¿ Introduction
Obesity is a common chronic medical condition of diverse etiology that leads to considerable morbidity and mortality and is now considered a major health problem with a notorious increased incidence.1-3 Treatment options for obesity are multiple and include diet, behavioral therapy, medications or invasive therapy which may be further subdivided in surgical and non-surgical.1 The intragastric balloon (IGB) is used as an invasive non-surgical procedure for the treatment of obese patients. Possible complications related to intragastric balloon therapy include but are not limited to insufficient or null weight loss, gastric discomfort, epigastric pain, nausea, vomiting, esophageal or intestinal obstruction and direct injury to the digestive tract wall causing erosion with bleeding or that may even lead to perforation with abdominal sepsis.4 Management of gastric perforation requires prompt surgical intervention and the use of wide-spectrum antibiotics.4 Once the diagnosis of gastric perforation is established, immediate surgical treatment is mandatory to avoid further complications and even fatality. Herein we report the case of a 54 year old obese female who underwent placement of IGB elsewhere and later developed a ruptured anterior cerebral artery aneurysm with subarachnoid hemorrhage and a large gastric perforation with abdominal sepsis. Early diagnosis of both IGB related complications lead to prompt surgical treatment and a successful outcome.
¿ Case report
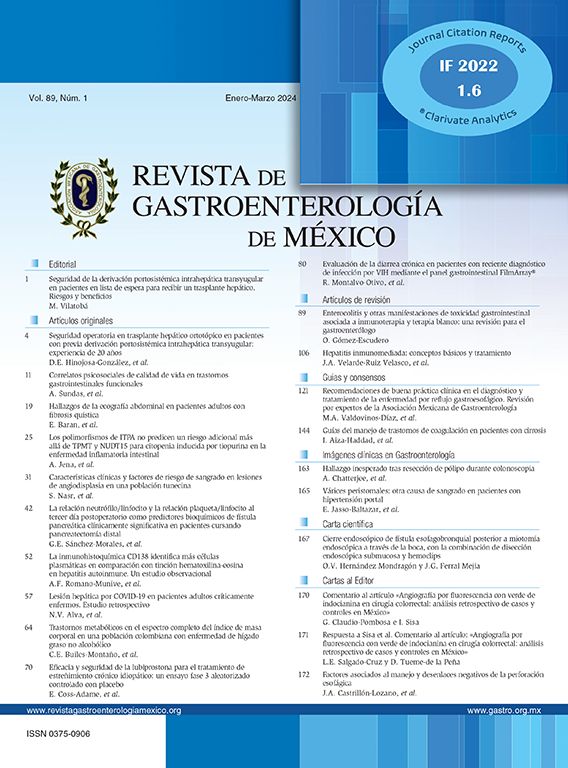
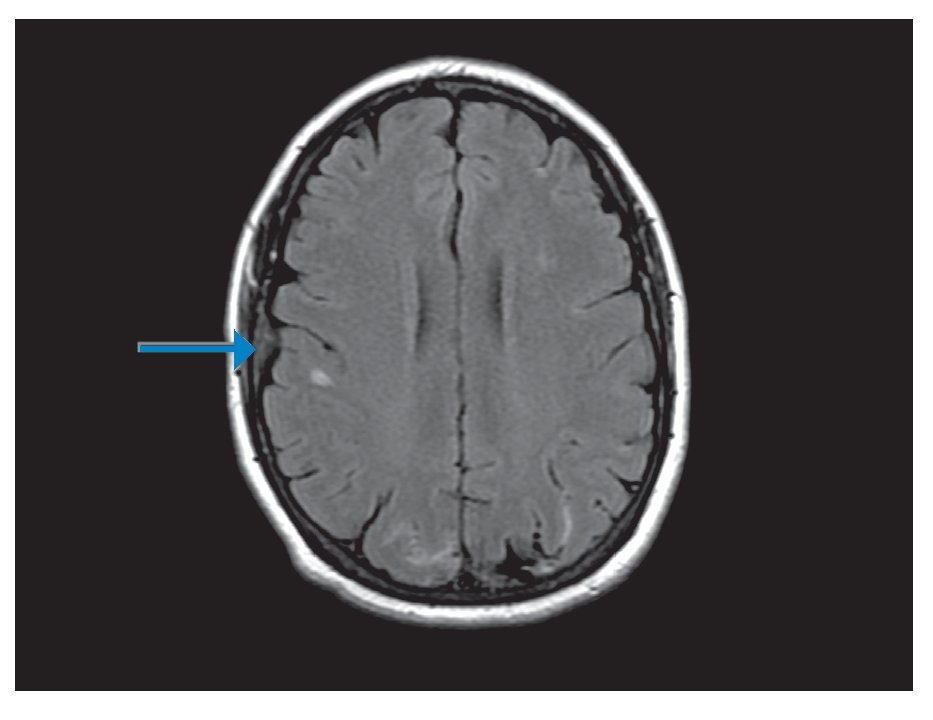
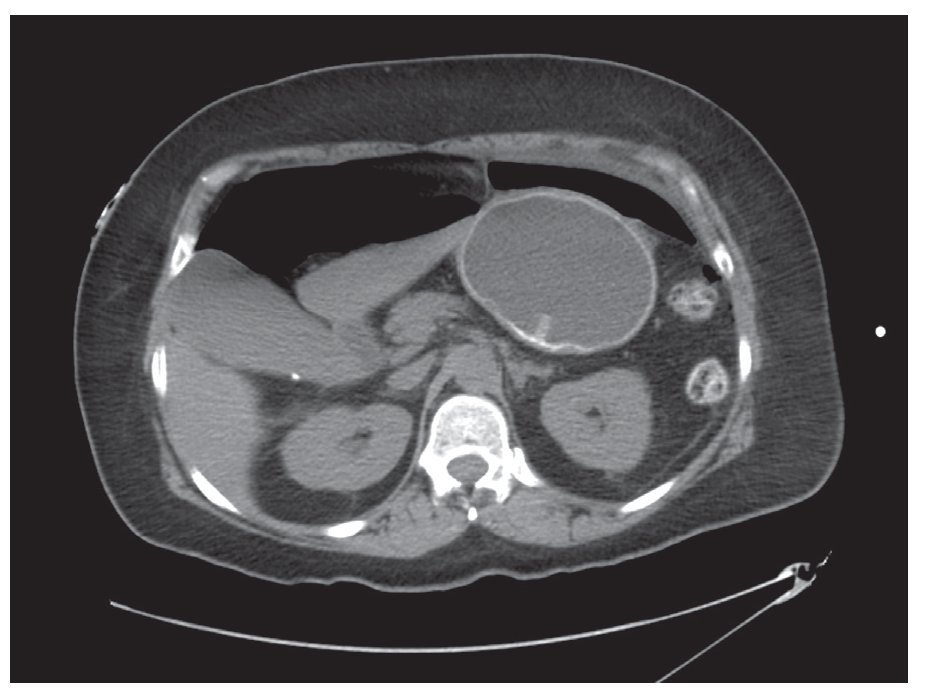
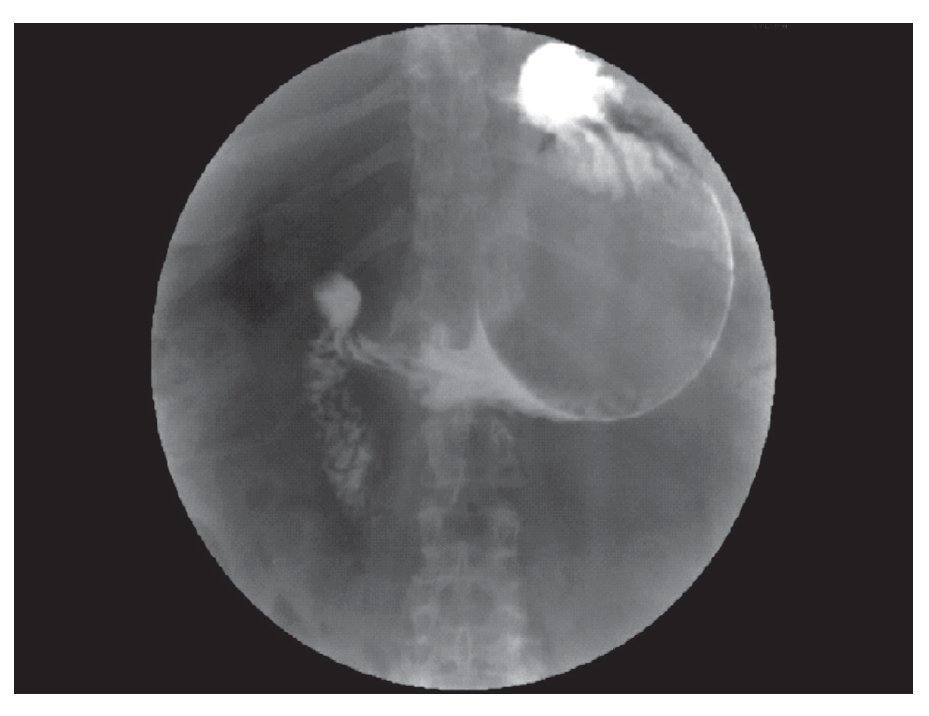
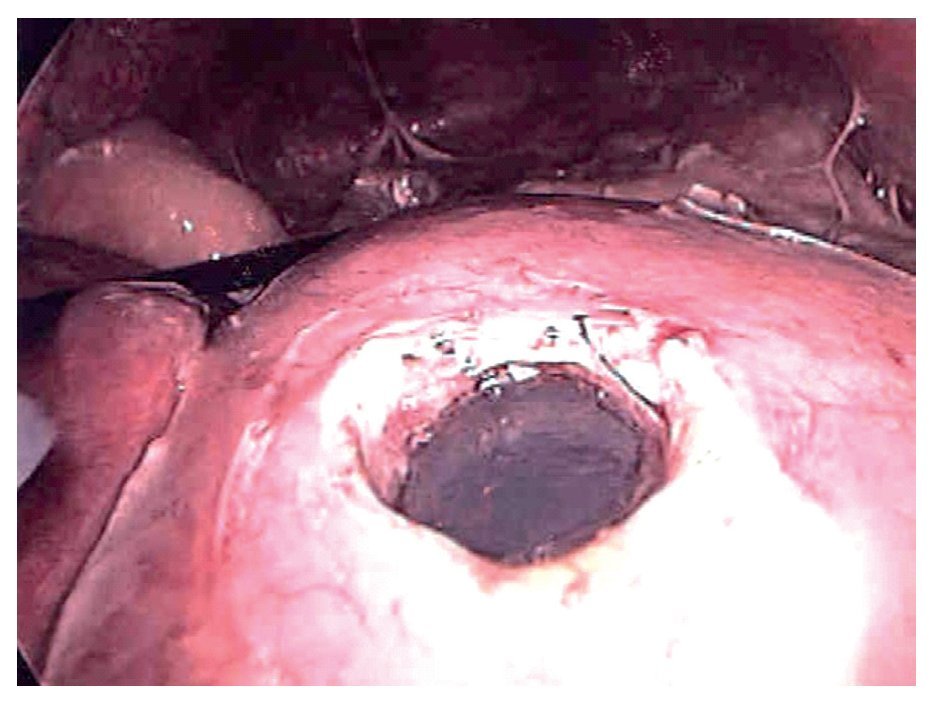
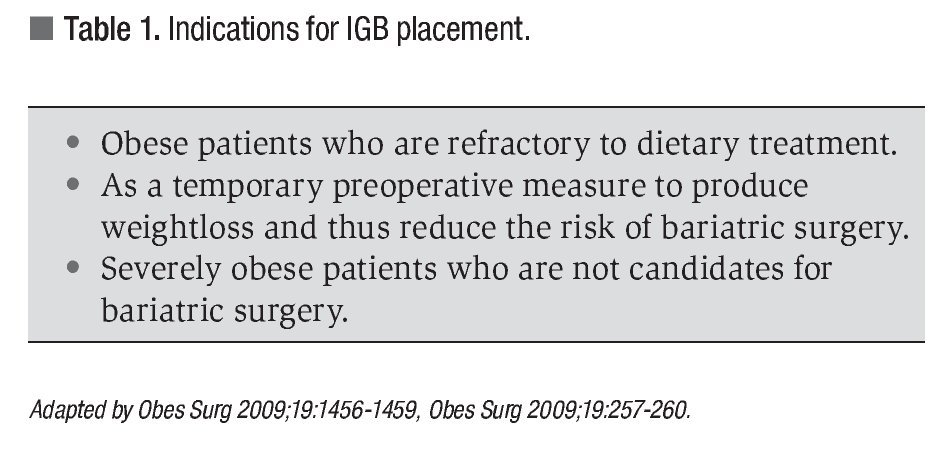
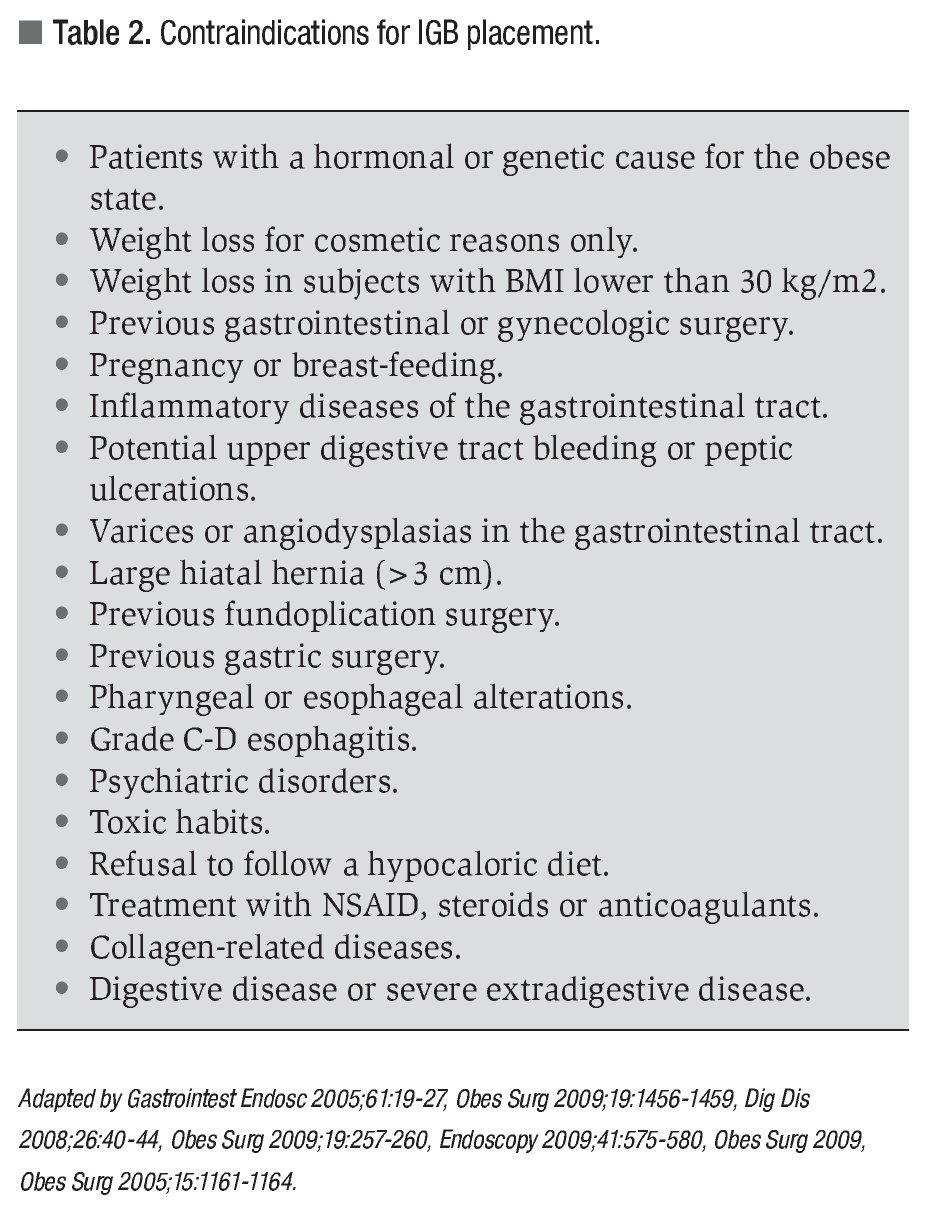
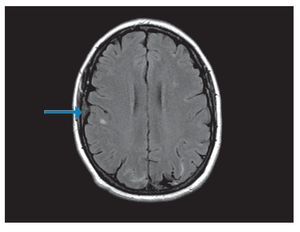
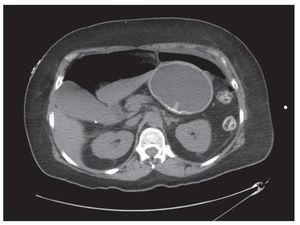
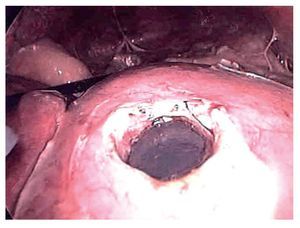
A 54 years old woman with obesity with a body mass index (BMI) of 31.2 was seen by a Gastroenterologist for endoscopic placement of an intragastric balloon (IGB) for weight loss. The patient had a history of well-controlled hypertension and a 15 year history of smoking. She had no history of a known cerebral aneurysm, chronic headaches, use of medications for weight loss, nor a history for familial cranial hemorrhage. By report, the device placement was uneventful, but the same day the patient developed nausea, vomiting and abdominal pain. The pain was persistent and located in the epigastrium. Vomiting was present although the patient was in liquid diet. The patient made strong efforts during vomiting episodes and was traduced in high blood pressure measurements. Four days after the IGB placement, the patient presented to the emergency room (ER) with a severe headache associated to loss of strength and sensation on the lower extremities. The headache had an acute onset of presentation and was after an intense vomiting episode. A cranial-spinal MRI showed findings