Chronic pancreatitis is a benign and irreversible inflammatory disorder characterized by the conversion of pancreatic parenchyma into fibrous tissue.1,2 Initial management should be conservative and surgery should be applied if there is medical treatment failure.1,3,4 Among the surgical procedures are distal pancreatectomy, pancreaticoduodenectomy, duodenum-sparing pancreatic head resection, local resection of the pancreatic head with longitudinal pancreaticojejunostomy, the Berne procedure, and the Hamburg procedure. Drainage procedures are the Puestow procedure and its modification (Partington and Rochelle).1 The development of minimally invasive techniques has made the laparoscopic performance of these technically very difficult procedures possible. Our aim was to report the initial experience at our hospital in the management of chronic pancreatitis through the laparoscopic Puestow technique.
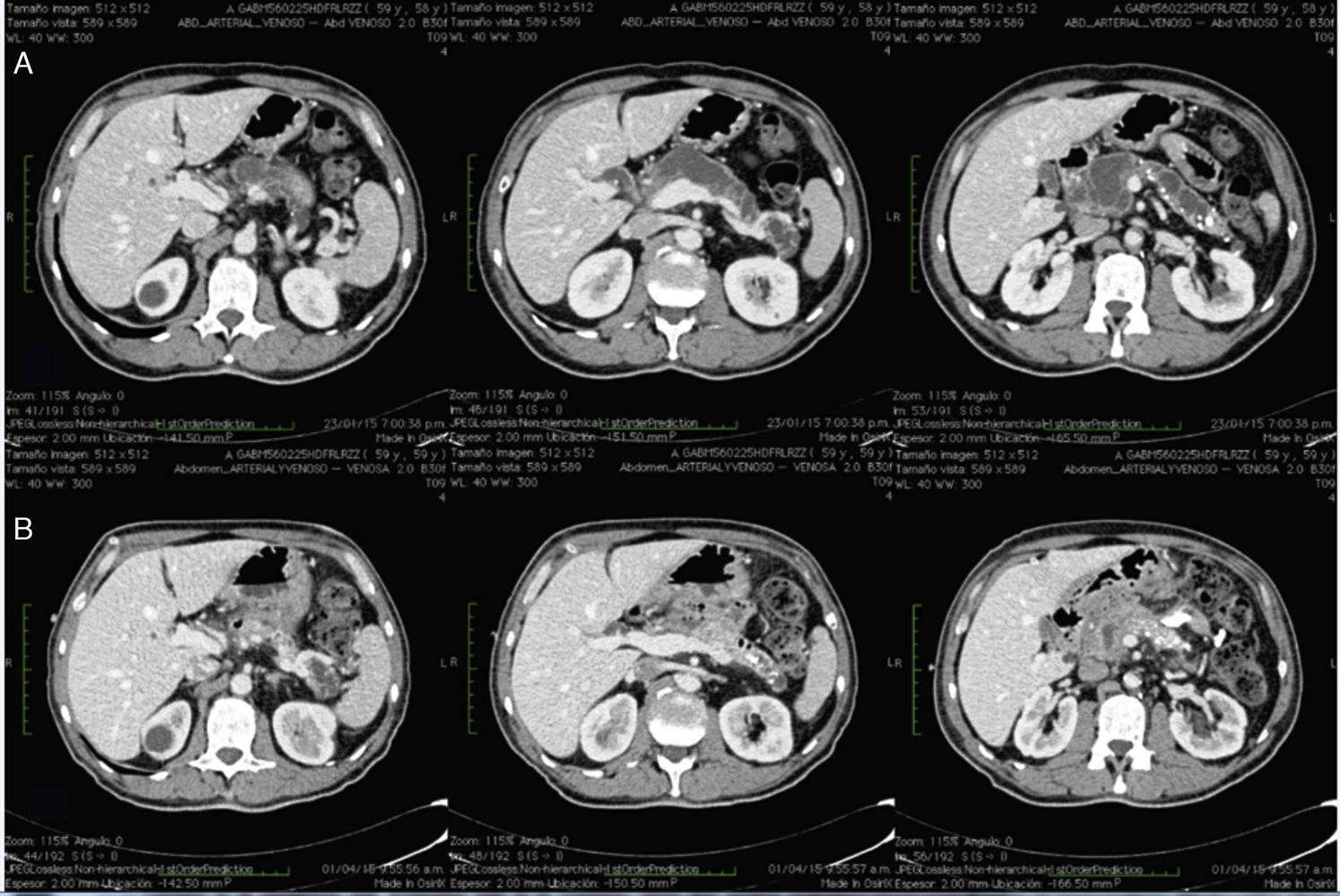
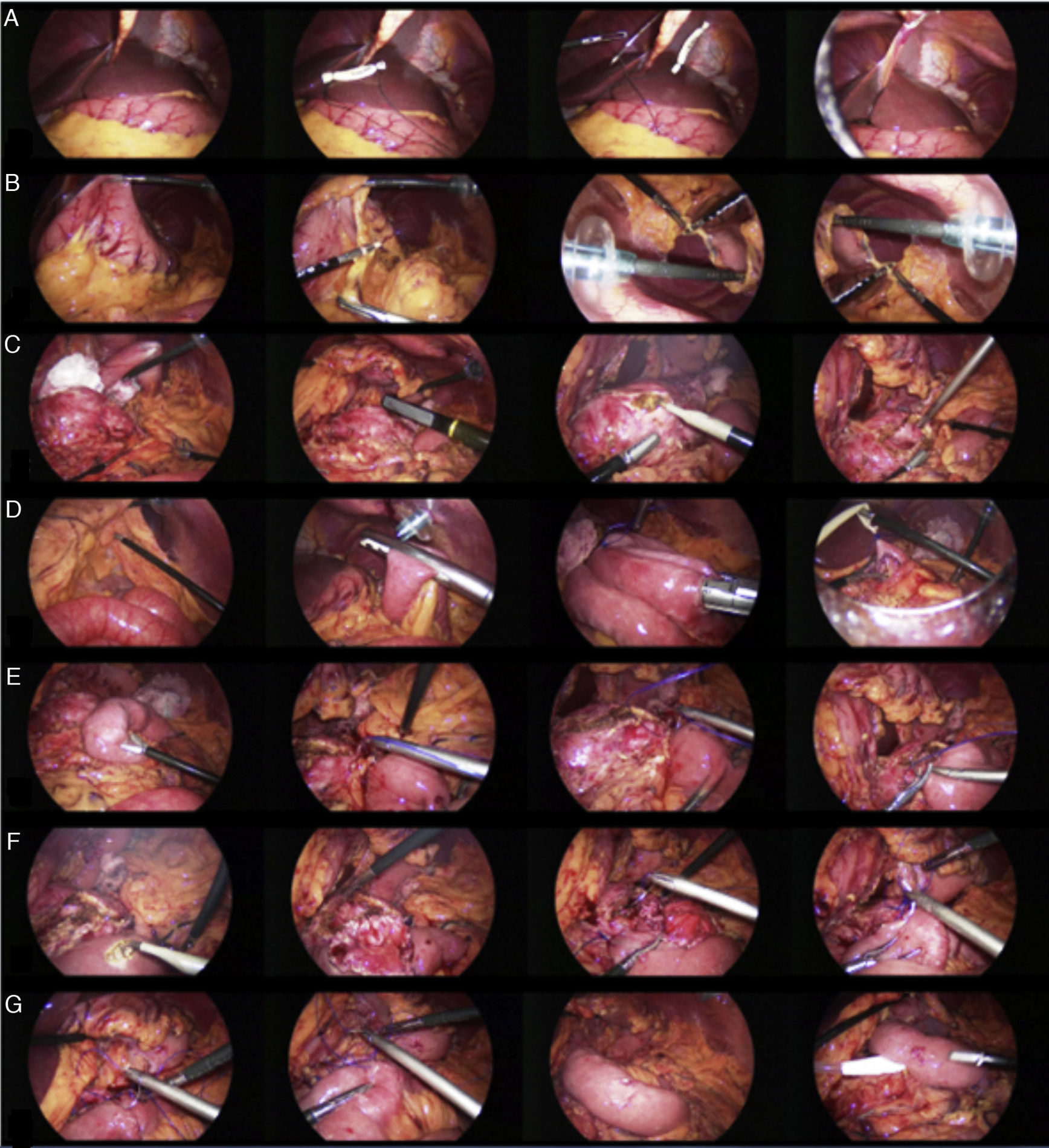
A 59-year-old man had a past history of chronic alcoholism since he was 19 years old. At the end of 2013 he presented with exacerbations of intermittent epigastric pain and unmeasured weight loss. He underwent medical treatment with opioids for 2 years. Computed tomography scan revealed a heterogeneous pancreas, calcifications, and a main pancreatic duct of 16-19mm (fig. 1A). Surgical management was decided upon. We performed the procedure under balanced general anesthesia. The Veress needle was used to create the pneumoperitoneum with a pressure of 14mmHg and the approach included a supraumbilical 12mm optical port, 4 working ports of 5 and 12mm, 2 of which were placed at the midclavicular line in the right and left subcostal area and 2 at the anterior axillary line in the right and left flank. The pancreas was exposed through the sectioning of the gastrocolic ligament with a Harmonic Ace® scalpel (Ethicon Endo-Surgery Inc., Ohio, USA), with cephalad retraction of the stomach, opening of and entering into the lesser sac cavity, (figs. 2A and B). The ventral surface of the pancreas was exposed from the neck, the laparoscopic ultrasound device was introduced, and the intraoperative study was carried out, identifying a dilated main