Basal cell carcinoma (BCC) is the most frequent malignant neoplasia of the skin and makes up 75% of the non-melanocytic tumors.1 It more commonly presents in the male sex (80% of the patients) and the mean presentation age varies from 65-75 years.2 BCC frequently appears in areas exposed to ultraviolet radiation, mainly the head and neck. Its appearance at non-sun-exposed areas is atypical, and among those sites, location at the perianal region is extremely rare (0.1%), representing 0.2% of perianal tumors.3 Immunodeficiencies, infections, burns, chronic irritations, or previous radiation have been other etiopathogenic factors related to the appearance of this neoplasia. Likewise, certain hereditary syndromes, such as basal cell nevus syndrome or xeroderma pigmentosum, have also been implicated in its development.1,3
We present herein an unusual case of BCC located at the perianal level, with no predisposing factors.
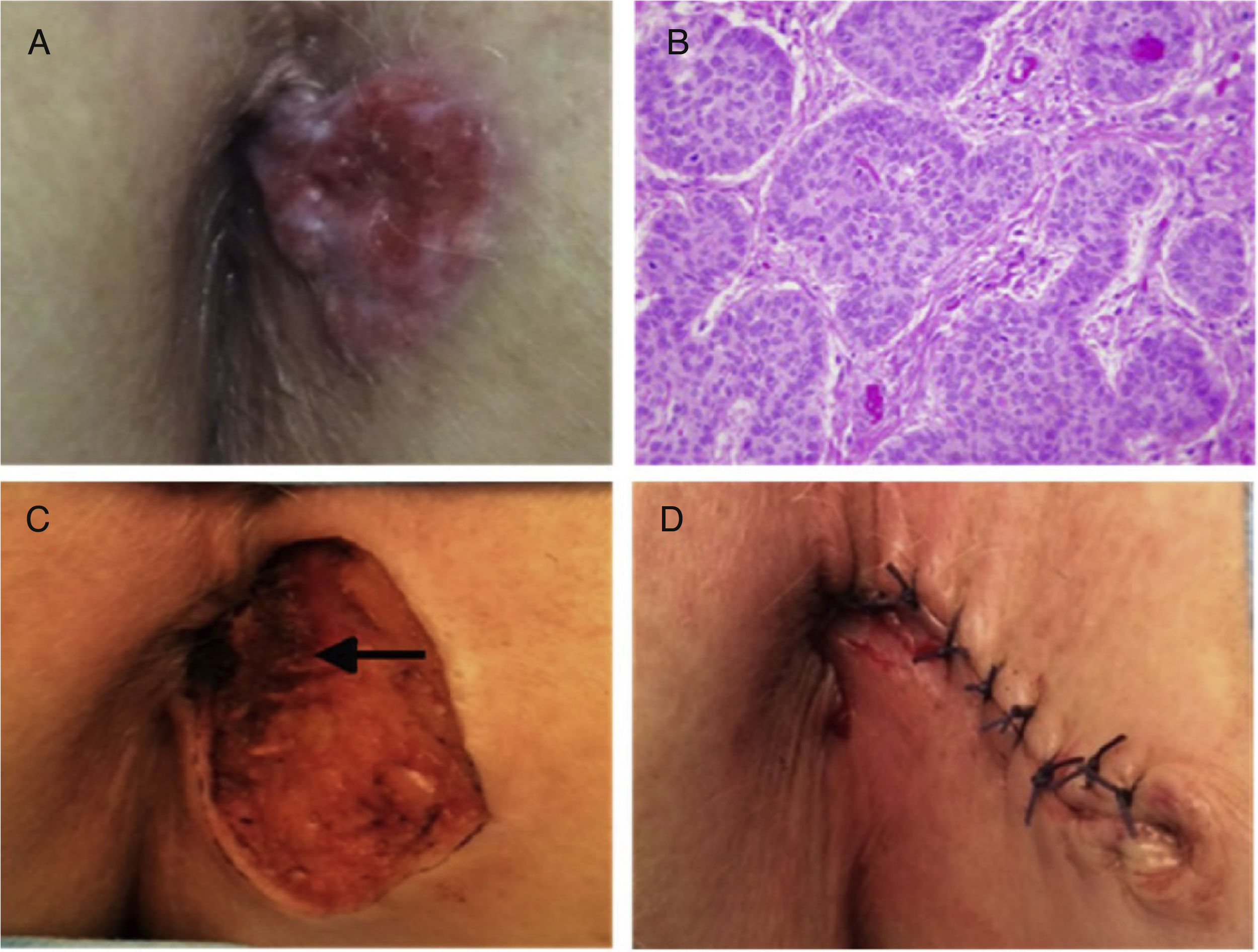
A 78-year-old woman with an unremarkable past medical history sought medical attention for a perianal lesion of 2-year progressive growth, associated with pruritus and occasional bleeding. Physical examination revealed a well-defined, ulcerated, erythematous neoformation, 3cm in diameter, at the left anal margin (fig. 1A). Nodular BCC diagnosis was made from the biopsy (fig. 1B). Rectosigmoidoscopy was performed, ruling out anal canal involvement. A pelvic magnetic resonance (MR) study identified no evidence of infiltration into the sphincteric musculature. The lesion was locally excised and repaired through primary cutaneous closure (figs. C and D). The histopathologic study reported microscopic infiltration of the internal margin and reintervention was carried out to widen the resection. Biopsy after reoperation confirmed tumor-free surgical margins. The patient had clinical follow-up and there are currently no signs of local recurrence at postoperative month 6.
