Untreated celiac disease has traditionally been linked to a greater risk for small intestinal bacterial overgrowth, but the existing evidence is inconclusive.
AimsTo compare the prevalence of small intestinal bacterial overgrowth in subjects with celiac disease compared with control subjects and patients with irritable bowel syndrome.
Material and methodsThe study included 15 untreated celiac disease patients, 15 subjects with irritable bowel syndrome, and 15 healthy controls. All enrolled patients underwent a lactulose breath test measuring hydrogen and methane. Small intestinal bacterial overgrowth was defined according to previously published criteria.
ResultsNo differences were found in relation to age or sex. The prevalence of small intestinal bacterial overgrowth was similar between the celiac disease patients and the controls (20 vs. 13.33%, P=NS), whereas it was higher in patients with irritable bowel syndrome (66.66%, P<05).
ConclusionThere was no difference in the prevalence of small intestinal bacterial overgrowth between the untreated celiac disease patients and healthy controls.
Clásicamente, se ha vinculado a la enfermedad celíaca no tratada con un mayor riesgo de sobrecrecimiento bacteriano. Sin embargo, la evidencia existente no es concluyente.
ObjetivoComparar la prevalencia de sobrecrecimiento bacteriano en sujetos celíacos con respecto a sujetos controles y a pacientes con síndrome de intestino irritable.
Material y métodoFueron inscritos 15 pacientes celíacos no tratados, 15 sujetos con síndrome de intestino irritable y 15 sujetos controles sanos. Los pacientes inscritos realizaron un test de hidrógeno/metano en aire espirado con lactulosa. Se definió al sobrecrecimiento bacteriano según criterios previamente publicados.
ResultadosNo se encontraron diferencias en cuanto a edad y sexo. La prevalencia de sobrecrecimiento bacteriano fue similar entre celíacos y controles (20 vs. 13.33%, p=NS), mientras que fue mayor en pacientes con síndrome de intestino irritable (66.66%, p<0.05).
ConclusiónLos celíacos no tratados presentan una prevalencia de sobrecrecimiento bacteriano no diferente a los sujetos sanos.
Celiac disease is an immunologic disorder in which an inflammatory alteration is produced due to exposure to gluten, with varying degrees of villous atrophy and nutrient malabsorption.1 Current treatment consists of a gluten-free diet.
Untreated and/or refractory celiac disease has traditionally been linked to a greater risk for developing small intestinal bacterial overgrowth, but conclusive evidence with respect to this is lacking.2,3
Small intestinal bacterial overgrowth diagnosis is difficult. A noninvasive alternative is the hydrogen/methane breath test.4 Its usefulness for this purpose is controversial because of the influence of bowel transit time on the results. Nevertheless, it continues to be a widely used tool in clinical practice.
The evidence with respect to the prevalence of small intestinal bacterial overgrowth measured by breath test in celiac disease subjects is scarce and contrasting. Therefore our aim was to compare the results of said test in celiac disease subjects with those of healthy controls and patients with irritable bowel syndrome (IBS) in whom such alteration is frequently observed.5
MethodsPatient selectionPatients above the age of 18 years that were seen at the Gastroenterology Section of our institution within the time frame of January 2013 and December 2014 were evaluated. On the one hand, subjects were enrolled that had a recent diagnosis of celiac disease and that had not yet begun treatment with a gluten-free diet. Celiac disease patients were defined as those patients with positive IgA or IgG anti-tissue transglutaminase and/or anti-endomysial antibodies, together with a duodenal biopsy showing signs of villous atrophy (Marsh III).
On the other hand, subjects were enrolled that had IBS diagnosis without constipation and that were negative for celiac disease antibodies. IBS was defined in accordance with the Rome III criteria.6 And finally, healthy subjects seen at our institution for preventive clinical control were invited to participate if they did not present with digestive symptoms and were negative for celiac disease antibodies. The subjects were enrolled in a 1:1:1 ratio.
Those subjects suspected of concomitant digestive disease, that were pregnant, and patients that had taken antibiotics or probiotics within the last 30 days or prokinetics in the last 2 weeks, were excluded from the study.
Breath testOnce the written statements of informed consent were signed, the enrolled subjects were given a hydrogen/methane breath test utilizing lactulose as a substrate. The celiac disease subjects took the test before beginning the gluten-free diet. The tests were performed using the previously described technique:7 after the subjects fasted for 12h and were on a low fermentable carbohydrate diet, they provided breath samples before (baseline sample) and after ingesting 10ml of lactulose every 20min for 180min. The samples were analyzed with a chromatograph (BreathTracker® SC. QuinTron Instruments Company; Milwaukee, WI, USA) to determine the excreted hydrogen and methane concentrations, which were measured in particles per million (ppm). Curves were drawn illustrating the excreted gas concentrations in relation to time.
The presence of anomalous hydrogen and/or methane excretion considered consistent with small intestinal bacterial overgrowth was evaluated for each case. Any of the following findings were regarded as abnormal: a) hydrogen excretion greater than 20ppm before 90min or an initial peak of 12ppm before 90min followed by a decrease of at least 5ppm and a later increase (double hydrogen peak), and b) an increase in methane excretion greater than 3ppm at any time during the test.
In addition, the presence of an elevated baseline value of hydrogen and/or methane (value greater than 3ppm of methane and 12ppm of hydrogen) was registered.
