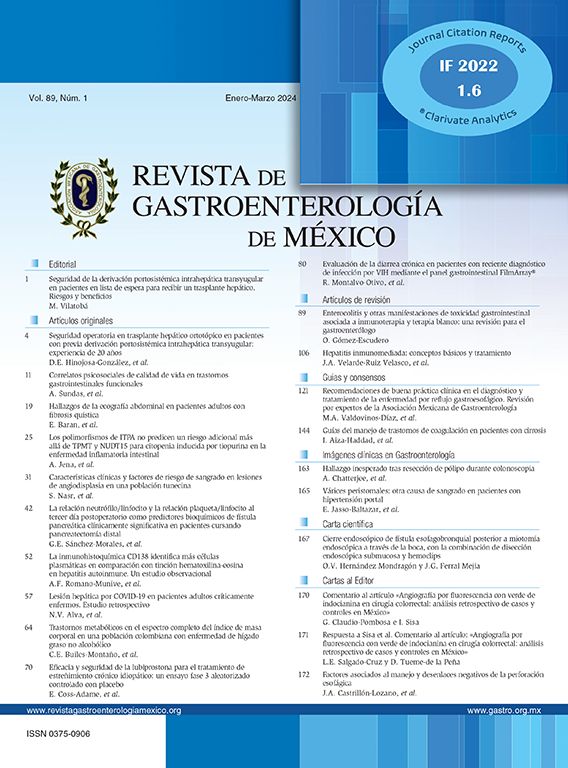
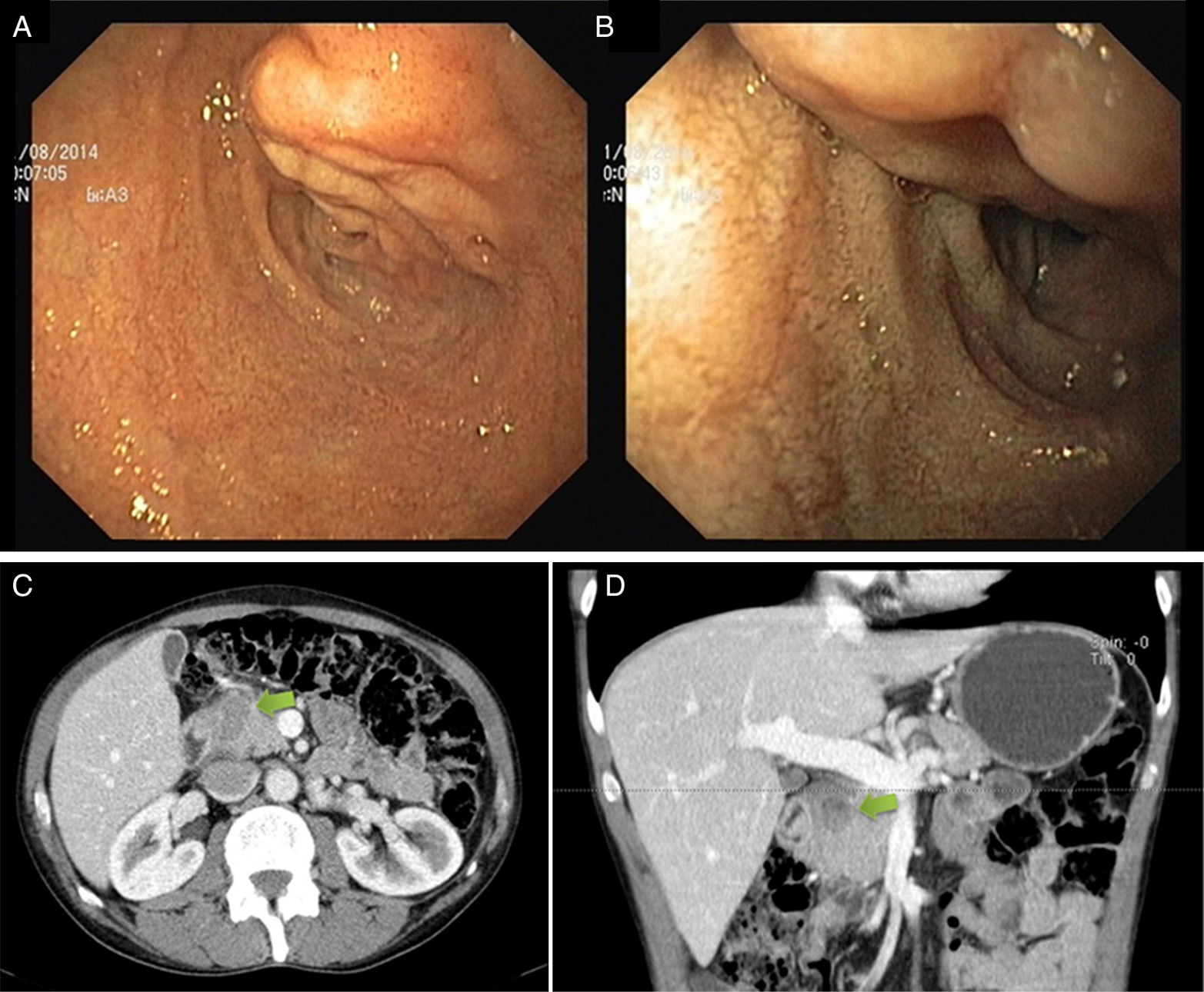
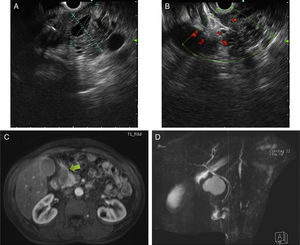
A 54-year-old man with a history of heavy alcohol consumption, muscle wasting, and recent hospitalization due to acute alcoholic pancreatitis, presented at the emergency room with epigastric pain and vomiting. Clinical examination and laboratory tests were normal. An upper endoscopy was performed that revealed a 30-mm tubular lesion at the upper edge of the duodenal bulb, covered with normal mucosa, suggestive of a vascular lesion (fig. 1A and B). A computed tomography scan identified a predominantly solid and heterogeneous mass, between the duodenum and pancreatic head, measuring 40 x 15mm, with indefinite borders, that had no contrast enhancement (fig. 1C and D). Endoscopic ultrasound confirmed the extra-pancreatic location. The color Doppler ultrasound exam was negative for vascular flow, but no other information was obtained (fig. 2A and B). Two weeks later, a magnetic resonance imaging scan described a spontaneous, hyperintense lesion on T1 and T2 in the proximity of the gastroduodenal artery that showed no enhancement after gadolinium administration (figs. 2C and D). The imaging features were suggestive of a thrombosed pseudoaneurysm of the gastroduodenal artery. The patient refused clinical follow-up and continued with heavy alcohol consumption.
A and B) Endoscopic ultrasound defined a largely hypoechoic lesion, with some anechoic areas and poorly defined limits. Color Doppler ultrasound was negative for vascular flow. C and D) The magnetic resonance imaging scan shows a spontaneous hyperintense lesion on T1 and T2 in the proximity of the gastroduodenal artery, with no enhancement after gadolinium administration. No communication with the common bile duct or pancreatic duct was observed.
Aneurysms of the visceral arteries occur in up to 5% of patients with acute or chronic pancreatitis (gastroduodenal: 10-15%) and are associated with a mortality rate of 25 to 50%.1,2
