Presentamos el caso de una paciente de 16 años, originaria del sur del estado de Puebla, México. En sus antecedentes destaca la convivencia con mascotas caninas y la cría de ovejas por la familia de la paciente. La escasa sintomatología de la paciente hizo sospechar una lesión benigna. Los estudios practicados que incluyeron una exploración laparoscópica nos orientaron a considerar el manejo. quirúrgico para un quiste no parasitario. Ante la persistencia del dolor sordo en el hipocondrio derecho se decidió una nueva exploración esta vez a cielo abierto la cual descubrió un quiste hidatídico joven y activo, no complicado, de 6 cm de diámetro, que fue manejado quirúrgicamente con éxito, el diagnóstico definitivo fue aportado por el patólogo, el cual demostró la presencia de las 3 cubiertas características del quiste parasitario, histológicamente compatible con Echinococcus granulosus. La evolución postoperatoria fue sin incidentes, el ultrasonido de control mostró la restitución completa del parénquima hepático.
We present herein the case of a 16-year-old female from the southern portion of the State of Puebla, Mexico. When gathering her past medical history, it was revealed that she had grown up with pet dogs and that her family raised sheep. Because the patient presented with few symptoms, a benign lesion was suspected, and after laparoscopic exploration, the possibility of surgical management for a non-parasitic cyst was considered. A dull pain in the right hypochondrium persisted and open surgical exploration was performed in which a 6 cm young, active, uncomplicated hydatid cyst was discovered. Its surgical removal was successful and the pathologist provided the definitive diagnosis. The three layers characteristic of a parasitic cyst were present and it was histologically consistent with Echinococcus granulosus. Postoperative progression was unremarkable and the control ultrasound study revealed complete restitution of the hepatic parenchyma.
