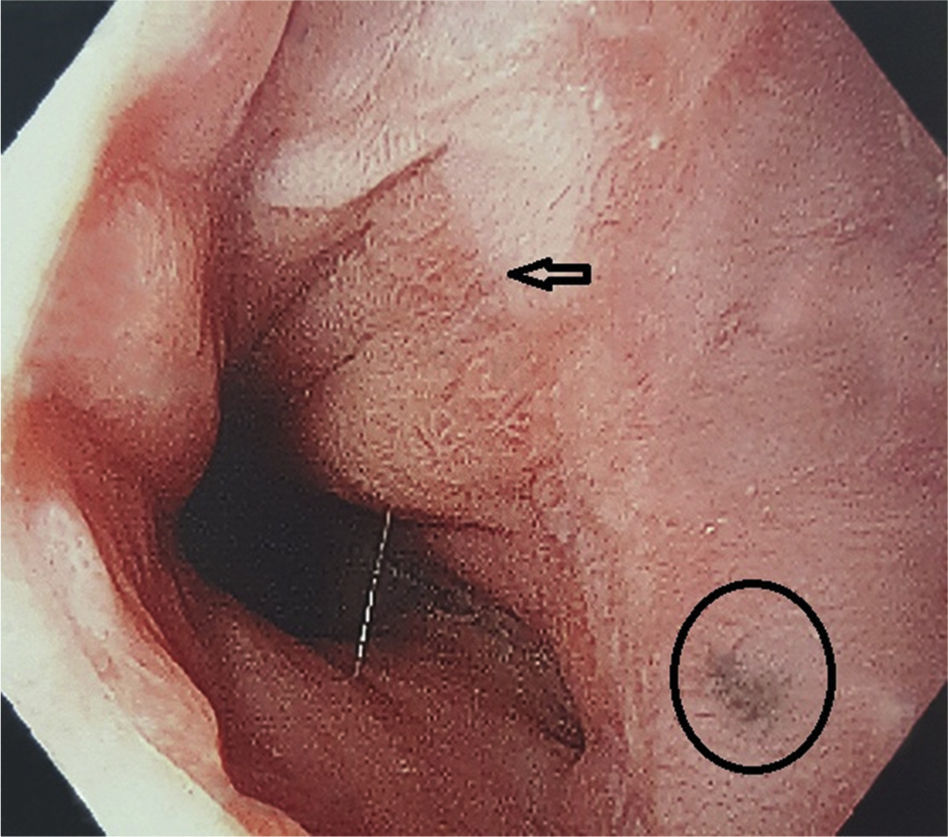
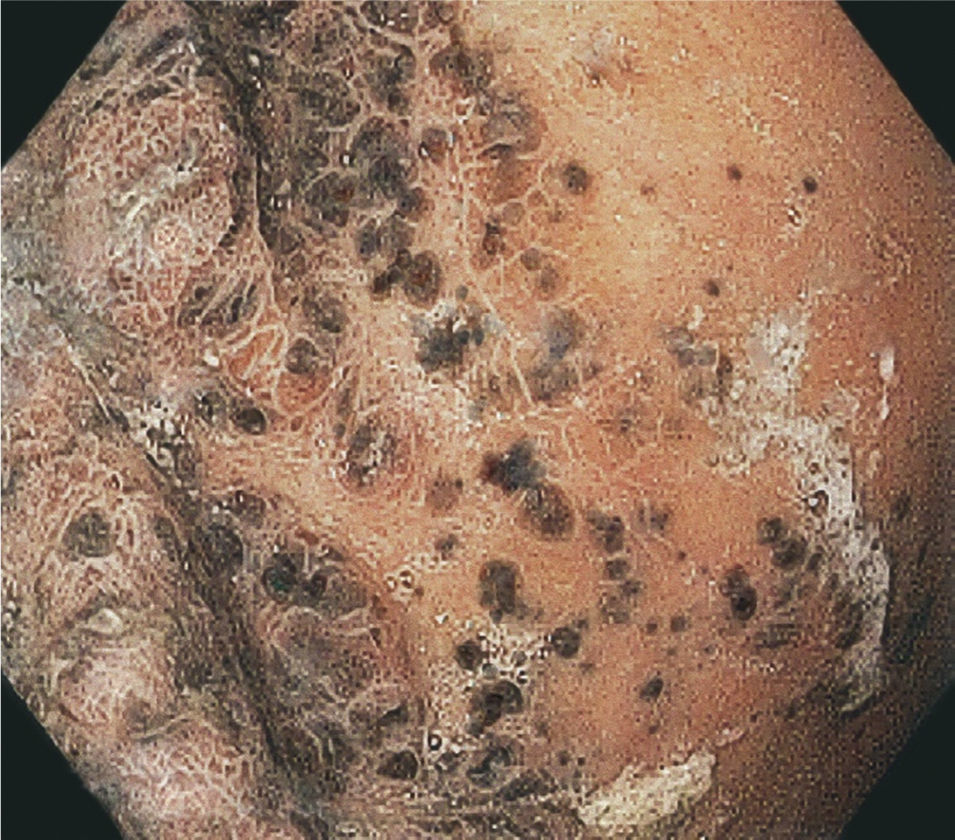
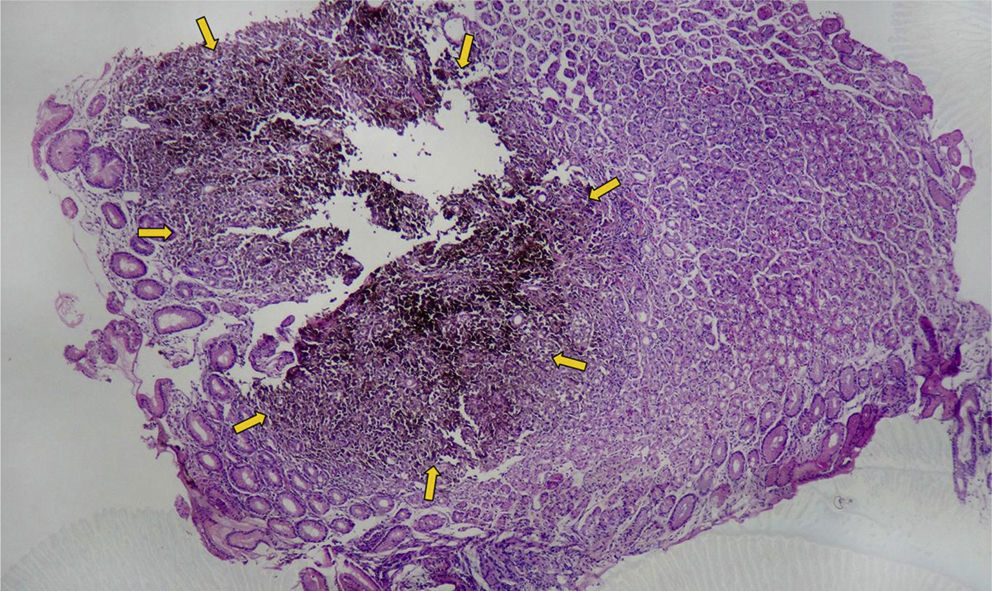
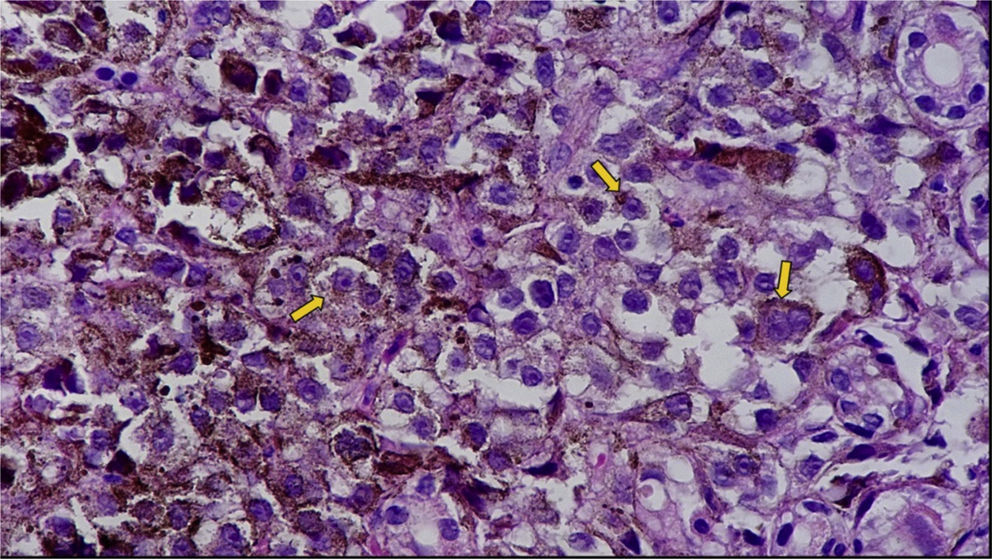
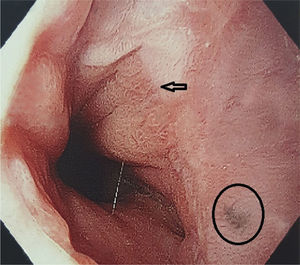
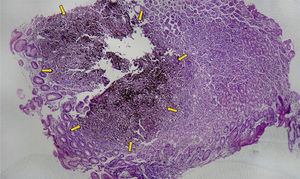
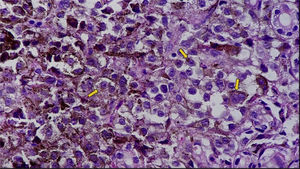
The stomach is the most common site of metastasis to the gastrointestinal tract from cutaneous melanoma, but the clinical diagnosis is made in less than 5% of those patients. We present herein the case of a 67-year-old man that had undergone wide local excision of an invasive ulcerated melanoma on the back (Clark III, Breslow 1.8mm, stage IIIB) 2 years prior, with positive sentinel lymph node biopsy. He also had complete left axillary lymph node dissection and radiotherapy in the same lymph node area. After presenting with painless episodes of lower gastrointestinal bleeding, the patient underwent esophagogastroduodenoscopy. In the medical interview, he did not complain of other abdominal symptoms. Colonoscopy was normal, with the exception of internal hemorrhoids. The esophagogastroduodenoscopy incidentally revealed multiple melanocytic lesions of different sizes, some of which were ulcerated, with no signs of active bleeding. There were no lesions in the pylorus or duodenum (figs. 1–3). Numerous biopsies were sent to the pathology department, which confirmed the diagnosis of gastric metastasis from cutaneous melanoma (figs. 4–5). At the time of the finding, the patient already presented with CNS invasion and perigastric, hepatogastric, peripancreatic, celiac, and para-aortic adenopathies. He received medical oncologic systemic treatment, but due to disease extension and progression, outcome was unfavorable.
The authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of dataThe authors declare that no patient data appear in this article.
Right to privacy and informed consentThe authors declare that no patient data appear in this article.
Financial disclosureNo financial support was received in relation to this article.
Conflict of interestThe authors declare that there is no conflict of interest.
Please cite this article as: Bercholc-Urinowsky IJ, Aristi-Urista G, Shueke-Esses M. Diagnóstico endoscópico incidental de metástasis gástrica por melanoma cutáneo. Revista de Gastroenterología de México. 2017;82:337–338.