A) Perianal erythematous papular lesion with pearly nodules and superficial ulceration. B) Histopathologic study: Basaloid cell nests with peripheral palisading on top of subepidermal loose connective tissue, consistent with nodular basal cell carcinoma (H&E x40). C) Detail of the surgical site after resection, showing the absence of infiltration into the sphincteric musculature (arrow). D) Aspect of the operating area after surgical reconstruction.
BCC presents as a cutaneous lesion with erythematous papules, nodules, and ulcerations.4 Gibson and Ahmed5 described an ulcerous presentation of those tumors in up to 29.4% of patients. They also classified BCC into the following subtypes: nodular (66%), superficial (18%), infiltrative (8%), micronodular (4%), basosquamous (2%), and as fibroepithelioma of Pinkus (2%). A lesion with those characteristics should be biopsied to confirm the diagnosis and rule out other perianal diseases, such as Crohn's disease, squamous cell carcinoma, adenocarcinoma, melanoma, neuroendocrine tumors, gastrointestinal stromal tumors, verrucous carcinoma, Kaposi sarcoma, or Paget disease.4,6 The differential diagnosis should include entities of infectious origin, such as sexually transmitted diseases, or less common dermatoses, including candidiasis, tuberculosis granuloma, fungal infections, and amoebiasis.6 It is particularly important to differentiate BCC from cloacogenic carcinoma, which is an aggressive, invasive tumor.1 Rectosigmoidoscopy and magnetic resonance imaging are the recommended complementary studies to rule out infiltration into the anal canal or sphincteric musculature invasion.
The current therapeutic options for BCC are exeresis, Mohs micrographic surgery, electrodessication and curettage, cryosurgery, radiation, or photodynamic therapy with aminolevulinic acid.7 Nonsurgical treatment includes the use of immune response modifiers, such as imiquimod. 8 Radiotherapy is the treatment of choice for lesions ≥ T2, elderly patients, or patients with relevant comorbidities.3,4 Standard treatment is local wide resection, but abdominoperineal resection may be necessary as rescue therapy or first-line treatment in patients with invasion proximal to the dentate line or the anal sphincter.3,9 Mohs micrographic surgery is generally used in patients with large lesions, recurrent tumors, or with lesions in esthetically exposed areas, such as the face. However, surgical excision is generally preferred over Mohs micrographic surgery, given that the latter requires specialized training and has a longer operating time and higher costs.7 The recurrence rate after standard exeresis with wide oncologic margins varies from 0-29%.3 The lapse of time from tumor appearance, tumor size above 2cm, or lesions with an infiltrative, micronodular, or morpheaform microscopic appearance are among the factors with a higher risk for recurrence.7 Vismodegib has been described as an efficacious therapeutic option in patients with locally advanced BCC or those with metastasis.10 Recurrences tend to be local and are treated with a new surgical resection or radiotherapy. BCC has a good prognosis, given that it is a slow-growing tumor with a low metastatic capacity.2,3 Five-year survival percentages of 100% have been reported in 2 large case series.2,5 The particularity of our case was the location of the pathology in a nonphotoexposed area and the absence of predisposing factors, emphasizing the fact that BCC should be included in the differential diagnosis when there is a slow-progressing perianal lesion.
Conflict of interestThe authors declare that there is no conflict of interest.
Please cite this article as: Fernández-Martínez D, Rodríguez-Infante A, Sanz-Navarro S, Miguel-Ruiz C, Baldonedo-Cernuda RF. Carcinoma basocelular perianal: una localización infrecuente. Revista de Gastroenterología de México. 2018;83:461–463.