Endoscopic retrograde cholangiopancreatography (ERCP) is the criterion standard for biliary and pancreatic drainage. Ten to fifteen percent of these procedures are reported as failed due to numerous causes, among which are: tumors, ductal stricture, ampullary fibrosis, giant gallstone, etc.1,2 Alternative bile duct access is transhepatic percutaneous biliary drainage (THBD) or surgical diversion (SD), both of which have high morbidity and mortality rates.3
Endoscopic ultrasound (EUS) provides clear, real-time images of the common bile duct and the main pancreatic duct, as well as of extraintestinal organs.4,5
There are different bile duct drainage techniques through EUS in relation to the access route: anterograde or choledochoduodenostomy (CD-EUS) access, whether through the transduodenal or transgastric routes in distal obstructions;6 transenteric or hepaticogastrostomy (EUS-HG) in proximal obstructions;6,7 and the transpapillary or “rendezvous” (EUS-RV) access, in which, through endoscopic ultrasound, a guidewire is advanced in an anterograde manner into the native ampulla, after which the common bile duct is cannulated with the duodenoscope alongside the guidewire, using the guidewire in a regular manner once it is retrieved by means of a metallic loop.8,9 Maranki et al. reported a success rate of only 57%,10 but Lee et al. described a rate of 94.1%.11
Even though this procedure is considered both adequate and successful, these techniques are not exempt from complications, among which include: pneumoperitoneum, biliary peritonitis, stent migration, hemorrhage, and sepsis.12
We describe herein 3 cases at our hospital in which these techniques were performed as palliative drainage due to unresectable advanced disease and failed ERCP. The materials used in all the cases were: a 19 G EchoTip®Ultra (Cook Medical®) fine needle, a 480-cm long TracerMetro® Direct Wire Guide (CookMedical®) 0.035″ guidewire, an ERCP1 5.5 Fr (Cook Medical) GloTip® catheter, and a 7.5 Fr×5.5cm controlled radial expansion balloon dilator with inflation diameters of 6-7-8mm (Boston Scientific).
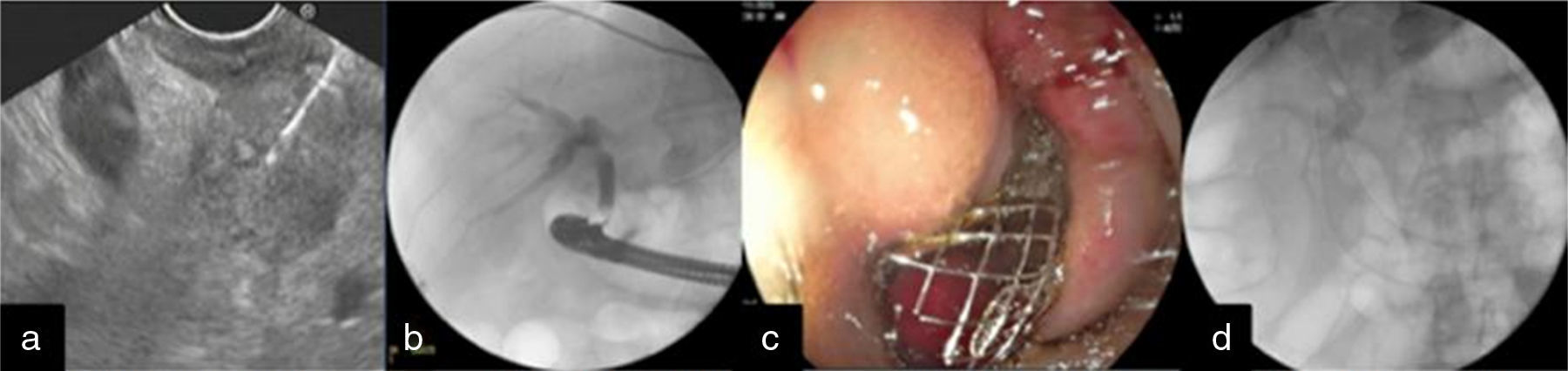
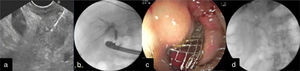
Case 1A 70-year-old man came to our service due to weight loss over the past 6 months, liver function tests reflecting cholestasis, and inability to eat. An abdominal computed tomography scan revealed a mass at the head of the pancreas and liver metastases. The ERCP procedure failed because tumor infiltration made it impossible to access the second portion of the duodenum. EUS revealed an unresectable heterogeneous tumor at the head of the pancreas with a diameter of 40×35mm, a 6-mm dilation of the common pancreatic duct, and a 14-mm dilation of the extrahepatic bile duct. Biliary drainage was carried out with the choledochoduodenal approach, using a linear echoendoscope (Pentax model EG-3870UTK®). The choledochus was punctured with a fine needle, contrast was injected to corroborate the site, and the hydrophilic guidewire was advanced. It was fistulized with a GloTip® catheter and dilated to 8mm with the CRE dilator. A fully covered Wallflex 10×40mm self-expanding metal biliary stent (Boston Scientific®) was placed, achieving spontaneous bile outflow. Finally, an uncovered 20×90mm self-expanding metal intestinal stent was advanced with a Savary-Guilliard® guidewire for intestinal permeability and corroborated through fluoroscopy (fig. 1). The patient progressed satisfactorily and was sent home for palliative care due to unresectable metastatic disease.