pancreatic duct (1.6cm) (fig. 2C). An incision was made in the body of the pancreas with a monopolar hook. The lumen of the main pancreatic duct was found and the incision was extended longitudinally from the neck to the tail of the pancreas (10cm) (fig. 2C). The Roux-en-Y loop was prepared 75cm from the ligament of Treitz and the jejunum was sectioned with a 60mm Endo-GIATM stapler (Covidien, Minnesota, USA). Transmesocolic retrocolic conduction of the Roux loop was carried out, closing the open cut in the mesocolon with 3-0 MonocrylTM suture (Ethicon Endo-Surgery Inc., Ohio, USA). A jejunojejunal anastomosis at 60cm was performed with an Endo-GIATM stapler (Covidien, Minnesota, USA) and the enterotomy was closed with 2-0 polypropylene intracorporeal suture (fig. 2D). A jejunal isoperistaltic loop (Roux) was longitudinally placed at the opening of the main pancreatic duct, and monopolar enterotomy was performed in the antimesenteric segment. Intracorporeal pancreaticojejunal anastomosis was carried out through an inferior and a superior plane, with a total thickness simple stitch using a 2-0 polypropylene suture (figs. 2E and F). Two closed drains were placed at each anastomosis (fig. 2G).
A) Exposure with retraction of the round ligament with a Penrose drain. B) Dissection by way of the gastrocolic ligament to approach the lesser sac. C) Identification of the pancreatic duct with laparoscopic ultrasound and the opening of the duct. D) Roux-en-Y formation. E) Placement of the isoperistaltic Roux loop. F) Enterotomy and formation of the pancreaticojejunal anastomosis. G) Completion of the pancreaticojejunal anastomosis and placement of the closed drain.
The operation was completed laparoscopically with no incidents. Surgery duration was 300min and the estimated blood loss was 100ml. There were no postoperative complications. The patient was released 4 days after surgery. At the follow-up at week 4, the patient had abdominal pain relief, tolerated oral diet, had no significant changes in his weight, no gastrointestinal symptomatology, and was not using analgesics. The control tomography scan at one month revealed pancreaticojejunal anastomosis viability and resolution of the dilation of the entire main pancreatic duct (fig. 1B).
