Anal sphincter spasm contributes to the delay in surgical wound healing after hemorrhoidectomy. A prospective, experimental, randomized, double-blind trial was conducted on two groups of patients that underwent closed hemorrhoidectomy. There were 26 patients in each group. Group A received topical diltiazem in the anal region three times a day. Group B received a placebo. Cicatrization time was documented for 6 weeks through digital photography. Mean healing time for the group treated with diltiazem was 3.19 weeks (22.33±0.884 days) and 3.92 weeks (27.44±1.130 days) for the control group (p=0.012 95% CI). At week three, the wounds in 73.07% of the patients in the diltiazem group had healed, compared with 46.15% of the patients in the control group.
El espasmo del esfínter anal contribuye al retardo en la cicatrización de las heridas quirúrgicas después de una hemorroidectomía. Se realizó un estudio aleatorizado, prospectivo, experimental, doble ciego, de dos grupos de pacientes en los que se efectuó hemorroidectomía con técnica cerrada. Cada grupo incluyó 26 pacientes; el grupo A recibió diltiazem tópico en la región anal 3 veces al día, y el grupo B recibió un placebo. Se documentó el tiempo de cicatrización, mediante fotografía digital, durante 6 semanas. El promedio del tiempo de cicatrización para el grupo tratado con diltiazem fue de 3.19 semanas (22.33±0.884 días); en tanto que en el grupo control fue de 3.92 semanas (27.44±1.130 días) (p=0.012 IC 95%). A la tercera semana, el 73.07% de los pacientes del grupo tratado con diltiazem habían cicatrizado, en comparación con el 46.15% de los pacientes del grupo control.
Hemorrhoidectomy has been associated with postoperative pain and slow surgical wound cicatrization. Anal sphincter spasm has been signaled as one of the factors that favors surgical would healing delay after hemorrhoidectomy.
To reduce anal sphincter pressure after hemorrhoidectomy and shorten the healing time of those surgical wounds, studies on topical nitroglycerin and botulinum toxin have been conducted.1,2 Topical diltiazem also reduces maximum resting pressure of the anal sphincter, and so it has been used for the treatment of anal fissures.3 In addition, it has been shown to reduce postoperative pain after hemorrhoidectomy.4
The exclusive aim of our study was to evaluate the efficacy of topical diltiazem in reducing surgical wound healing time after hemorrhoidectomy.
Materials and methodsAn experimental, prospective, longitudinal, randomized, double-blind study was conducted on 52 patients diagnosed with grade III and IV internal hemorrhoid disease that underwent closed Ferguson hemorrhoidectomy.
Sample size was calculated considering the fact that the worldwide incidence of hemorrhoidal disease in the general population is 6%. Nevertheless, given the use of conservative measures and nonsurgical treatment, such as elastic band ligature, infrared photocoagulation, and sclerotherapy, only one-fourth of the patients with hemorrhoidal disease is estimated to require some type of surgical treatment. In other words, just 1.5% of the general population will require a surgical procedure.
All the patients were operated on by the same surgeon and three primary hemorrhoidal cushions were resected in all cases. All the surgeries were carried out with 000 absorbable monofilament suture, hemostasis was performed through electrocautery, and a hemostatic sponge was placed at the end of the intervention.
None of the patients had diabetes mellitus or cardiovascular disease, nor were they under treatment with steroids or calcium channel antagonists. With respect to female patients, none were pregnant or became pregnant within the study period. The patients with grade III and grade IV hemorrhoid disease were not placed into separate groups, considering that the classification evaluates the degree of protrusion, rather than the size of the hemorrhoidal cushions.
The patients were randomly divided into two groups of 26 patients each group. The patients in group A received topical diltiazem (gel at 2%) in the immediate postoperative period and treatment continued for 6 weeks, applying the topical medication 3 times a day. The patients in group B were given a placebo, with the same indications as in group A.
Both the diltiazem gel at 2% and the placebo had the same physical characteristics. The patients were given a dosing syringe and instructed to apply 0.5ml of the product in the anal region, the equivalent of 10mg per dose. The syringes were randomly marked with a progressive number and the study was double-blinded.
The data was carefully recorded throughout the randomized study. Without knowing its content, the number of the syringe corresponding to each patient was written down. The list that identified the syringes containing diltiazem and those with the placebo was made by an independent assistant who swore not to reveal its content, and it was kept in a closed envelope until the end of the study.