Two types of aneurysms have been described: true aneurysms, which develop when the inflammatory process causes the partial digestion of the arterial wall, and pseudoaneurysms, when pancreatic enzymes from a pseudocyst erode into an adjacent artery leading to bleeding (our case).
The most common clinical presentation is gastrointestinal bleeding secondary to rupture (52%), followed by abdominal pain (46%). The mortality rate in the setting of rupture is about 40% and according to the medical literature, spontaneous thrombosis is one of the most infrequent forms of clinical presentation of gastroduodenal artery pseudoaneurysm.3–5 The gold standard for diagnosis continues to be visceral angiography. The use of alternative methods with good sensitivity, such as computed tomography, magnetic resonance imaging, and endoscopic ultrasound, has already been reported.3
Spontaneous thrombosis is an unpredictable event and was previously reported in association with factors that decrease blood flow and increase coagulation, such as hypotension, dehydration, vasospasm, local damage to the arterial wall, and occult malignancies.4–7 However, given the high mortality rate, physicians should not wait for this to occur. Endovascular repair with coil embolization or stent placement is currently the first line of treatment. Surgery is reserved for patients with failed endovascular repair or that present with hemodynamic instability.3,8–10
Ethical responsibilitiesProtection of persons and animalsThe authors declare that no experiments were performed on humans or animals for this study.
Data confidentialityThe authors declare that they have followed the protocols of their work center in relation to the publication of patient data.
Right to privacy and informed consentThe authors have obtained the informed consent of the patients and/or subjects referred to in the article. This document is in the possession of the corresponding author.
Conflict of interestThe authors declare that there is no conflict of interest.
Please cite this article as: Gião Antunes A, Peixe B, Guerreiro H. Trombosis espontánea de un seudoaneurisma de la arteria gastroduodenal manifestado como una lesión subepitelial. Revista de Gastroenterología de México. 2018;83:354–356.