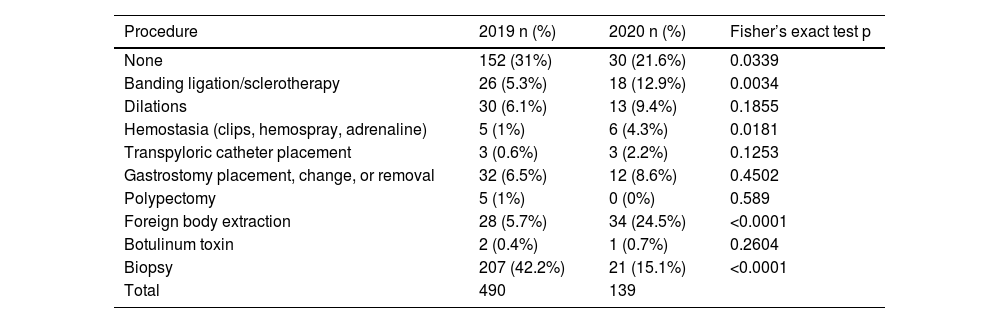
There was a significant decrease in 2020, in the number of patients in whom no procedures were performed but biopsies were taken. There was also a decrease in banding ligation/sclerotherapy, a slight increase in hemostasis, and a considerable increase in foreign body extraction in 2020, all with statistical significance (Table 4).
Type of procedure.
| Procedure | 2019 n (%) | 2020 n (%) | Fisher’s exact test p |
|---|---|---|---|
| None | 152 (31%) | 30 (21.6%) | 0.0339 |
| Banding ligation/sclerotherapy | 26 (5.3%) | 18 (12.9%) | 0.0034 |
| Dilations | 30 (6.1%) | 13 (9.4%) | 0.1855 |
| Hemostasia (clips, hemospray, adrenaline) | 5 (1%) | 6 (4.3%) | 0.0181 |
| Transpyloric catheter placement | 3 (0.6%) | 3 (2.2%) | 0.1253 |
| Gastrostomy placement, change, or removal | 32 (6.5%) | 12 (8.6%) | 0.4502 |
| Polypectomy | 5 (1%) | 0 (0%) | 0.589 |
| Foreign body extraction | 28 (5.7%) | 34 (24.5%) | <0.0001 |
| Botulinum toxin | 2 (0.4%) | 1 (0.7%) | 0.2604 |
| Biopsy | 207 (42.2%) | 21 (15.1%) | <0.0001 |
| Total | 490 | 139 |
The median number of upper endoscopies in 2020 was 9.5 procedures per month (minimum: 2, maximum: 23), which was significantly lower than the 43 procedures per month in 2019 (minimum: 12, maximum: 56) (p=0.0001 in the Mann–Whitney U test).