The patients in each group received standard post-hemorrhoidectomy treatment throughout the study: sitz baths in warm water every 6hours and 10mg of oral ketorolac every 6hours in case of pain. The patients also took a hydrophilic laxative (psyllium), dissolving one tablespoon of the laxative in a glass of water at night. They had a high-fiber diet and drank 8 glasses of water a day. They sat to the side to avoid placing direct support on the area of the surgical intervention.
A complete postoperative proctologic examination was performed (inspection, palpation, digital rectal examination, and anoscopy) on the patients weekly for 6 weeks, and the wounds were considered healed when they presented with complete epithelialization, which was documented through clinical photographs of the patients, taken with a digital camera. The study was conducted according to the principles of the Declaration of Helsinki.
The statistical analysis of the results was carried out using the Statistical Package for the Social Sciences (SPSS) version 25.0. The nonparametric Mann-Whitney U test was used to compare the two patient groups and confirm their comparability. The Student's t test was employed to compare the means of the healing times between the two groups, as independent samples, and to determine whether there were statistically significant differences.
ResultsThe mean age of the control group patients was 47.61 years and 47.57 years for the diltiazem group patients. There was no statistically significant difference in relation to age between the two groups (p = 0.657; 95% confidence interval [CI]). In the control group, 11 patients were women and 15 were men. In the diltiazem group, 14 of the patients were women and 12 were men. There were no significant differences with respect to sex between the two groups (p = 0.317; 95% CI) (Mann-Whitney U test).
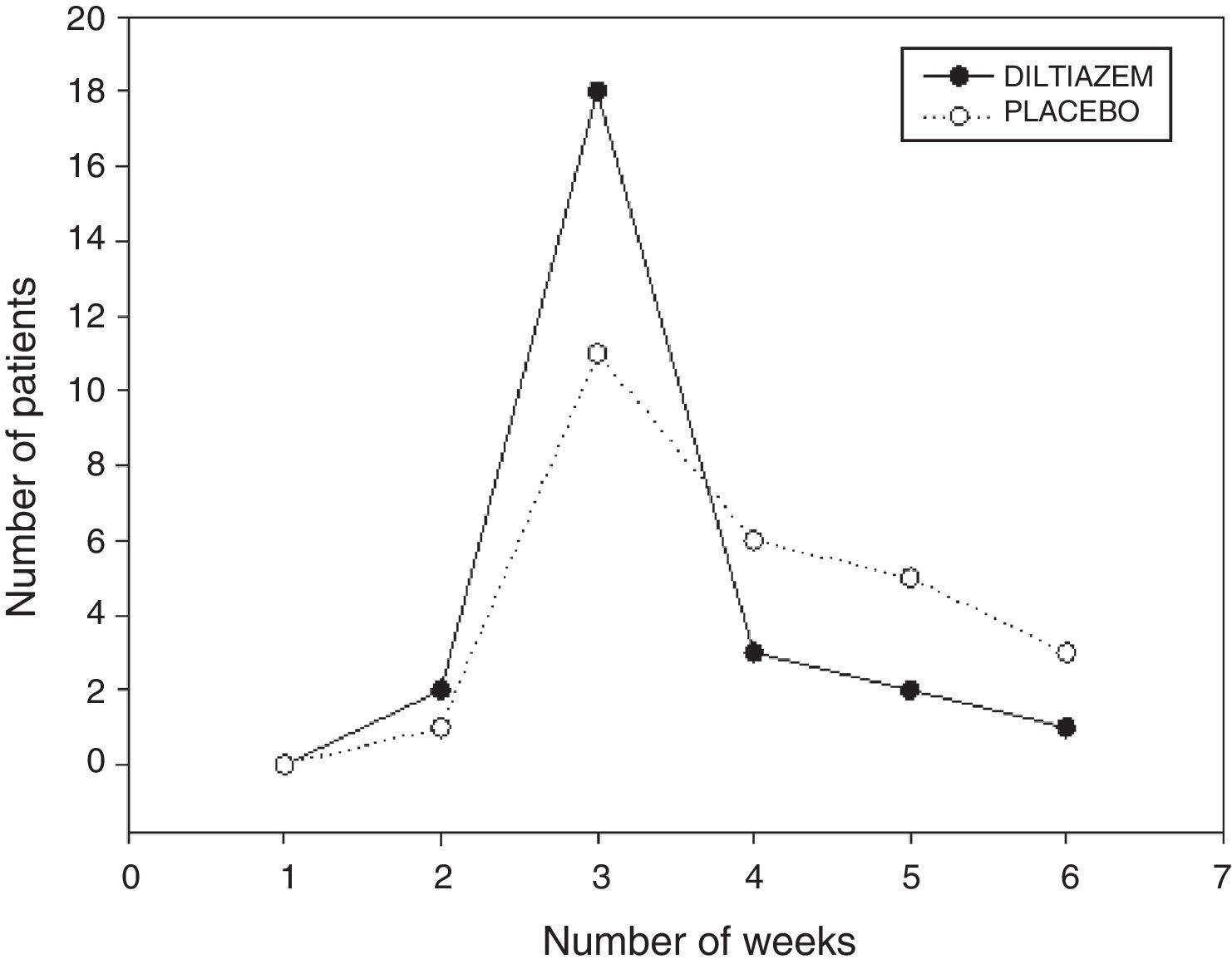
None of the patients were considered healed at the first week of evaluation. At the second week, one patient in the control group and two patients in the diltiazem group presented with cicatrization. At the third week, the wounds in 11 control group patients and 18 diltiazem group patients were healed, at the fourth week, cicatrization was observed in 6 patients in the control group and 3 patients in the diltiazem group, and at the fifth week, the wounds in 5 control group patients and in 2 diltiazem patients were healed. At the sixth week, 3 patients in the control group and one patient in the diltiazem group presented with cicatrization.
