Celiac disease (CD) is a process with an autoimmune base that affects the small bowel and is triggered by the ingestion of gluten in genetically susceptible individuals. Numerous complications associated with CD have been described, among which cavitating mesenteric lymph node syndrome (CMLNS) stands out for its rarity. Little is known of its etiopathogenesis, and it should be recognized early and differentiated from infections and lymphoma, in particular. We present herein a case of CD with this complication associated with other concomitant diseases with an autoimmune base.
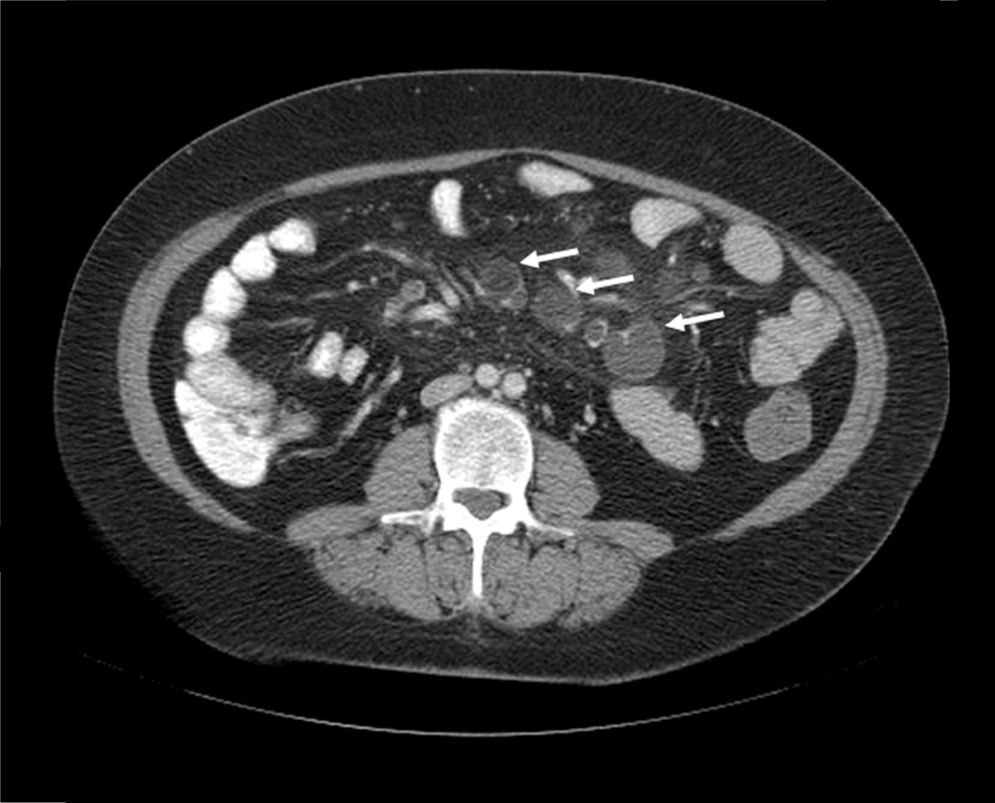
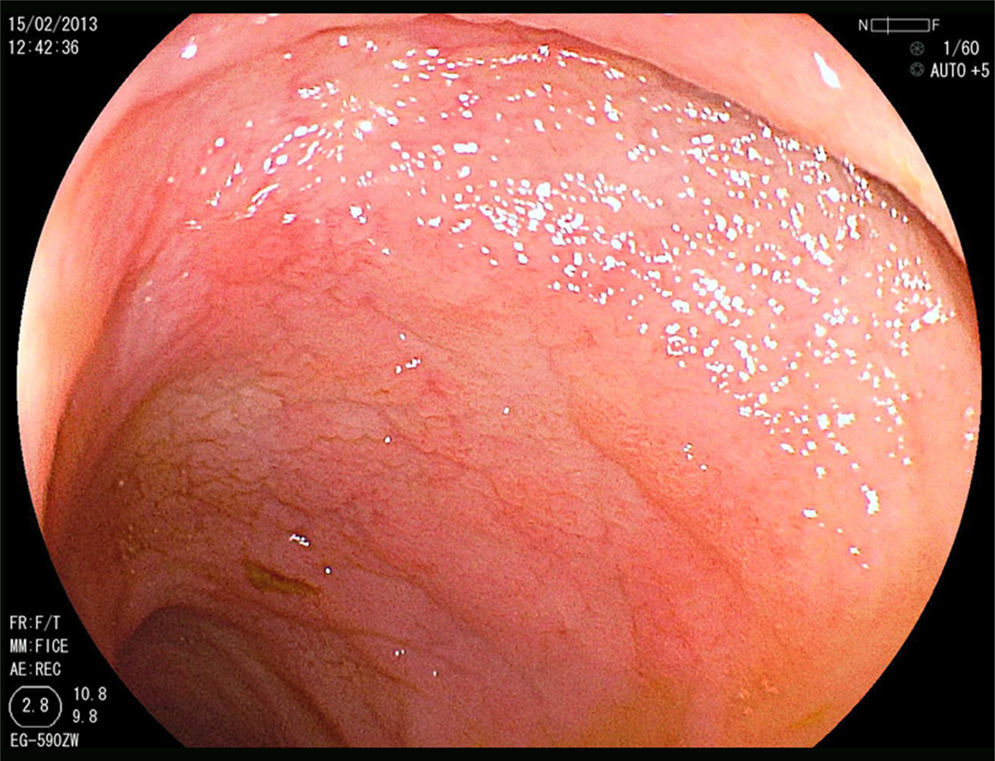
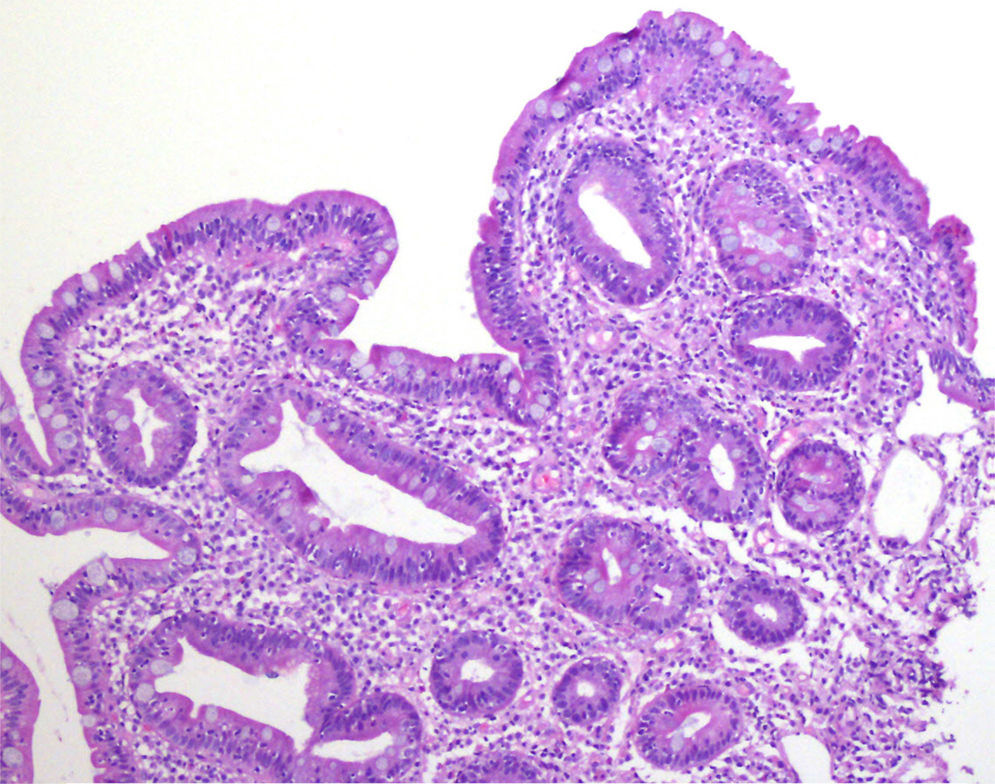
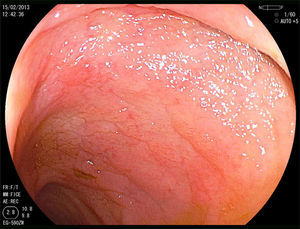
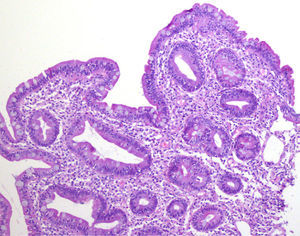
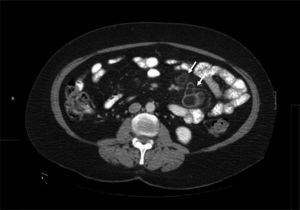
A 52-year-old woman was diagnosed with Sjögren syndrome (SS) and she sought medical attention for altered transaminases and cholestatic enzymes, and positive AMA with positive M2 and elevated IgM. An abdominal ultrasound (US) study and liver biopsy were ordered and treatment with ursodeoxycholic acid at a dose of 14mg/kg/day was begun due to primary biliary cholangitis (PBC) diagnosis. The patient complained of non-bloody, pasty stools 4-5 times a day over a 6-month period and a consequent weight loss of 8kg. Physical examination was normal. Weight: 65kg and height: 167cm. Body mass index: 23.3. The remarkable laboratory test results were: alanine aminotransferase: 68 (0-31) U/l; aspartate aminotransferase: 113 (0-55) U/l; alkaline phosphatase: 264 (5-36) U/l; GGT: 341 (35-104) U/l; immunoglobulins: IgM: 624mg/dl (40-230); AMA: 1/604; AMA-M2: positive; and anti-transglutaminase: 160 U (0-20). The US study identified pathologic mesenteric adenopathies with a cystic appearance. Tumor markers were normal. The microbiology study was negative for human immunodeficiency virus and tuberculosis. A thoracoabdominal computerized tomography (CT) scan showed multiple adenopathies in the mesentery > 1cm, with a rounded cystic aspect and low attenuation in the central area (fig. 1). Colonoscopy was normal and gastroscopy revealed an atrophied duodenal nodular mucosal pattern that was histologically consistent with Marsh IIIa stage disease (figs. 2 and 3). Liver biopsy was consistent with stage II PBC.