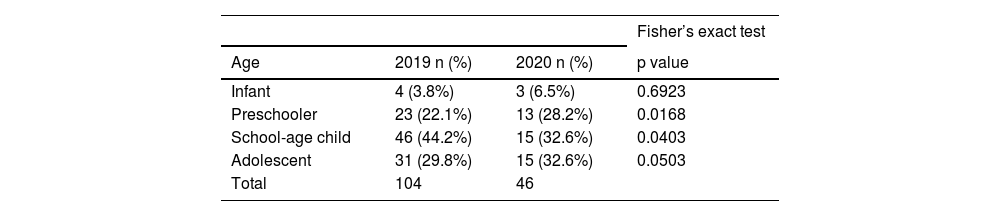
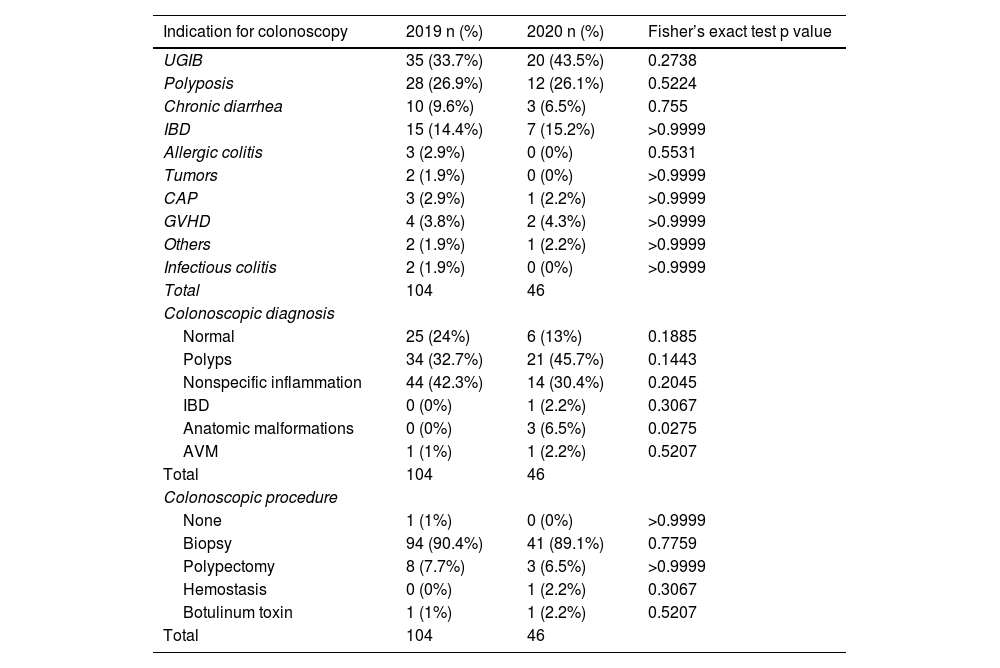
ColonoscopyIn the two years analyzed, 150 procedures were performed; 104 in 2019 and 46 in 2020, resulting in a decrease of 66%. Regarding demographic characteristics, in 2019, the procedures were carried out on 51 males and 53 females, whereas in 2020, they were carried out on 28 males and 18 females. There was no difference by sex between the two years (p=0.02160). Mean patient age was 109.61 months (58.26 SD) in 2019, whereas it was 109.20 months (64.95 SD) in 2020. The patients were divided by age group, which highlighted the fact that preschoolers were more affected in 2020, compared with school-age children, in whom there was a significant reduction. The findings are shown in Table 5.
In 2019, 76 diagnostic colonoscopies and 28 therapeutic colonoscopies were performed, whereas 29 diagnostic colonoscopies and 17 therapeutic colonoscopies were performed in 2020, signifying a decrease of 62% in the diagnostic procedures and 40% in therapeutic ones. No proportional differences were detected (p=0.2843), with diagnostic procedures always predominating.
Table 6 shows the indications, diagnoses, and procedures in colonoscopy. No statistically significant differences were detected in the comparison of the two years.
Colonoscopy indications, diagnosis, and procedure performed.