Mean healing time was 3.92 weeks (27.44 days) for the control group and 3.19 weeks (22.33 days) for the group treated with diltiazem. At the third week, the wounds in 46.15% of the control group patients had healed, compared with 73.07% of the patients treated with diltiazem (fig. 1).
The statistical analysis between the two groups was carried out using the Student's t test, resulting in a p = 0.012 with a 95% CI.
Only one patient in the group treated with diltiazem presented with anal pruritus at the fifth week of application of the medication. There were no other side effects in either group.
DiscussionThe internal anal sphincter has a calcium-dependent mechanism to maintain tone, in addition to possessing extrinsic cholinergic inhibitory innervation. Calcium antagonists have a relaxation effect on the internal anal sphincter.5 On the other hand, the increase in the resting pressure of the anal sphincter produces a decrease in blood flow, which reduces the capacity to heal.6
Topical diltiazem reduces the maximum resting pressure of the anal sphincter. In one study,3 diltiazem gel at 2% reduced the maximum resting pressure of the anal sphincter by 28%, with no additional effect at greater concentrations of the gel. Topical diltiazem is more efficacious than oral diltiazem for decreasing maximum resting pressure of the internal anal sphincter.7
In another study,8 topical nitroglycerin at 2% was used to improve healing after hemorrhoidectomy. The surgical wound cicatrization rate in the group treated with nitroglycerin was 74.5% at postoperative week 3, compared with 42% in the control group (p= 0.002). We obtained very similar results in our patients with the use of topical diltiazem.
Wound healing was reported at 42.5% in a study9 on postoperative hemorrhoidectomy patients at three weeks after the procedure that were treated with nitroglycerin at 0.2%, compared with 19.04% of the patients in the control group.
In a more recent study1 on patients that underwent hemorrhoidectomy, the group treated with nitroglycerin had a higher cicatrization rate (76.7%) at the end of the third week, compared with the control group (46.7%). In a meta-analysis10 on postoperative hemorrhoidectomy patients, healing time was reduced in the patients treated with topical nitroglycerin.
Botulinum toxin has also been reported to reduce healing time after hemorrhoidectomy. Cicatrization time in one study2 was shorter (23.8 ± 4.1 days) in patients that received botulinum toxin, compared with patients that were given a placebo (31.3 ± 5.5 days) (p < 0.05). In our study, the mean healing time in the group treated with diltiazem was 22.3 days, compared with 27.44 days in the control group.
In the present study, topical diltiazem at 2%, applied in the postoperative period after closed hemorrhoidectomy, was statistically significant in reducing surgical wound healing time.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of dataThe authors declare that they have followed the protocols of their work center on the publication of patient data.
Right to privacy and informed consentThe authors declare that no patient data appear in this article.
Financial disclosureNo specific grants were received from public sector agencies, the business sector, or non-profit organizations in relation to this study.
Conflict of interestThe authors declare that there is no conflict of interest.
Please cite this article as: Rodríguez-Wong U, Rodríguez-Medina U, Medina-Murillo GR. Ensayo clínico aleatorizado con diltiazem tópico para la cicatrización de heridas posthemorroidectomía. Revista de Gastroenterología de México. 2019;84:119–122.