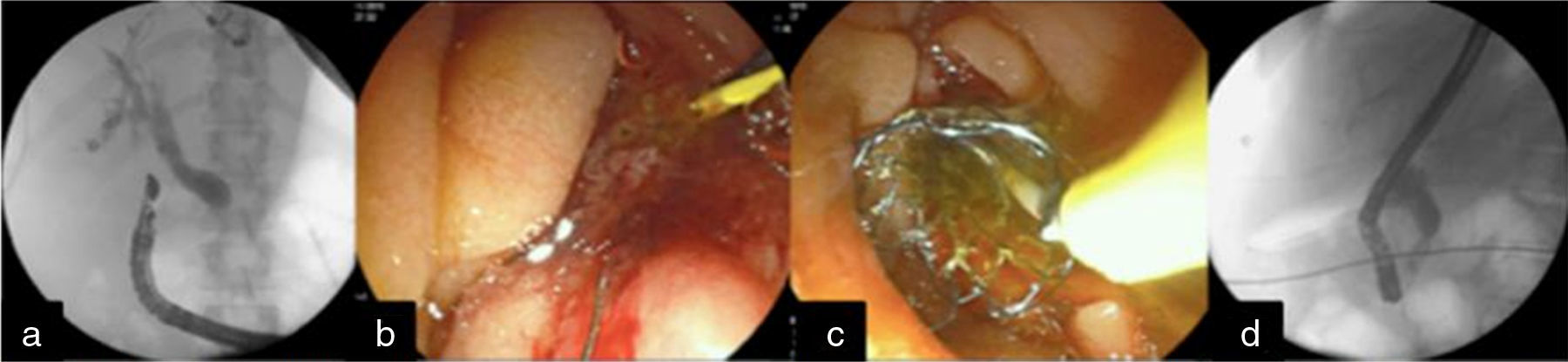
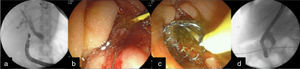
Case 2A 53-year-old woman presented with progressive jaundice, fever and 9-kg weight loss of 8-month progression. A tomography scan showed a pancreatic tumor with duodenal infiltration and liver metastases. Cannulation was impossible due to friability and tumor infiltration into the papilla major, resulting in a failed ERCP. EUS identified a heterogeneous mass in the pancreas with a diameter of 80×80mm. Drainage was carried out using the rendezvous technique (EUS-RV). The linear echoendoscope was introduced into the duodenal bulb, the proximal bile duct was punctured with a fine needle and opacified, and the hydrophilic guidewire was advanced. Through fluoroscopy, the guidewire was introduced in an anterograde manner in the direction of the ampulla until reaching the intestinal lumen. The duodenoscope was introduced and retrograde cannulation was carried out adjacent to the guidewire with a sphincterotome. Short sphincterotomy (5mm) was performed and a WallFlex® 10×60mm covered biliary stent was placed, achieving spontaneous bile output (fig. 2). The patient was sent home 24h later with no signs of complications or bile duct obstruction.
a) EUS-guided puncture of the common bile duct with fluoroscopic support and advancement of the guidewire into the duodenum, b). “Rendezvous” technique and common bile duct cannulation. c) Placement of the metal biliary stent, and d) Fluoroscopic view of the self-expanding metal biliary stent.
An 84-year-old woman presented with 10-kg weight loss, jaundice, and intermittent fever of 4-month progression. She was referred to our service due to severe cholangitis. EUS revealed a heterogeneous pancreatic tumor with a 40×50mm diameter that invaded the splenoportal confluence. Choledochoduodenal drainage was performed due to failed ERCP.
The linear echoendoscope was placed in the duodenal bulb, revealing intrahepatic and extrahepatic bile duct dilation of 13mm in diameter. Fine needle puncture was performed and the guidewire was advanced. Fistulization was carried out with a GloTip® catheter and a CRE balloon dilator was dilated to 6mm. Finally, a double pig-tail 40mm×10 Fr plastic biliary stent (CookMedical®) was advanced. Biliary drainage was technically successful.
Today, endoscopic ultrasound-guided biliary drainage is an alternative to failed ERCP drainage in patients with malignant distal biliary obstruction. It is considered a second-line technique, but the fact is that not all centers are equipped with endoscopic ultrasound and therefore continue to utilize surgical and/or radiologic drains.
Despite its being a complex procedure, the technical and clinical success rates of biliary drainage through EUS are similar to those of surgical drainage, but with a lower complication rate. Its performance requires careful patient selection, experienced operators, a multidisciplinary team, and the adequate accessories.
Conflict of interestThe authors declare that there is no conflict of interest.
Please cite this article as: Membrillo-Romero A, Altamirano-Castañeda ML, Muñoz-Bautista A. Drenaje biliar guiado por ultrasonido endoscópico en obstrucción maligna distal del conducto biliar común. Revista de Gastroenterología de México. 2018;83:75–76.