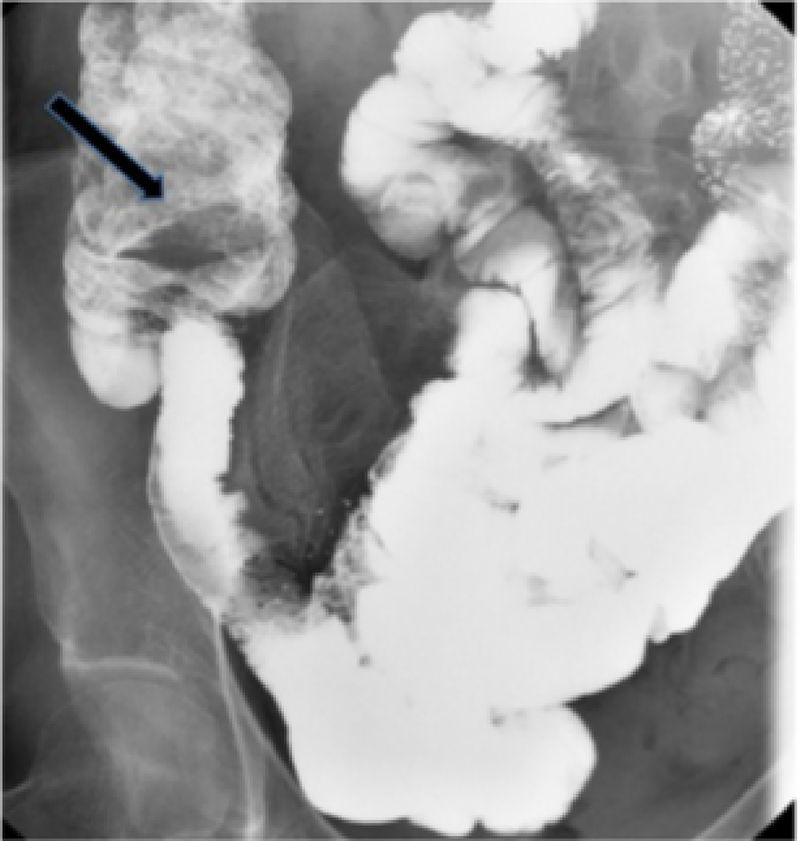
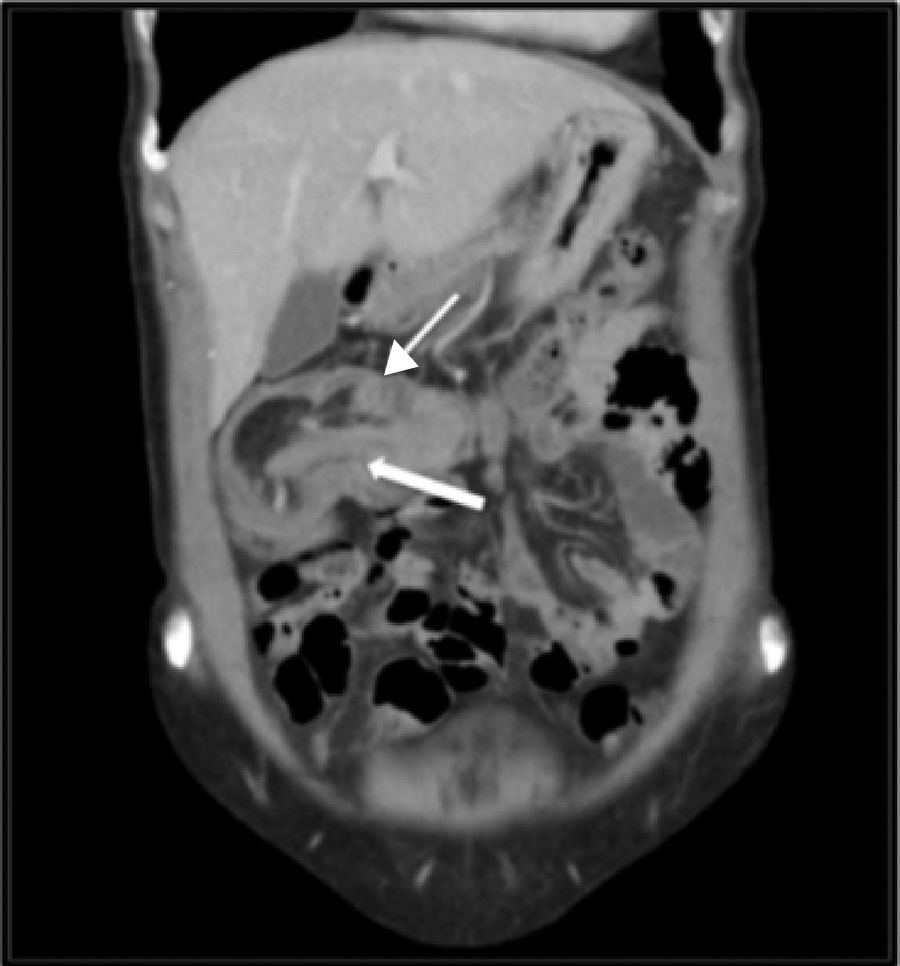
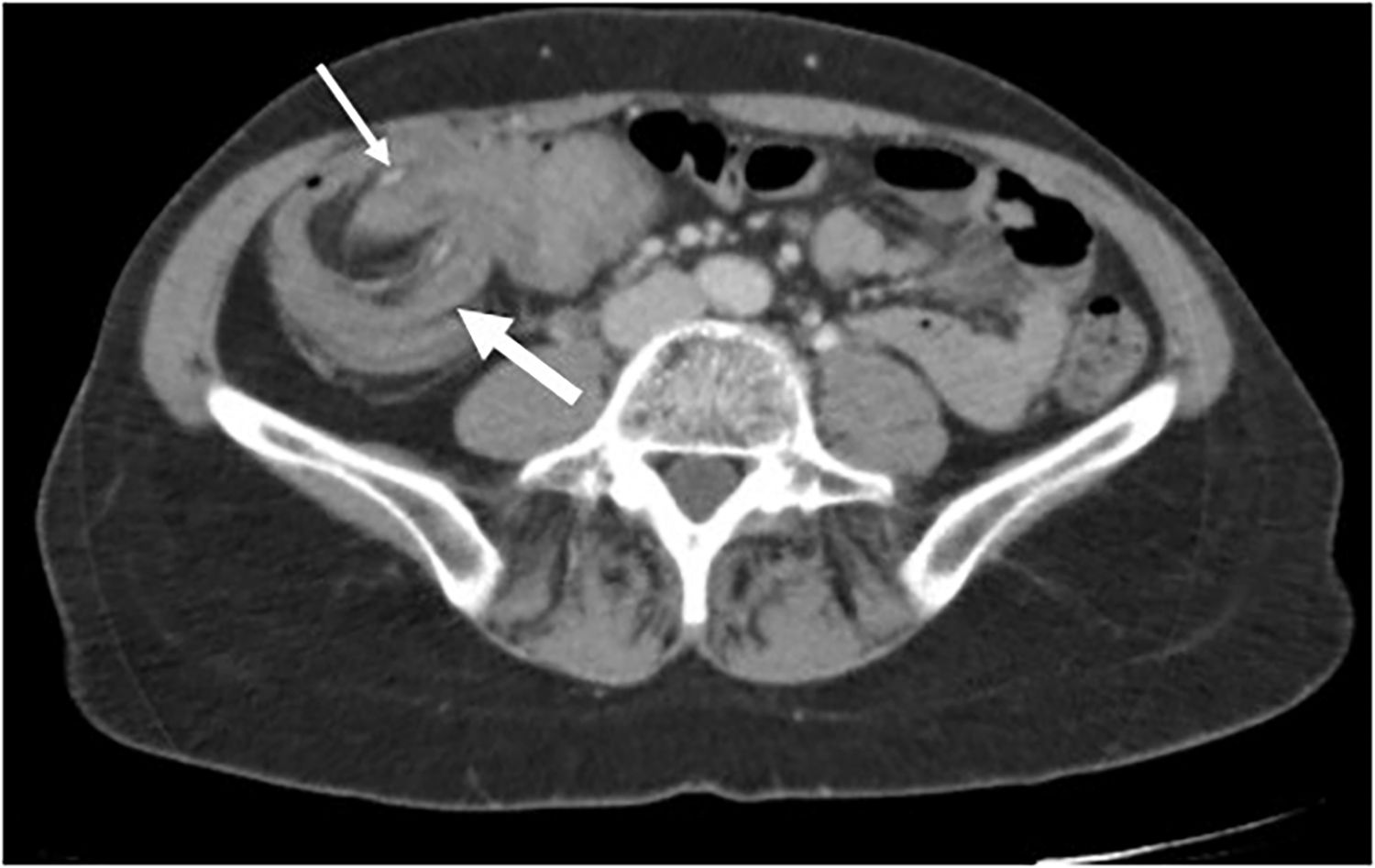
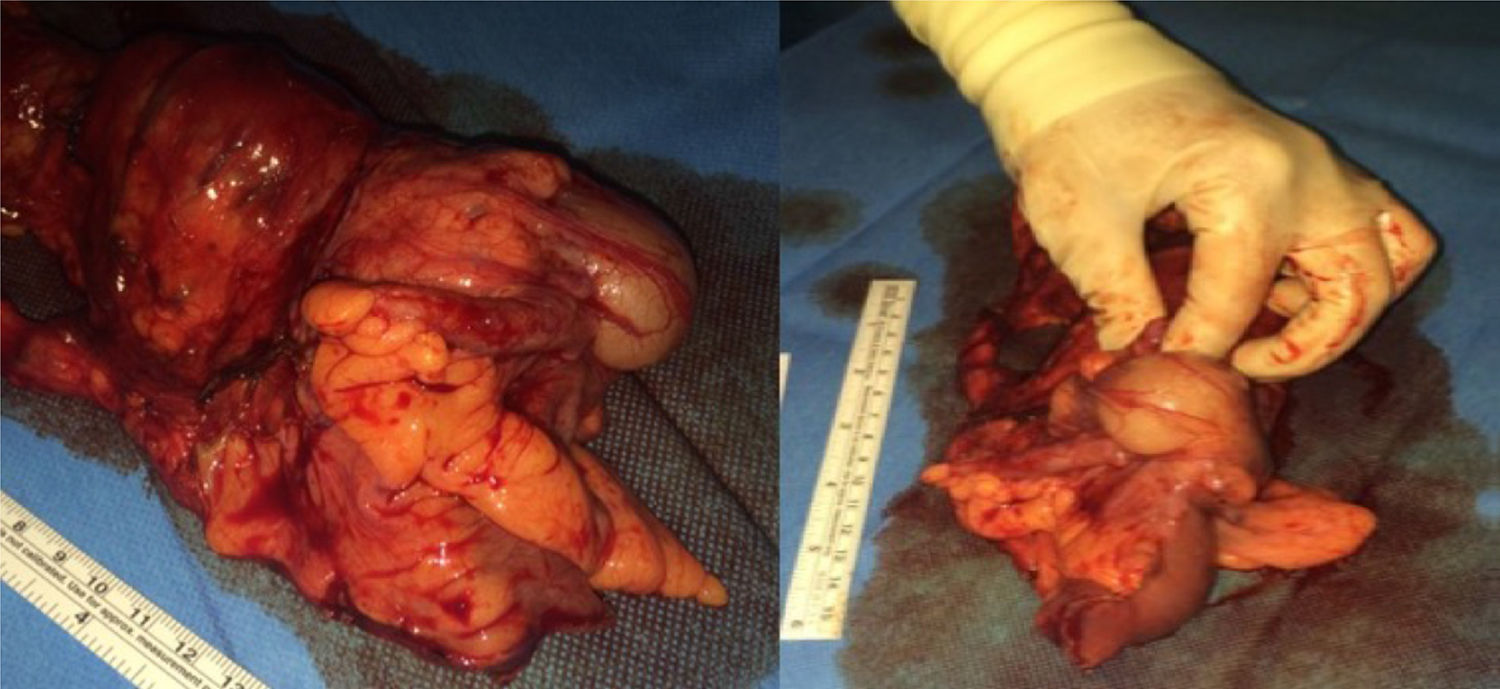
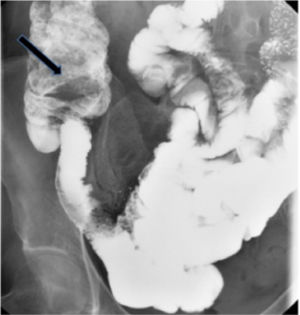
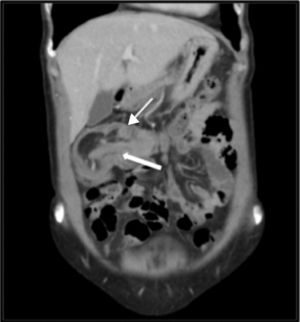
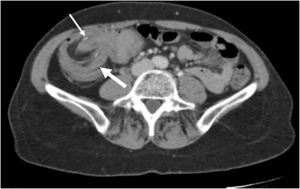
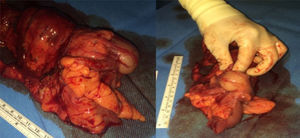
A 56-year-old woman came to the emergency department presenting with colicky pain in the right iliac fossa of 48-h progression that radiated to the right hypochondrium and the epigastrium, associated with diarrhea. She had undergone gastrointestinal evaluation due to complaints of similar episodes over the past 5 months. Abdominal ultrasound image was normal and bowel transit showed a filling defect located in the