The ideal surgical approach for chronic pancreatitis should be designed for the long-term effective relief of pain, preserving pancreatic function, and with minimum surgical morbidity and mortality.5
In 1958 Puestow and Gillesby described ductal drainage through longitudinal anastomosis, with resection of the tail of the pancreas and splenectomy. In 1960 Partington and Rochelle modified that technique, eliminating splenectomy and distal pancreatectomy. This modification (the modified Puestow) is the currently performed technique and is indicated in those patients with a dilated duct (> 7-8mm). It achieves initial pain relief in 66-93% of the patients, 50% of the patients have recurrent symptoms in the long term, and relief is not achieved in 10-35%.5
Kurian and Gagner performed the first laparoscopic Puestow procedure in 1999, establishing the safety of carrying it out laparoscopically.6
In a case series of 17 patients, laparoscopic lateral pancreaticojejunostomy was performed, concluding that the essential element was training and skill in relation to intracorporeal sutures and knots.7
The second case series with more patients (n=12) reported that the most important aspect was patient selection in order to avoid conversion, especially patients with ducts > 10mm.8,9
Despite the limited evidence in regard to the laparoscopic surgical management of chronic pancreatitis, the modified Puestow procedure is feasible and safe. It is in the early phase of development due to the limited number of cases reported worldwide. The present report is the first in the Mexican literature on the completely laparoscopic management. A characteristic of our clinic is the minimally invasive management of neoplastic and inflammatory pathologies in Mexico.10
Financial disclosureNo financial support was received in relation to this study/article.
Conflict of interestThe authors declare that there is no conflict of interest.
Please cite this article as: Crisanto-Campos BA, Trejo-Ávila ME, Román Ramírez E, Lina-López LM, Moreno-Portillo M. Pancreaticoyeyuno anastomosis totalmente laparoscópico (procedimiento de Puestow modificado). Reporte de caso. Revista de Gastroenterología de México. 2017;82:97–99.