Introduction
The aims of this article were to present the first case in the State of Puebla, according to the Department of Epidemiology of the Mexican Health Department, of hydatid cyst (HC) and to underline its characteristics and current treatment modalities. The present case had the appearance of a simple solitary cyst, but its parasitic nature was suspected during laparotomy and direct examination. Management was surgical, due to persistent symptomatology and the size of the cyst. The present case illustrates how the possibility of parasitic disease must be considered when dealing with a voluminous cyst, even if imaging studies do not reveal enough elements for such a suspicion. During the procedure, a clear fluid was found inside the cyst that was covered by the characteristic whitish membrane.
Clinical case
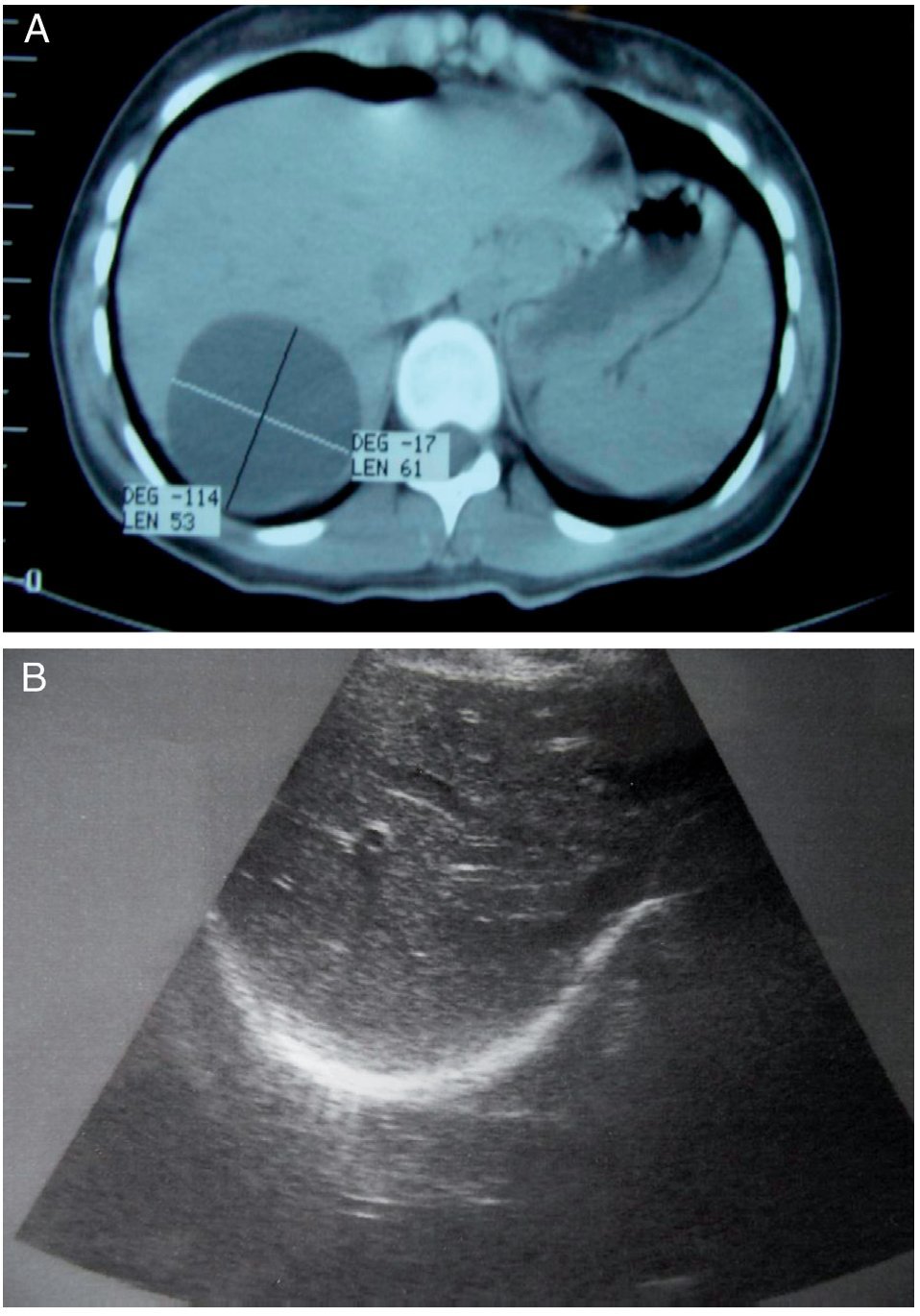
A 16-year-old female had disease onset in Januar y 2011 with mild pain in the right hypochondrium for which her attending physician ordered an ultrasound study. It revealed the presence of a rounded anechoic image of approximately 6 cm in diameter in segment VII of the Couinaud liver segment classification. Upon hospital admittance, her basic laboratory work-up (full blood count, blood chemistry, and coagulation tests) was normal. Eosinophils were reported at 0% and it was not possible to order other tests. The patient underwent laparoscopic exploration on January 27, 2011, during which the cyst could not be visualized because of its posterosuperior location. Two weeks later, with the patient experiencing an intensified dull pain that did not allow her to eat properly, another ultrasound study was ordered along with an abdominal computed axial tomography scan, correctly locating the cyst in segment VIII of the Couinaud classification (Figs. 1A-B).
Figure 1. A) Absence of septums in the interior of the simple biliary-like cyst. B) Postoperative ultrasound control showing the absence of cysts.