| Indication for colonoscopy | 2019 n (%) | 2020 n (%) | Fisher’s exact test p value |
|---|---|---|---|
| UGIB | 35 (33.7%) | 20 (43.5%) | 0.2738 |
| Polyposis | 28 (26.9%) | 12 (26.1%) | 0.5224 |
| Chronic diarrhea | 10 (9.6%) | 3 (6.5%) | 0.755 |
| IBD | 15 (14.4%) | 7 (15.2%) | >0.9999 |
| Allergic colitis | 3 (2.9%) | 0 (0%) | 0.5531 |
| Tumors | 2 (1.9%) | 0 (0%) | >0.9999 |
| CAP | 3 (2.9%) | 1 (2.2%) | >0.9999 |
| GVHD | 4 (3.8%) | 2 (4.3%) | >0.9999 |
| Others | 2 (1.9%) | 1 (2.2%) | >0.9999 |
| Infectious colitis | 2 (1.9%) | 0 (0%) | >0.9999 |
| Total | 104 | 46 | |
| Colonoscopic diagnosis | |||
| Normal | 25 (24%) | 6 (13%) | 0.1885 |
| Polyps | 34 (32.7%) | 21 (45.7%) | 0.1443 |
| Nonspecific inflammation | 44 (42.3%) | 14 (30.4%) | 0.2045 |
| IBD | 0 (0%) | 1 (2.2%) | 0.3067 |
| Anatomic malformations | 0 (0%) | 3 (6.5%) | 0.0275 |
| AVM | 1 (1%) | 1 (2.2%) | 0.5207 |
| Total | 104 | 46 | |
| Colonoscopic procedure | |||
| None | 1 (1%) | 0 (0%) | >0.9999 |
| Biopsy | 94 (90.4%) | 41 (89.1%) | 0.7759 |
| Polypectomy | 8 (7.7%) | 3 (6.5%) | >0.9999 |
| Hemostasis | 0 (0%) | 1 (2.2%) | 0.3067 |
| Botulinum toxin | 1 (1%) | 1 (2.2%) | 0.5207 |
| Total | 104 | 46 |
AVM: arteriovenous malformation; CAP: chronic abdominal pain; GVHD: graft-versus-host disease; IBD: inflammatory bowel disease; UGIB: upper gastrointestinal bleeding.
In 2020, only 31% (185) of the procedures were performed, compared with 594 procedures in 2019, implying a decrease of 69%. When dividing the procedures, 139 (28%) upper endoscopies were performed in 2020, compared with 490 in 2019, resulting in a 72% decrease; 104 colonoscopies were performed in 2019 and 46 (44%) in 2020, signifying a 66% decrease.
The median number of colonoscopies in 2020 of 3.5 monthly procedures (minimum: 0, maximum: 15) was significantly lower than the 10 monthly procedures in 2019 (minimum: 1, maximum 15) p=0.0199 in the Mann–Whitney U test) (Fig. 1).
DiscussionIn the medical literature, the reported impact of the pandemic on the decrease in the number of procedures is on average 80%. In our study, we found that endoscopic procedures were reduced by 69%. Urgent and emergency procedures were predominant during the pandemic, which is a protocol that has been continued by the Instituto Nacional de Pediatría, in accordance with recommendations by NASPGHAN, ESPGHAN, and the GESA.6,9–11
When comparing age at the time of endoscopy, school-age children predominated in 2019 and decreased in 2020 (p<0.05), whereas the number of preschoolers was higher in 2020 (p<0.05). This is explained by the longer time children remained at home, often unsupervised, accounting for the increase of foreign body ingestion in children. In addition, foreign body extraction is an urgent or emergency procedure, and in the 2019 and 2020 comparison, suspected foreign body was one of the most important indications in 2020 (p<0.05).
One of the differences between 2019 and 2020 is the type of procedure performed. In 2019, diagnostic endoscopy was more frequently performed, whereas in 2020, it was therapeutic endoscopy (p<0.05). Once again, this is explained by the indication to only perform urgent and emergency procedures, resulting in a decrease in diagnostic endoscopy of 86%, a figure coinciding with that reported by the ESPGHAN,11 whereas therapeutic endoscopy decreased by only 36%.
Among the main medical indications for performing upper endoscopy in 2019 were: esophageal varices (19%) (92/490), gastrointestinal bleeding (13%) (65/490), suspected foreign body (11%) (55/490), altered swallowing mechanics (8%) (41/490), gastroesophageal reflux (8%) (41/490), and esophageal stricture (7.5%) (37/490). In 2020, the main indications were: suspected foreign body (34%) (48/139), esophageal varices (14.5%) (20/139), stricture (11.5%) (16/139), UGIB (8.6%) (12/139), altered swallowing mechanics (8%) (11/139), and gastroesophageal reflux (2%) (3/139). In 2020, suspected foreign body was one of the main indications (p<0.05). Notably, variceal and nonvariceal bleeding were the indications whose numbers most commonly increased in 2020 (p<0.05), along with stricture.