consistent with a ruptured anterior cerebral artery aneurysm and a subarachnoid hemorrhage (Figure 1). The patient was seen by the Neurosurgery department and an aneurysm clipping was performed without further complications. The patient was discharged from the hospital 5 days after the surgery with tolerance to liquid diet and the use of non-steroideal anti-inflammatory drugs. After hospital discharge, the patient had persistent nausea and vomiting during two weeks and she returned to the emergency room. In addition to these symptoms, the patient presented with somnolence and oliguria. The patient was diagnosed with severe dehydration and acute tubular necrosis. She was transferred to the intensive care unit where she received aggressive fluid replacement and was started on a dopamine drip. Her mental status normalized, but two days after the hospitalization she began complaining of intense abdominal pain and chills. On physical examination, the patient had abdominal diffuse tenderness, hyperestesia and hyperbaralgesia. An abdominal CT showed abundant amount of peritoneal fluid and free intraperitoneal air (Figure 2). A mixture of sodium amidotrizoate and meglumine amidotrizoate in a proportion of 10:66 (Gastrografin®) for an upper gastrointestinal swallow study was performed, but it was not possible to identify a site of perforation (Figure 3). Under the suspicion of gastric perforation secondary to intragastric balloon, wide-spectrum antibiotics were started and the patient