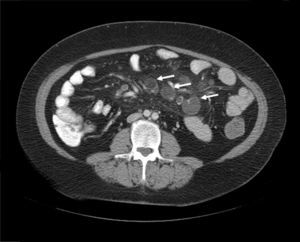
Once infections (tuberculosis and Whipple's disease) and Crohn's disease were ruled out, the main differential diagnosis was lymphoma. Given the CD diagnosis, the radiologic characteristics of the adenopathies, and the exclusively mesenteric location, no histologic study was carried out given the low probability of lymphoma. The findings were interpreted as CMLNS and a gluten-free diet (GFD) and early radiologic control were decided upon. At 3 months, the patient had gained 3kg and the control CT scan showed adenopathy cavitation and reduced size, corroborating the diagnosis (fig. 4).
CMLNS is a very rare complication of CD and its pathogenesis is unknown. It is postulated that an alteration in intestinal permeability could favor massive and chronic exposure to certain antigens, causing ischemic damage from the deposit of immune complexes on the vascular endothelium of the lymph node, and its consequent necrosis.1
This entity presents with the usual symptoms of CD, mesenteric adenopathies, and sometimes with hyposplenism, and should always be suspected in celiac patients with a poor response to a GFD.
The clinical and radiologic data are essential for diagnosis, and CT is the main study.2 The initial CT finding is the presence of multiple adenopathies located exclusively in the jejunal-ileal mesentery of various sizes (2-7cm) and with central areas of low attenuation (density of 30-40 HU or lower) produced by the presence of fluid and/or fat.
Occasionally, fluid-fat levels are observed in the adenopathies, which is a typical radiologic sign of CMLNS. Nuclear magnetic resonance can be useful for viewing fluid-fat levels, using T1 and T2 weighted sequences with fat saturation techniques, even if the fluid-fat levels are not seen in the CT scans.3 Some authors state that the demonstration of these changes in the adenopathies through magnetic resonance can eliminate the use of other more invasive techniques, such as lymph node puncture.4
The main differential diagnoses to be made with CMLNS are infections and lymphoma. Adenopathies from lymphoma have soft tissue attenuation with no cavitation, various lymph node chains are affected, and splenomegaly is common. Infections, such as tuberculosis and Whipple's disease, can sometimes have non-cavitating, low-attenuation abdominal adenopathies and the laboratory, endoscopic, clinical, and radiologic data are very important for their diagnoses.5
Patients that do not clinically improve with a GFD or that have uncharacteristic radiologic findings, must undergo a radiologic or surgery-guided biopsy to obtain a histologic study of the adenopathy.
The pathognomonic CMLNS signs of progressive cavitation of the adenopathies and a decrease in their size are observed after starting a GFD. In addition to the typical CD dietary restrictions, the intensive use of systemic corticoids is sometimes necessary.6 Even though initial publications described an elevated mortality rate in patients with CMLNS, new studies have reported progression that is similar to that of the rest of celiac patients.7
In conclusion, CMLNS is an extremely rare complication of CD that must be differentiated from other clinical entities upon diagnosis and during its progression. Diagnosis can be made through a combination of clinical and radiologic data.
Financial disclosureNo financial support was received in relation to this article.
Conflict of interestThe authors declare that there is no conflict of interest.
The authors wish to thank the gastroenterologists that participated in the study.
Please cite this article as: Ruiz-Clavijo García D, García de Galdiano Fernández A, González de la Higuera Carnicer B, Rubio-Marco I, Mercado Gutiérrez M. Síndrome del nódulo mesentérico cavitado: complicación infrecuente de la enfermedad celíaca. Revista de Gastroenterología de México. 2017;82:351–353.