Likewise, there was an important change in endoscopic findings, given that in 2019, the most common finding was varices/congestive gastropathy (26%) (107/490), followed by normal endoscopy (18.5%) (91/490), which is explained by the fact that the indications in that year were mainly diagnostic: nonerosive gastropathy (9%) (46/490), esophagitis (7.7%) (38/490), and erosive gastropathy (7.7%) (38/490), whereas in 2020, the most common findings were esophagitis (24%) (34/139), varices/congestive gastropathy (18%) (25/139), normal endoscopy (16%) (22/139), foreign body (6%) (8/139), and erosive and nonerosive gastropathy, both with (5%) (7/139). There were more abnormal (pathologic) studies than normal studies in 2020, compared with 2019 (p<0.05), again explaining the changes in endoscopy indications in the two years.
There was also an important change in the type of procedure performed. Compared with 2020, diagnostic biopsy (42%) (207/490) was the most frequent procedure in 2019, followed by no procedure (31%) (152/490), dilations (6%) (30/490), foreign body (5.7%) (28/490), and banding ligation/sclerotherapy (5.3%) (26/490). In 2020, the main procedure was foreign body extraction (24%) (34/139), followed by no procedure (21%) (30/139), biopsy (15%) (21/139), banding ligation/sclerotherapy (13%) (18/139), and dilations (9%) (13/139). There was a statistically significant decrease in the number of biopsies due to the fact that in 2020, indications for endoscopy were mainly therapeutic, and not diagnostic. Foreign body extraction (p<0.05) and banding ligation and/or variceal sclerotherapy were the most important procedures in 2020 because children were at home longer, often unsupervised, leading to a substantial increase in foreign body ingestion, whereas esophageal variceal bleeding continued being an emergency.
ColonoscopyWith respect to colonoscopy, there was a 66% decrease in the procedure in 2020; 73% of the procedures were diagnostic in 2019, dropping to 63% in 2020; therapeutic procedures increased to 37% in 2020, compared with 26% in 2019, as was expected.
The clinical indications were the same for the two years: lower gastrointestinal bleeding (33.6% in 2019 and 43.5% in 2020) and polyposis (27% in 2019 and 26% in 2020), followed by chronic diarrhea, inflammatory bowel disease, and graft-versus-host disease. Even though the proportions were different, the indications remained more or less the same. Bleeding continued to be one of the most common causes both years. No statistically significant differences were found.
In both years, regarding diagnostic colonoscopy, nonspecific inflammation predominated (42% in 2019 and 30% in 2020), followed by polyps (33% in 2019 and 47% in 2020) and normal colonoscopy (24% in 2019 and 13% in 2020). Fewer diagnostic procedures were performed in 2020, thus there were fewer normal studies reported, but those results were not statistically significant.
ConclusionsAccording to the data reported, there was an important decrease in the number of procedures performed, as well as a change in the type of procedure, with a decrease in diagnostic upper endoscopy and an increase in therapeutic endoscopy.
One of the most common causes for diagnostic and therapeutic upper endoscopies is UGIB and the presence of esophageal varices and hypertensive gastropathy. Clinical indications for colonoscopy remained the same in the two years, with lower gastrointestinal bleeding and polyps being the main causes. This highlights the importance of endoscopy services being supplied with all the new hemostatic techniques (hemospray, hemostasis clips, argon plasma, silver nitrate, etc.)
In addition, due to the lockdown, there was an increase in foreign body ingestion, especially in preschoolers, suggesting the need for reinforcing prevention measures in the home and increasing the awareness of pediatricians of the possibility of this occurrence.
Financial disclosureNo financial support was received in relation to this article.
Conflict of interestThe authors declare that there is no conflict of interest.