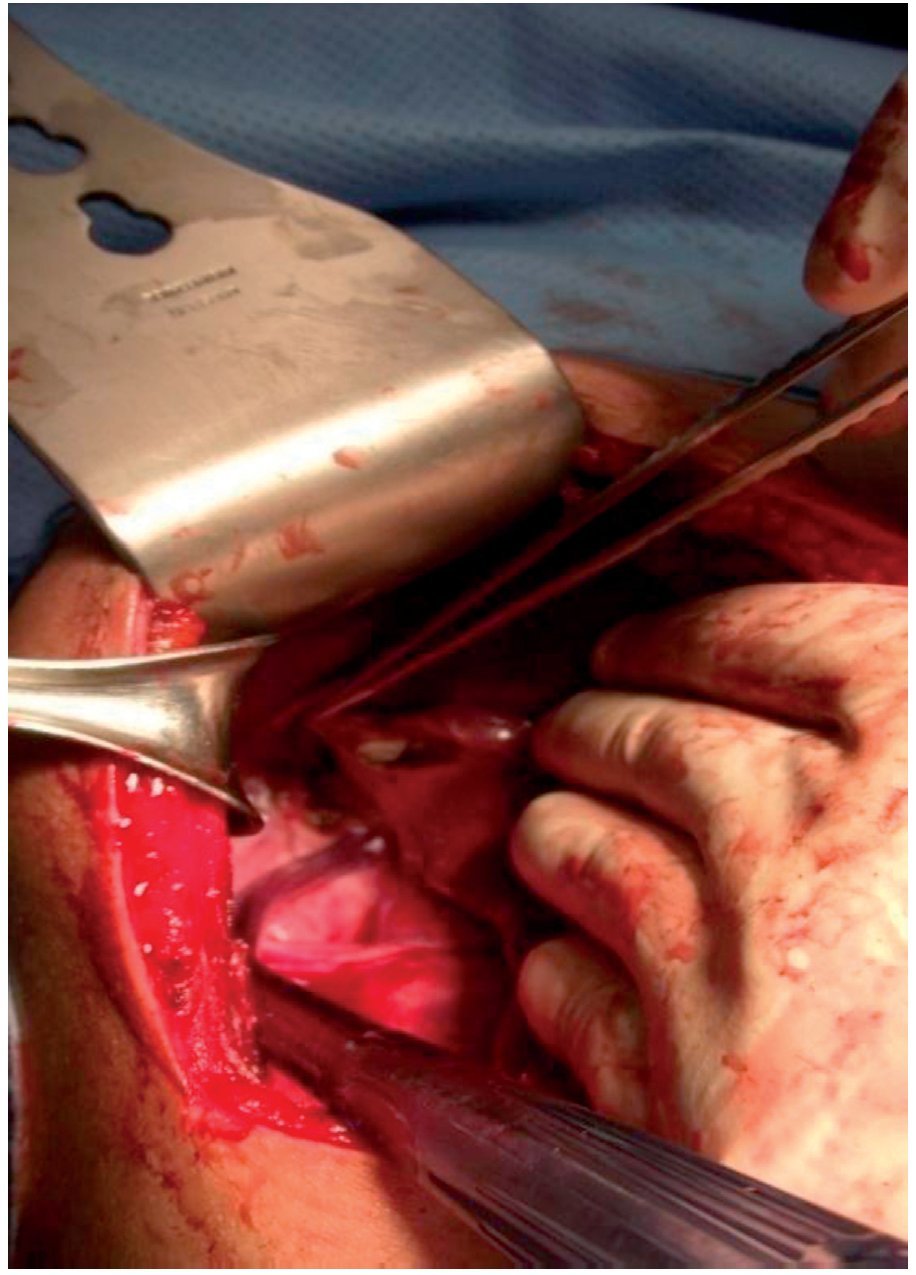
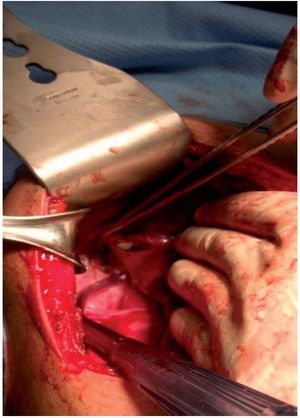
A right subcostal laparotomy was done at this precise location, to directly puncture the cyst, extracting a clear fluid that was sent to the pathologist. When the upper portion of the capsule was removed, the window created showed that the cyst was different from a simple biliary cyst of the liver because it had a second layer formed by whitish tissue (Fig. 2), completely covering the interior of the cyst. This second layer was removed in its entirety after the rest of the abdomen was isolated using surgical compresses and the cavity of the cyst was impregnated with hypertonic saline solution by means of a compress left inside it for 10 minutes. The procedure was completed with a pedicled greater omentum omentoplasty.
Figure 2. The liver reclined with the hand to the left of the patient. The whitish layer of the germinal membrane is visible.