was immediately taken to the operating room where a laparoscopic exploration was performed. During surgery, an anterior perforation at the body of the stomach was identified as well as abundant purulent peritoneal liquid (Figure 4). The balloon was deflated by punction and pulled-out of the stomach through the site of perforation. Closure of the perforation was made with a linear laparoscopic stapler and reinforced with continuous non-absorbable suture. An extensive abdominal lavage was done. The patient was transferred to the ICU due to a significant systemic inflammatory response and septic shock. Although the patient required fluid supplementation postoperatively, the patient remained stable, was extubated on postoperative day 4 and further hospital course was uneventful. The patient was discharged from the hospital two weeks after the operation ambulatory and tolerating a general diet. At a 6-month follow up the patient is asymptomatic and without neurologic deficits or gastrointestinal symptoms.
¿ Figura 1. Brain MRI showing right subarachnoid hemorrhage (arrow).
¿ Figura 2. Abdominal CT scan showing extraluminal peritoneal air due to gastric perforation. Notice the intragastric balloon device.
¿ Figura 3. Water-soluble swallow. This study was not capable to show the gastric perforation.
¿ Figura 4. Laparoscopic view of the gastric perforation. Note the intragastric balloon device still inflated.
¿ Discussion
Obesity is a disease that is associated with considerable morbidity and mortality. Treatment of patients with obesity should focus on a sustained 10% to 15% weight loss to reduce cardiovascular and other obesity-related diseases.2,5 In morbid obesity, defined a body mass index (BMI) of >35 kg/m2, a sustained weight loss of 20% - 25% is required. The initial approach should consist of a combination of energy-restricted diet, physical activity and behavior modification.5 A surgical approach is restricted to extremely obese2 patients with a BMI >40 kg/m2 or those with a BMI of >35 kg/m2 who present complications of obesity such as diabetes mellitus, hypercholesterolemia, sleep apnea, arthralgias, etc.
The IGB was first used in 1982.4,6-9 It is a mechanical device formed by a silicone wrapper inserted endoscopically in the stomach, filled with 500 cm3 of saline solution and 10 mL of methylene blue. The device is expanded into a spherical shape.1,3,7 The filled balloon acts as an artificial bezoar by partially filling the stomach and inducing a feeling of satiety.7 Additionally, the intragastric balloon is thought to help individuals to modify their eating habits by providing a self-education tool.8
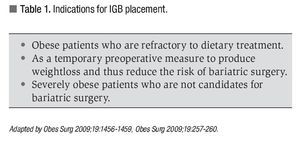
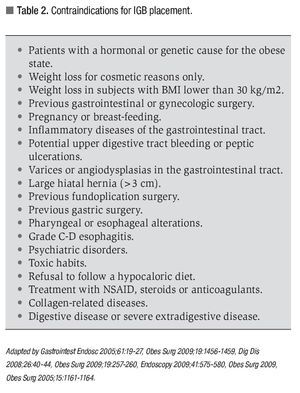
Indications and contraindications are specified in Table 1 and Table 2 respectively. Treatment with intragastric balloon is recommended for six months. However, some studies report one year results with substantial weight loss, and the majority of patients maintained this weight loss during the balloon-free second year.2 In the study of Dastis and collaborators, a weight loss 310% of weight at baseline and sustained at 2.5 years was achieved in 24% of participants.9 In one study including 119 patients treated with the IGB device, there was improvement of obesity- related illnesses with decrease in levels of fasting glucose, cholesterol, triglyceride, C-reactive protein, and blood pressure. The authors reported no serious complication related to IGB.10
The most common side effects after the placement of this device are nausea (71%), vomiting (27%), and epigastric pain (23%).8 These symptoms are to be expected for 72 hours and require treatment with antiemetic, antispasmodics, analgesics, and acid suppressants.5 Is necessary to instruct the patient to have a liquid diet for a 72-hour after the insertion of the device to minimize these side effects.5 These symptoms were present in our patient shortly after the placement of the IGB. The subarachnoid hemorrhage that our patient experienced was probably secondary to the combination of an undiagnosed aneurysm and the high intracranial pressure experienced during the vomiting episodes. Added to these factors, the patient had history of high blood pressure and smoking which could be related with the development of the cranial hemorrhage. We believe that the aneurysm rupture occurred after an episode of intense vomiting that caused an increase in blood pressure and the intracranial pressure.