Statistical analysisStatistical analysis was carried out using the Stata® version 11.1 statistics program (Statacorp, College Station; Texas, USA). Numerical values were described as means with their standard deviations. Categorical variables were described as percentages. The ANOVA test was utilized for the numerical variable comparison and the Fisher test for comparing the categorical variables. Odds ratios (OR) were calculated with their corresponding 95% confidence intervals (95% CI). Statistical significance was set at a value of p less than 0.05.
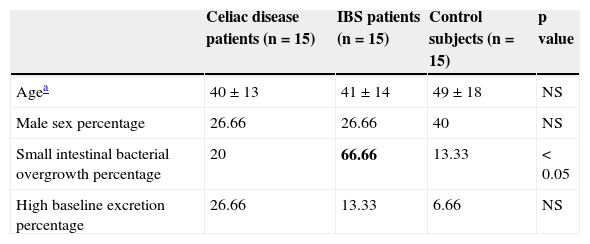
ResultsA total of 15 recently diagnosed celiac disease patients, 15 patients with IBS, and 15 healthy controls were enrolled in the study. Table 1 shows the comparison of the demographic data, as well as the prevalence of small intestinal bacterial overgrowth measured by breath test by group.
Comparison of the study group characteristics.
| Celiac disease patients (n=15) | IBS patients (n=15) | Control subjects (n=15) | p value | |
|---|---|---|---|---|
| Agea | 40±13 | 41±14 | 49±18 | NS |
| Male sex percentage | 26.66 | 26.66 | 40 | NS |
| Small intestinal bacterial overgrowth percentage | 20 | 66.66 | 13.33 | <0.05 |
| High baseline excretion percentage | 26.66 | 13.33 | 6.66 | NS |
NS: not significant; IBS: irritable bowel syndrome.
There was significant difference in small intestinal bacterial overgrowth prevalence in IBS subjects with respect to the other 2 groups (66.66 vs. 20% in celiac disease patients and 13.33% in the controls). This difference presenting in the IBS patients was significant when compared with both the celiac disease group (OR 8 [1.52-42.01], p=0.02) and the control group (OR 13 [2.07-81.48], p=0.007). No differences were found between the celiac disease patients and the controls (OR 1.62 [0.23-11.46], p=NS). Even though the difference was not statistically significant, the celiac disease patients presented with a greater frequency of elevated baseline values compared with the other groups. The patients that presented with a positive test for small intestinal bacterial overgrowth with compatible digestive symptoms were treated with 1,200mg/day of rifaximin for 2 weeks. Two weeks after having finished treatment, 77% of the patients had complete symptom resolution. No significant differences were found in relation to the antibiotic response between the evaluated groups.
DiscussionIn accordance with our results, there was no difference in small intestinal bacterial overgrowth prevalence measured through breath test between untreated celiac disease patients and healthy controls, but there was increased prevalence in the IBS subjects.
There is evidence as to a relation between altered breath test results in an IBS context and small intestinal bacterial overgrowth prevalence measured by this method in more than 80% of the cases.5 In a celiac disease context, there is far less evidence.
In this sense, Corazza et al.8,9 have observed an increase in the baseline value of hydrogen in untreated celiac disease subjects; this alteration was corrected with a gluten-free diet. On the other hand, Chang et al.2 found no significant differences in hydrogen excretion between celiac disease patients and controls. Our experience with untreated active celiac disease patients was that hydrogen values were not different, compared with those of the controls, and they were significantly lower when compared with the IBS subjects. Celiac disease patients present with intestinal motility alterations that can predispose to small intestinal bacterial overgrowth; nevertheless, prevalence is variable. Most likely small intestinal bacterial overgrowth prevalence is greater in celiac disease patients with digestive symptoms related to gases. Therefore, it is to be expected that in an unselected celiac disease patient population, prevalence would be similar to that of the general population, as was shown in our study. The addition of excreted methane values provides a more complete perspective to previous studies that suggested these findings, only measuring hydrogen in the breath test.
Although the value of the lactulose breath test for small intestinal bacterial overgrowth diagnosis is debatable, it is undeniable that the difference in hydrogen and methane excretion reflects a difference in the fermentative capacity of non-absorbable substrates on the part of the gut microbiota, regardless of whether or not this results in actual small intestinal bacterial overgrowth. Thus, our experience was valuable in that we found a difference between patients with celiac disease and healthy controls in relation to patients with IBS. The relatively small sample size of our patient population should be underlined as a limitation of our study, as well as the fact that the patients did not undergo a duodenal aspirate culture. Even though it is regarded as the criterion standard diagnostic test, it can be difficult to reproduce.
In conclusion, the patients with untreated celiac disease presented with hydrogen and methane excretion profiles consistent with small intestinal bacterial overgrowth that were similar to those of subjects with no digestive disorders, but significantly different from those of patients with IBS.
Financial disclosureNo financial support was received in relation to this study/article.
Conflict of interestThe authors declare that there is no conflict of interest.
Please cite this article as: Lasa JS, Zubiaurre I, Fanjul I, Olivera P, Soifer L. La prevalencia de sobrecrecimiento bacteriano en celíacos es similar a la de sujetos sanos y menor que en pacientes con síndrome de intestino irritable. Revista de Gastroenterología de México. 2015;80:171–174.