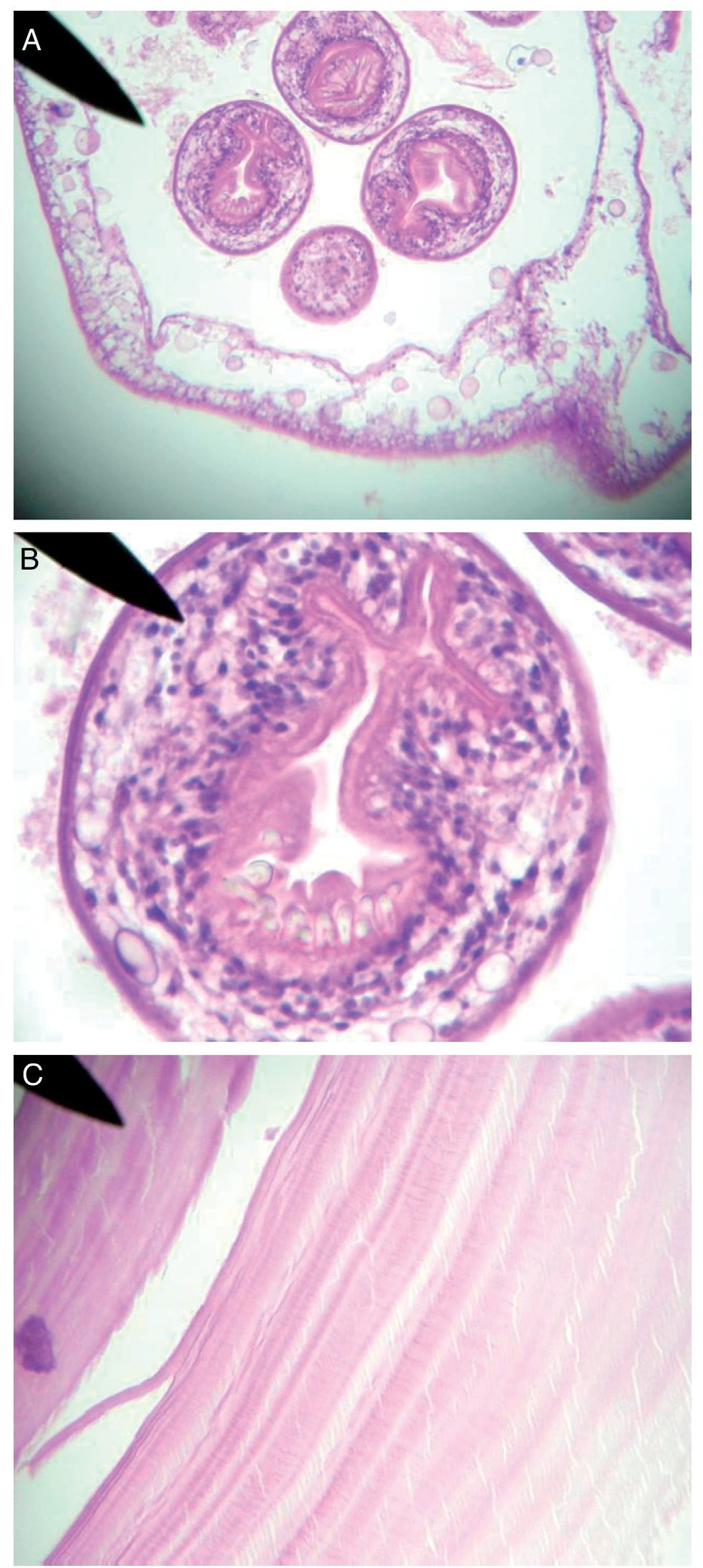
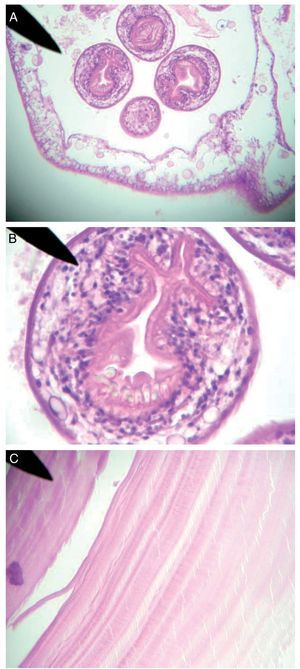
The pathology result of the fluid was negative for malignancy and had traces of proteinoid material. The surgical specimen had the aspect of a granulous layer of an Echinococcus granulosus (EG) cyst (Figs. 3 A-C).
Figure 3. A) Protoscoleces and gemmation of the granulous layer. B) Scolex of the Echinococcus granulosus with sucker and hooks. C) An anhistous layer of the cyst.