Other side effects that have been reported after placement of an IGB include hypokalemia, functional renal insufficiency, abdominal pain, bloating, gastroesophageal reflux, a feeling of heaviness in the abdomen, back pain.1,3 Injure the digestive tract during device placement or removal,1 esophageal or intestinal obstruction due to a balloon deflation and migration to the esophagus or small bowel, insufficient or null weight loss, gastric discomfort, epigastric pain,4,5,7,8 and mild acute pancreatitis.9 In a large study including 2 515 patients in whom the IGB was placed, the rate of complications was 2.8%, and gastric perforation occurred in 5 patients (0.19%). Four of these patients had previous gastric surgery.11
Gastric perforation is a serious complication that can lead to sepsis and death if not diagnosed and treated early. This complication occurs in 0.2% to 4.7% and mortality rates range from 0.1% to 4.7%.4,5 Gastric perforation can occur as early as 2 days after the intragastric balloon placement,3 one month after its placement, or during its removal 8 months after placement.1 The origin of gastric perforation is believed to be secondary to formation of gastric ulcers due to intragastric balloon leading to the gastric wall irritation and lack of cytoprotection secondary to prostaglandin production of the gastric mucosa.3,7 It is strongly postulated that food impaction between the balloon and the gastric wall or the irregular and rigid surface of the filling valve could increase gastric wall pressure, creating a weakened zone in the gastric wall and eventually promoting a perforation.3 Sudden abdominal pain after intragastric balloon deployment, even several weeks or months later, should raise the suspicion of gastric perforation.3 Wide-spectrum antibiotics are mandatory together with surgical treatment for gastric perforation. Surgery should be tailored in each case according to the site of perforation, the type and extension of the lesion, the degree of peritoneal contamination, the patient´s age, and associated diseases.4 The gastric perforation was the second complication in our patient, and a clinical picture of septic shock and acute abdomen were present at the moment of the diagnosis. It´s possible that the persistent vomiting, the acute stress for the cranial hemorrhage and surgery, added to the use of non-steroideal anti-inflammatory drugs could contribute to the gastric perforation. Adverse effects due to IGB device implantation occur frequently, although serious complications are less common. We described first the association between a ruptured aneurysm of the anterior cerebral artery and subsequently a gastric perforation with secondary septic shock in the same patient during the first two months after placement of the IGB device. The rupture of an intracranial aneurysm must be included as a complication of the IGB.
¿ Conclusion
Patients with IGB should be followed closely in order to promptly detect serious complications that can present as a result of the placement of this device. Physicians should carefully weigh the risks, benefits, and long term results of this procedure and discuss them with patients before its widespread use in the treatment of patients with obesity.
Correspondence author: Manuel Muñoz-Juárez M.D.
Carlos Graef Fernández 154-515, Col. Tlaxala, CP 05300, México D. F.
Telephone/Fax: (5255) 1664 7164.
E-mail: munozmd@prodigy.net.mx.
Received August 26th, 2010;
accepted December 7th, 2011.