cecum, suggestive of a tumor (fig. 1). Abdominal examination revealed pain in the right iliac fossa and the epigastrium, with no signs of peritoneal irritation or increased bowel sounds. There were no important alterations in the laboratory tests. Abdominal CAT scans identified a large mass situated in the middle third of the transverse colon with interposition of the proximal ileum inside the ascending-transverse colon suggestive of invagination, with «sausage-shaped» mass or «target sign» images (figs. 2 and 3), and bowel segments of normal caliber. Urgent surgery was indicated, and radical oncologic right hemicolectomy was performed (fig. 4). The anatomopathologic study of the surgical specimen reported poorly differentiated pT1N0 adenocarcinoma of the cecum.
The authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of dataThe authors declare that no patient data appear in this article.
Right to privacy and informed consentThe authors declare that no patient data appear in this article.
Financial disclosureNo specific grants were received from public sector agencies, the business sector, or non-profit organizations in relation to this study.
Conflict of interestThe authors declare that there is no conflict of interest.
Please cite this article as: de Andrés-Asenjo B, Gómez-Carmona Z, Blanco-Antona F, Beltrán de Heredia-Rentería J. Invaginación ileo-cólica transversa: causa infrecuente de abdominalgia inespecífica en el adulto. Revista de Gastroenterología de México. 2019;84:100–101.