Postoperative progress was unremarkable and the patient was released 24 h after her surgery. She remained under surveillance for one year during which time she was asymptomatic. The same laboratory studies done one month later showed 0% eosinophils and all other parameters were normal.
An ultrasound study carried out 11 months after the procedure showed complete restitution of the hepatic parenchyma that had been affected by the cyst (Fig. 3B).
Discussion
Echinococcosis is a cosmopolitan zoonosis and has been reported in Europe, Australia, New Zealand, Asia, Africa, South America, and Canada. Information on it in Mexico is limited and some authors state that the disease in humans is almost non-existent.1 In the literature consulted, we found cases reported in Durango, Oaxaca, Zacatecas, Nuevo León, Guanajuato, the State of Mexico, and Mexico City.1-3
Humans are the accidental hosts3 and acquire primary cystic hydatidosis through the ingestion of eggs excreted by infested carnivores. The cyst can measure from one to 15 cm or more, and grows at a rate of 1 cm/year.3 The fluid it contains is generally clear and protoscoleces produced by gemmation are found in the germinal layer. Clinically, the hepatic cyst may remain asymptomatic for years and symptoms depend on its location in the liver. Pain in the right hypochondrium is constant and can radiate to the shoulder and be accompanied by abdominal distension, cholestasis, portal hypertension, biliary cirrhosis, and/ or ascites. Symptoms should not be waited for, before suspecting the parasitic nature of a cyst. The characteristic images have been described4 and the Casoni or Montenegro skin tests are useful, as are the ELISA IgG antibodies against echinococcus, with a sensitivity of 94% and a specificity of 99%.3,4
Treatment for symptomatic hydatid cysts larger than 5 cm is surgical and is the accepted criterion for the majority of authors and liver surgeons. Less aggressive treatment is given to cysts under this size.4 Medical treatment is based on albendazole and is recommended for small asymptomatic cysts. The ideal surgical treatment is hepatic resection enabling the complete elimination of this pathology. However, this modality can only be offered on limited occasions depending on the location of the cysts, and its performance is even less frequent when attempted laparoscopically.1,3,4 The majority of times, surgery includes the extraction of the fluid in the cyst through puncture. Sterilization is carried out using different solutions such as formalin, hypertonic dextrose, or hypertonic saline solution,4 which is done through fenestration, removing the most prominent portion of the wall in order to carry out complete membrane extraction. In cases in which new vesicles have grown outwards, towards the hepatic parenchyma, extirpation of the adventitious layer is recommended, with the risk for important hemorrhage (pericystectomy).4,5 In a case series by Nari, 25 patients were treated, 7 surgical techniques were employed, and there was one death.6
Laparoscopic surgical treatment is feasible once the location of the cyst and its size have been correctly studied.4,5 This procedure is contraindicated if the cyst is in a posterior position.6,7 There are recent reports on laparoscopic hepatic resection with the use of intraoperative ultrasound, Harmonic scalpel or LigaSureTM, and cyst morcellation for facilitating its extraction.6-8
Some authors, especially in South America, manage cysts that are smaller than 5 cm through percutaneous puncture, evacuation, and sterilization of the cyst. This procedure has a risk for protoscolex dissemination by means of the needle.
Preoperative medical treatment with albendazole or mebendazole is recommended in all cases for the purpose of eliminating the parasite at the level of the intestine and other organs.
The preventive measures of hygiene are well known and contact with mammalian intermediate hosts should be avoided.4 Some detection efforts have been made using portable ultrasound and immunoelectrotransfer blot tests in endemic regions of Peru with good results.9 Treatment with praziquantel is obligatory for pets in the family environment.4 A vaccine for cattle susceptible to the EG parasite is currently available in Argentina.
Conclusions
Surgical exploration is recommended in patients that live in an environment in which there is close contact with animals and who present with a cyst larger than 5 cm with no typical imaging studies or suspicious laboratory work-up. When the cyst is opened, a whitish membrane is suggestive of parasite diagnosis and the abovementioned procedures should be carried out.
Received 23 May 2012;
accepted 17 October 2012
* Corresponding author at:
Calle Venustiano Carranza núm. 115-2, Col. Puebla Textil, C.P. 72470, Puebla, Puebla.
Tel.: 2+226214543.
E-mail address: juangorea75@yahoo.com.mx (J.G. Orea-Martínez).